See other cases
Endoscopic ampulectomy
We present the case of a 60 year-old female patient, with no previous medical history, who presented for jaundice with a recent onset, that was in remission at the time of evaluation.
Clinically, the patient had upper right quadrant pain. The clinical examination was unremarkable. Biologically, anicteric cholestasis and mild liver cytolysis were detected.
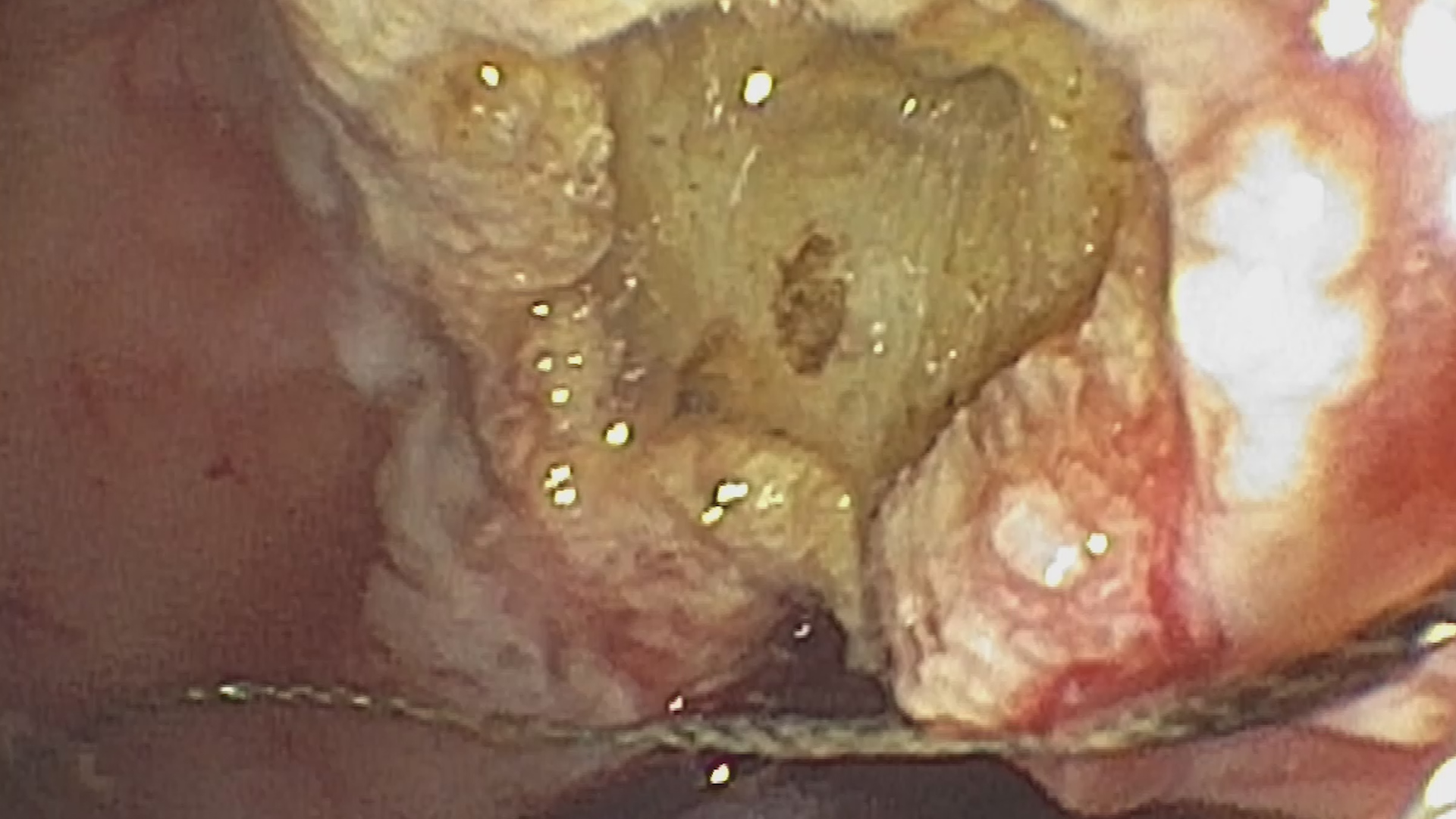
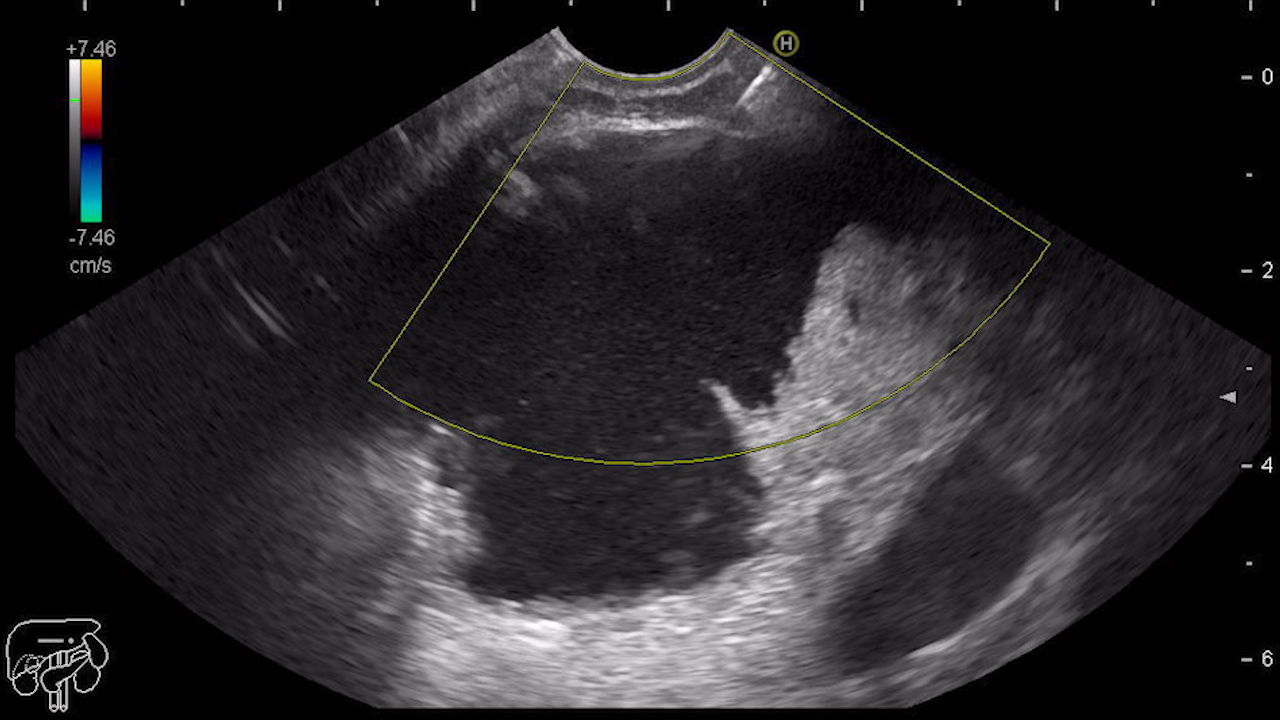
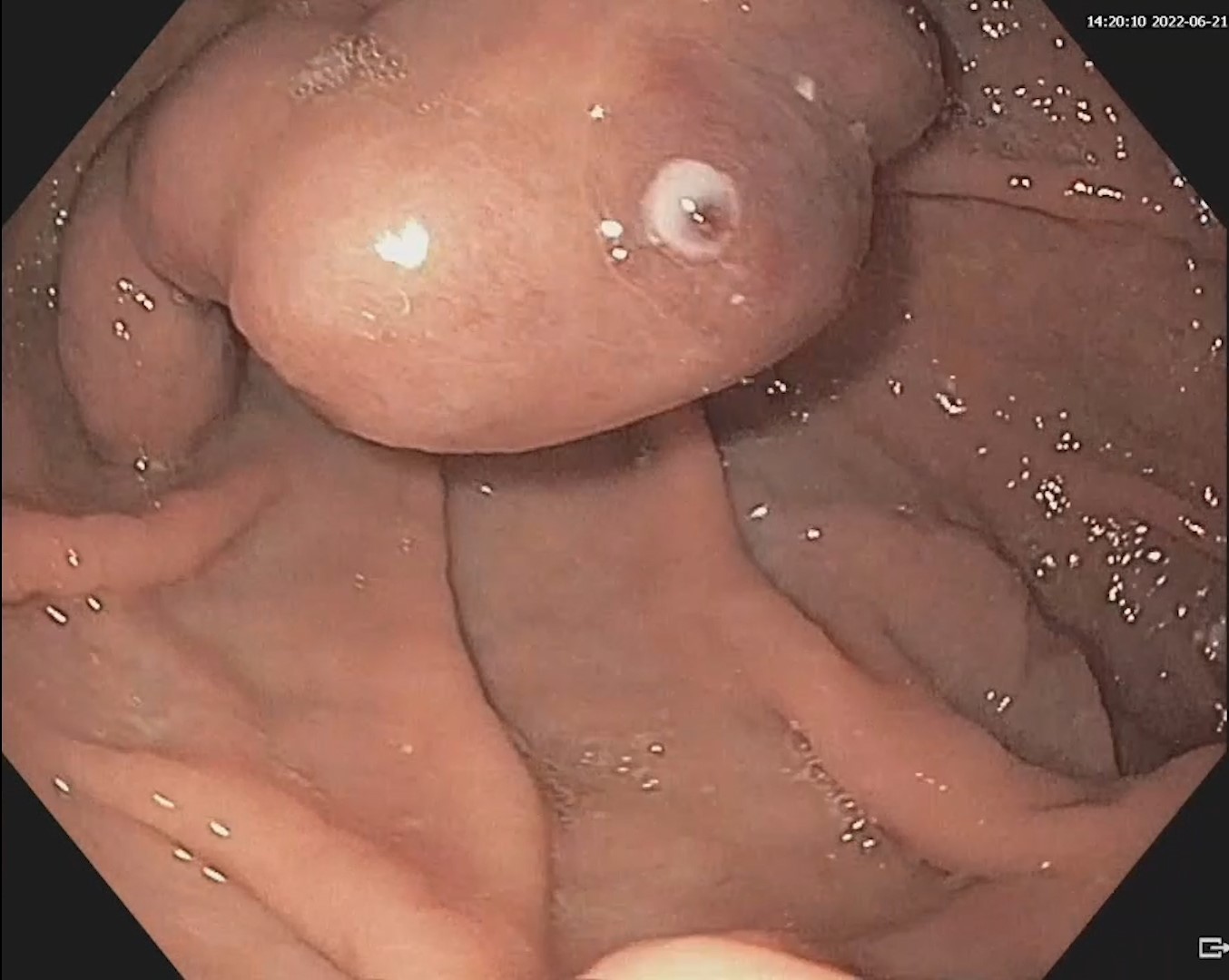
Both abdominal ultrasound and CT examination of the abdomen with intravenous contrast medium showed global distension of the biliary tree, without identifying the etiology. Upper digestive endoscopy performed with the duodenoscope revealed a lateral spreading lesion with a nodular component (Paris IIA+IS) measuring 25/30 mm (Figure 1), with a regular surface and microvascular pattern in the NBI mode examination, located at the level of the papillary region. The endoscopic biopsies and histopathological exam revealed a tubulo-villous adenoma with low-grade dysplasia, which was confirmed by a second set of biopsies. Endoscopic ultrasound indicated the absence of intraductal extension; submucosal invasion and malignant-looking lymph nodes were also absent.
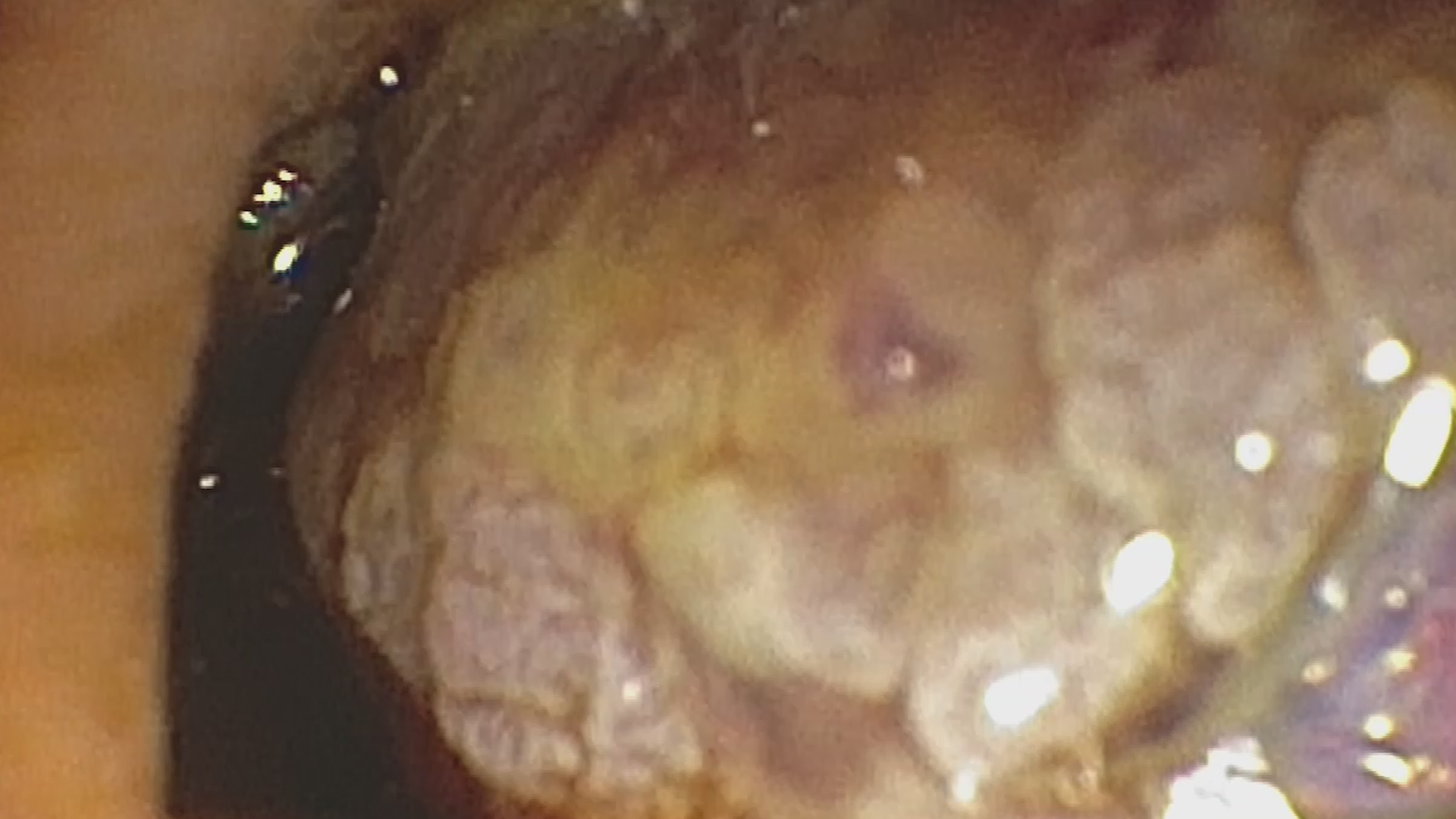
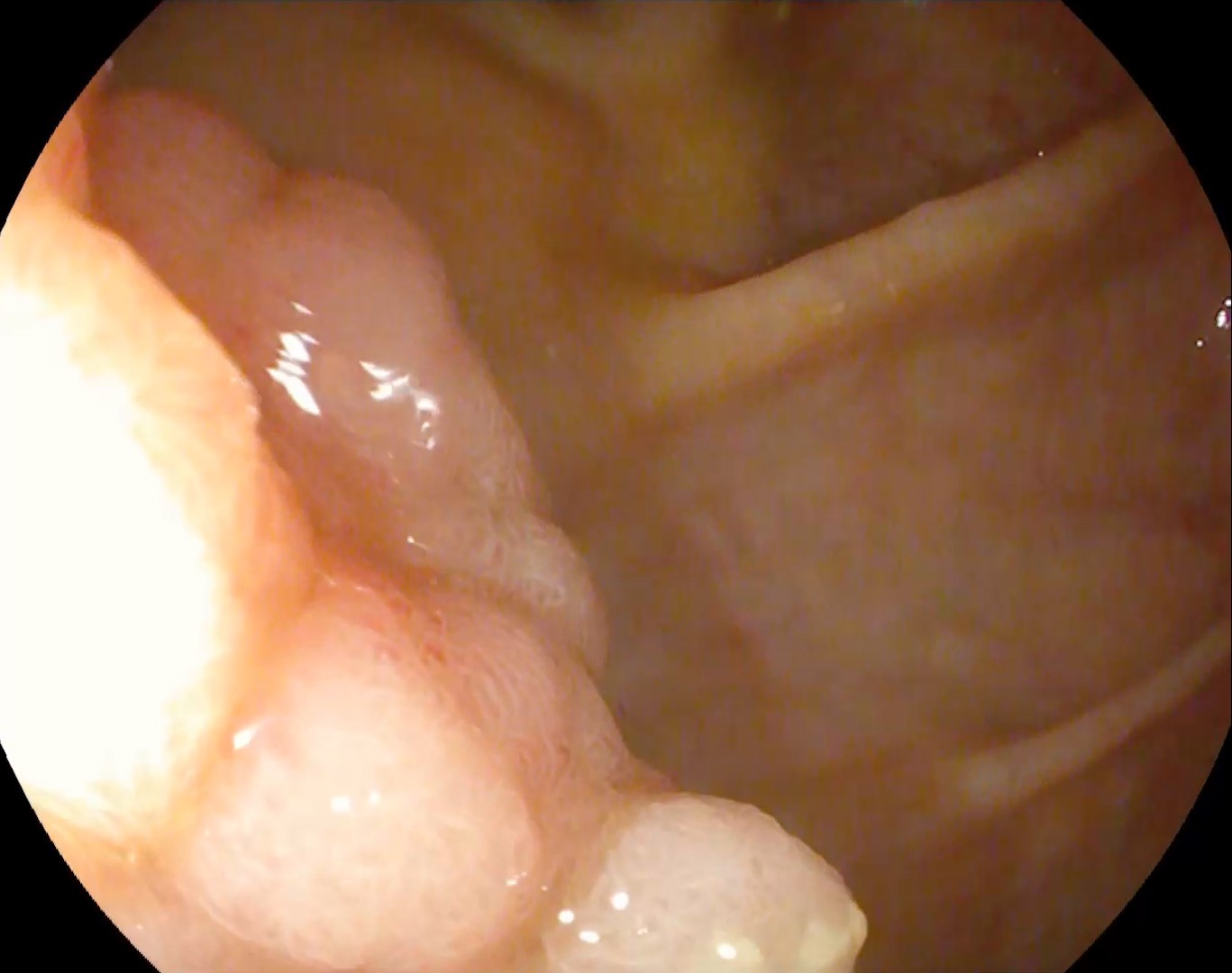
Endoscopic ampullectomy with a 25 mm loop was performed (Figure 2-4, Video 1) with subsequent placement of a pancreatic stent for the prophylaxis of acute pancreatitis. Histopathological examination of the resection specimen revealed tubulo-villous adenoma with low-grade dysplasia, with free lateral and deep margins. The endoscopic evaluation at 3 months, which included biopsies from the resection scar, showed no signs of local recurrence.
Ampullary adenoma – endoscopic ampullectomy.
Ampullary adenomas are premalignant lesions that develop at the level of the ampulla of Vater. The diagnostic workup usually begins with an abdominal ultrasound, when the patient presents for the investigation of jaundice. Definitive diagnosis requires upper digestive endoscopy and biopsies, followed by assessment of the intraductal extension by endoscopic ultrasound or MRCP. Although there are no universally accepted criteria, virtual chromoendoscopy can help identify signs suggestive of malignancy and deep submucosal invasion.
For ampullary adenomas, the guidelines recommend endoscopic ampullectomy for lesions up to 30 mm with intraductal invasion of less than 20 mm as a first treatment option. If the lesion does not exceed the papillary region, the resection is performed without submucosal injection as the ampullary region is fixed by the muscle layer. If the lesion extends beyond the ampulla, submucosal injection and elevation of the extrapapillary component is required. Retrieval of the piece is essential in order to confirm a complete resection and must be done quickly as intestinal motility can lead to loss of the specimen.
Prophylaxis of acute pancreatitis is mandatory due to an increased risk of occurrence in this setting; it is carried out by general measures (intrarectal NSAIDs, intravenous hydration) and pancreatic duct stenting. Biliary stenting is not routinely recommended; it should be performed in case of bleeding, perforation or cholangitis.
Ampullary adenomas are rare lesions, with an increasing prevalence in recent years due to easy access to endoscopic examinations and superior imaging modalities. Although they are benign lesions, resection is recommended due to the risk of malignant transformation. The clinical case presented emphasizes the fact that endoscopic ampullectomy is a safe and effective minimally invasive method of treatment of ampullary adenomas that meet the eligibility criteria for endoscopic treatment.
- Vanbiervliet G, Strijker M, Arvanitakis M et al. Endoscopic management of ampullary tumors: European Society of Gastrointestinal Endoscopy (ESGE) Guideline. Endoscopy 2021;53(4):429-448
- Patel R, Varadarajulu S, Wilcox CM. Endoscopic ampullectomy: techniques and outcomes. J Clin Gastroenterol. 2012 Jan;46(1):8-15
- Itoi T, Ryozawa S, Katanuma A et al. Clinical practice guidelines for endoscopic papillectomy. Dig Endosc. 2022;34(3):394-411.