See other “How to”
How to do WOPN drainage
How to do Endoscopic Ultrasound (EUS) guided Walled-Off Pancreatic Necrosis (WOPN) drainage and Direct Endoscopic Necrosectomy (DEN)
Walled-Off Pancreatic Necrosis (WOPN) is a late complication of acute necrotizing pancreatitis, characterized by the encapsulation of necrotic pancreatic and peripancreatic tissue within a well-defined fibrous wall. This process typically occurs at least 4 weeks after the onset of pancreatitis, as the body attempts to contain and isolate areas of necrosis.
Pathogenesis of WOPN
- Initial Inflammatory Phase: During acute pancreatitis, pancreatic enzyme activation leads to autodigestion, resulting in necrosis of pancreatic and surrounding tissues.
- Necrosis and Liquefaction: Over time, the necrotic tissue undergoes liquefaction due to enzymatic breakdown and the inflammatory response.
- Encapsulation: A fibrous capsule gradually forms around the necrotic material, resulting in the formation of a walled-off collection. Unlike pseudocysts, WOPN contains a mixture of solid necrotic debris and fluid, making its management more complex.
Clinical Significance
WOPN can lead to significant morbidity due to its potential to:
- Become infected, resulting in sepsis or abscess formation.
- Compress adjacent structures such as the stomach, duodenum, or bile ducts, causing obstructive symptoms.
- Cause persistent pain, gastrointestinal bleeding, or systemic inflammation if left untreated.
Indications for Intervention
Not all WOPN cases require intervention. Treatment is generally indicated in the following scenarios, usually when WOPN is symptomatic:
- Compression: Persistent pain, nausea, vomiting, or early satiety due to mass effect.
- Infection: Signs of infected WOPN, such as fever, leukocytosis, or bacteremia, confirmed by imaging and microbiological analysis.
- Complications: Hemorrhage, biliary obstruction, or gastric outlet obstruction.
The development of lumen-apposing metal stents (LAMS) has revolutionized the management of WOPN, allowing for minimally invasive drainage and necrosectomy under endoscopic ultrasound (EUS) guidance. This approach provides direct access to the necrotic cavity, enabling efficient drainage and debridement with a lower risk of complications compared to surgical or percutaneous methods.
This step-by-step guide details the procedure for EUS-guided necrosectomy using hot LAMS in a patient with symptomatic WOPN secondary to severe acute necrotic-hemorrhagic pancreatitis.
Step 1. Pre-procedure Preparation
1. Patient Selection and Assessment
- Confirm WOPN diagnosis with contrast-enhanced CT or MRI.
- Ensure the presence of a symptomatic, mature WOPN (at least 4 weeks from onset with defined walls).
- Evaluate for complications like infection, biliary obstruction, or vascular involvement.
- Optimize the patient’s coagulation profile and manage comorbidities.
2. Equipment Preparation
- Hot LAMS stent system (e.g., HotAxios or HotSpaxus).
- EUS endoscope with color Doppler capability.
- Irrigation and suction systems for necrosectomy.
- Accessories: snares, biopsy forceps, baskets, or nets for debris removal.
3. Sedation and Patient Positioning
- Administer general anesthesia or deep sedation.
- Position the patient in the left lateral decubitus position.
Step 2. Endoscopic Ultrasound-Guided Access
1. Visualization of the WOPN
- Introduce the EUS endoscope into the stomach or duodenum.
- Identify the WOPN and confirm proximity to the gastric or duodenal wall.
- Use color Doppler to avoid vascular structures.
2. Access Point Selection
- Choose a puncture site with the shortest distance to the WOPN.
- Confirm the presence of necrotic material and fluid content in the cavity.
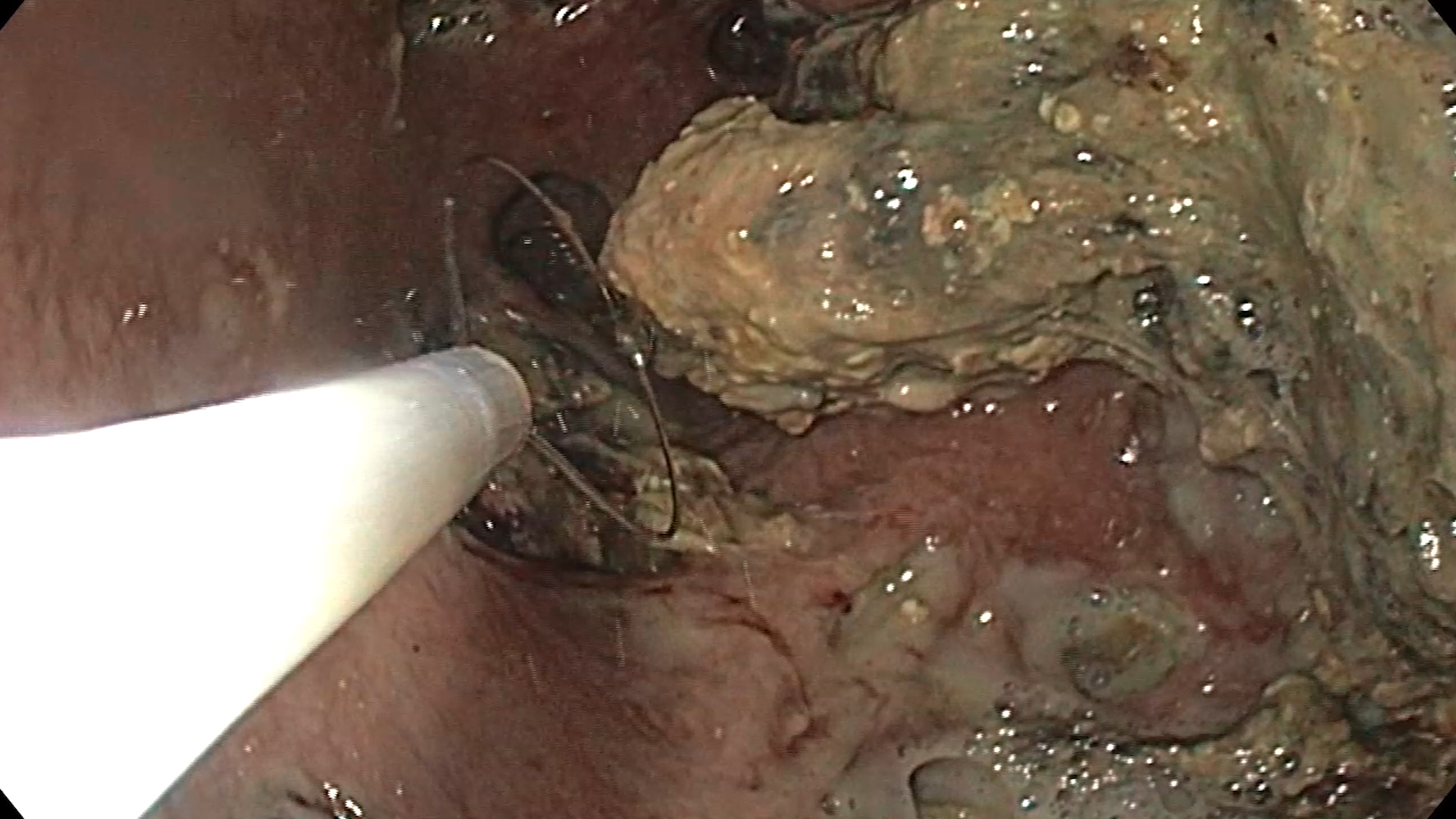
3. Cystotomy with Hot LAMS
- Advance the hot LAMS delivery catheter under EUS guidance.
- Deploy the first flange within the WOPN, ensuring it expands fully.
- Pull back gently and deploy the second flange against the gastric/duodenal wall.
- Confirm placement with endoscopy and EUS.
Step 3. Cavity Irrigation and Initial Debridement
1. Establish Cavity Drainage
- Flush the cavity with saline to evacuate loose necrotic material and pus.
- Collect samples for microbiology and cytology if infection is suspected.
2. Monitor Clinical Response
- Place a nasocystic tube for continuous lavage if extensive infection is present.
- Allow 48–72 hours for drainage and cavity maturation before necrosectomy.
Step 4. Endoscopic Necrosectomy
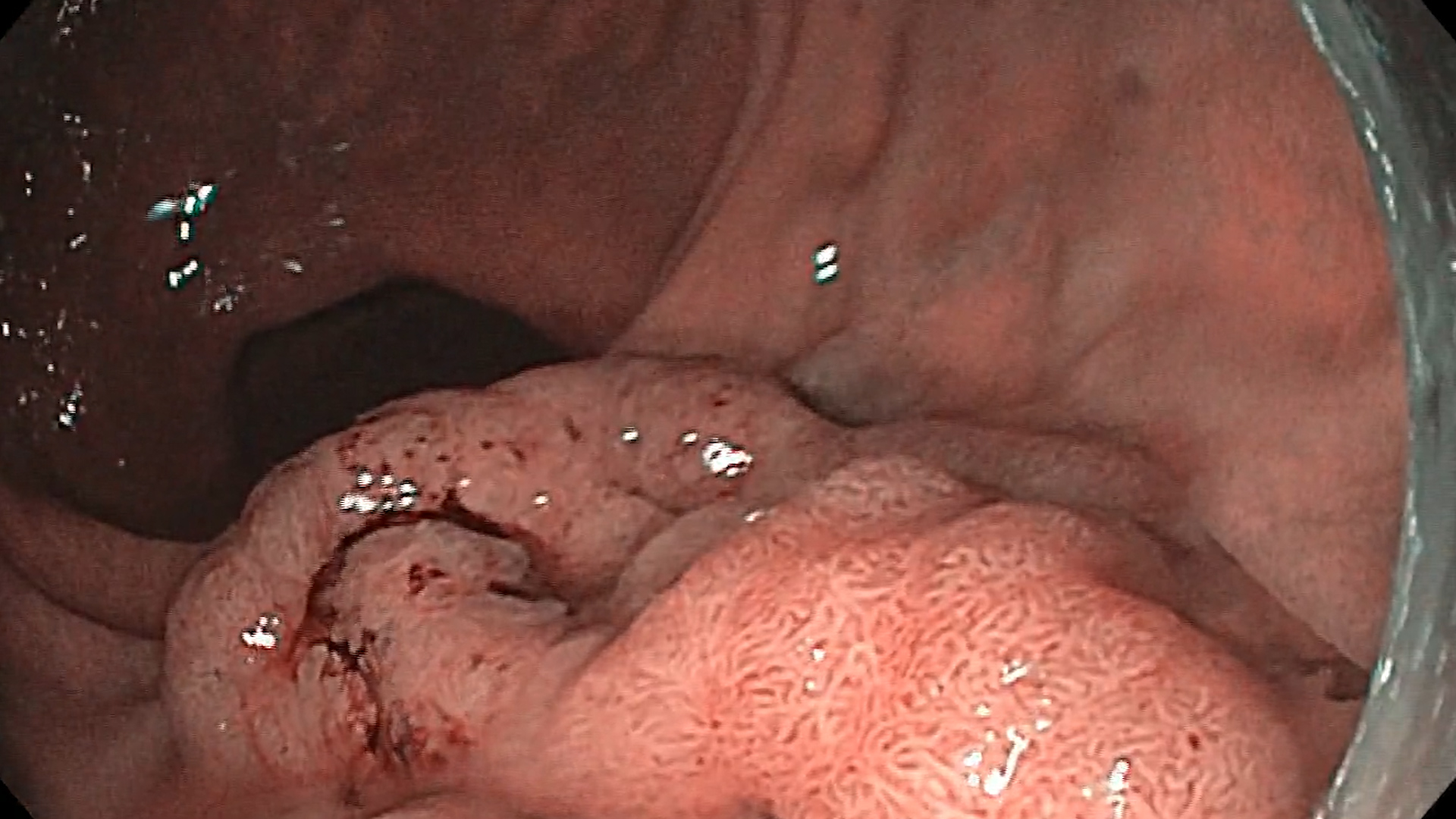
1. Re-access the Cavity
- Insert a therapeutic endoscope through the LAMS stent into the WOPN.
- Perform necrosectomy in sequential sessions if required.
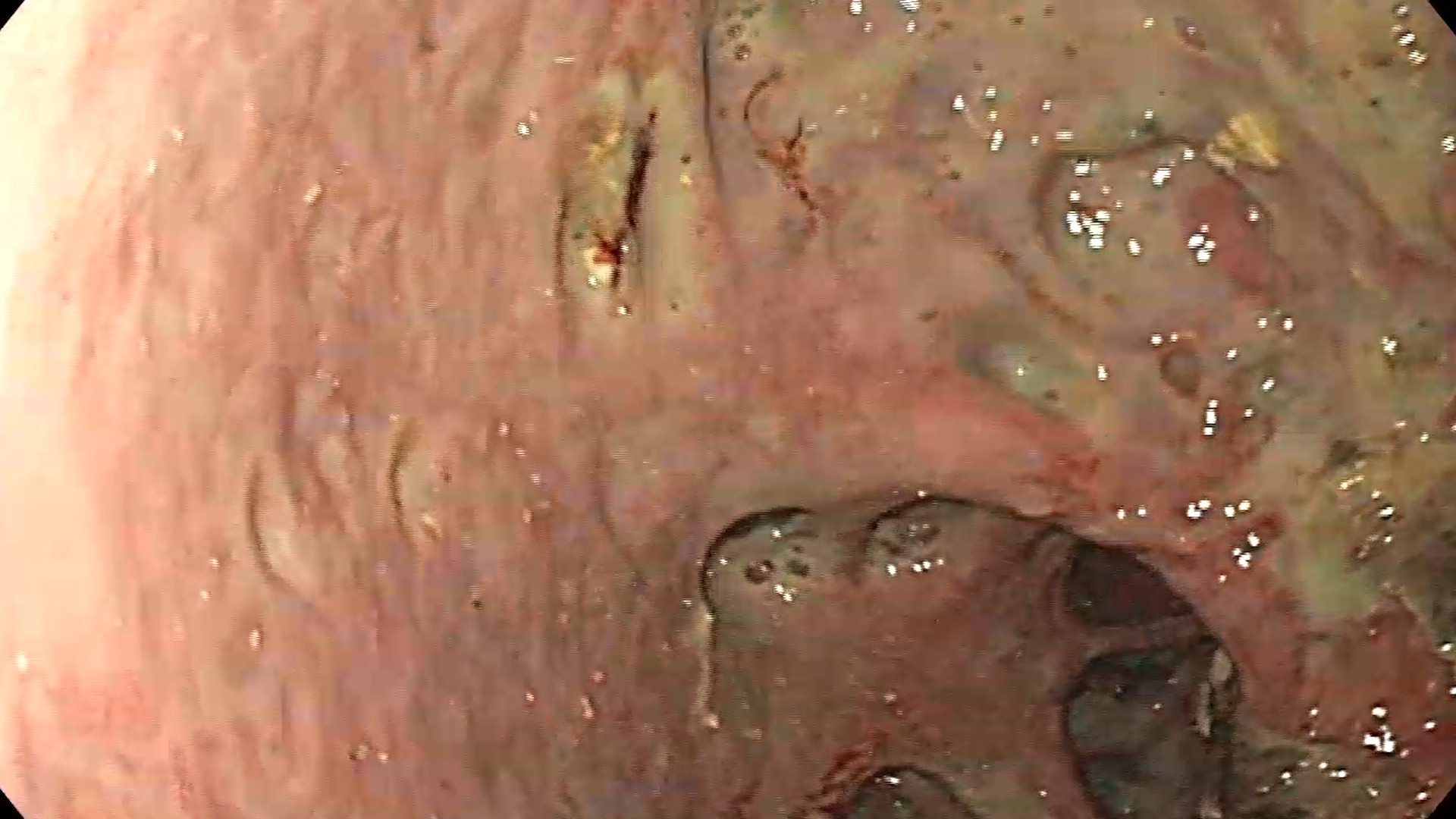
2. Debridement of Necrotic Tissue
- Use snares, forceps, and baskets to extract necrotic debris.
- Avoid aggressive maneuvers to prevent bleeding or perforation.
3. Cavity Irrigation
- Irrigate the cavity intermittently with sterile saline or diluted antibiotic solution.
- Use suction to clear fluid and residual debris.
4. Endoscopic Assessment
- Reassess the cavity after debridement for any remaining necrotic material.
- Confirm the absence of complications, such as bleeding or perforation.
Step 5. Post-procedure Care
1. Stent Maintenance
- Keep the LAMS in place for 2–4 weeks or until cavity resolution.
- Monitor the patient for fever, abdominal pain, or signs of stent blockage.
2. Imaging Follow-up
- Repeat CT or MRI after 2 weeks to assess cavity resolution.
3. Secondary Interventions
- Plan additional necrosectomy sessions if residual necrosis persists.
- Consider endoscopic or percutaneous drainage of adjacent collections, if necessary.
Step 6. Complications Management
1. Bleeding
- Apply hemostatic techniques (e.g., epinephrine injection, coagulation forceps).
- Consult interventional radiology for embolization if severe.
2. Infection
- Adjust antibiotic therapy based on microbiological results.
- Consider surgical debridement if the patient’s condition deteriorates.
3. Stent Migration or Blockage
- Replace the stent endoscopically if required.
Step 7. Final Stent Removal
- Perform LAMS stent removal endoscopically after resolution of the WOPN (it cannot be maintained more than 3-4 weeks).
- Place plastic stents in case of lack of resolution or presence of disconnected pancreatic duct syndrome (DPDS)
- Inspect the cavity to ensure complete resolution and absence of debris.
Conclusions
- In this case of biliary pancreatitis, address the biliary etiology (e.g., cholecystectomy or ERCP with biliary sphincterotomy and stone extraction) after the acute phase has resolved.
- Consider multidisciplinary management involving gastroenterologists, interventional radiologists, and surgeons.
References
- Kamal F, Khan MA, Lee-Smith W, Sharma S, Acharya A, Farooq U, Gangwani MK, Saeed A, Aziz M, Hayat U, Saleem N, Kumar A, Schlachterman A, Kowalski T. EUS-guided Drainage of Pancreatic Fluid Collections Using Lumen Apposing Metal Stents With or Without Coaxial Plastic Stents: A Systematic Review and Meta-analysis. J Clin Gastroenterol. 2025 Jan 1;59(1):47-53. doi: 10.1097/MCG.0000000000002080.
- Karstensen JG, Novovic S, Hansen EF, Jensen AB, Jorgensen HL, Lauritsen ML, Werge MP, Schmidt PN. EUS-guided drainage of large walled-off pancreatic necroses using plastic versus lumen-apposing metal stents: a single-centre randomised controlled trial. Gut 2023; 72(6): 1167-1173. doi: 10.1136/gutjnl-2022-328225.
- Boxhoorn L, Verdonk RC, Besselink MG, Boermeester M, Bollen TL, Bouwense SA, Cappendijk VC, Curvers WL, Dejong CH, van Dijk SM, van Dullemen HM, van Eijck CH, van Geenen EJ, Hadithi M, Hazen WL, Honkoop P, van Hooft JE, Jacobs MA, Kievits JE, Kop MP, Kouw E, Kuiken SD, Ledeboer M, Nieuwenhuijs VB, Perk LE, Poley JW, Quispel R, de Ridder RJ, van Santvoort HC, Sperna Weiland CJ, Stommel MW, Timmerhuis HC, Witteman BJ, Umans DS, Venneman NG, Vleggaar FP, van Wanrooij RL, Bruno MJ, Fockens P, Voermans RP; Dutch Pancreatitis Study Group. Comparison of lumen-apposing metal stents versus double-pigtail plastic stents for infected necrotising pancreatitis. Gut 2023; 72(1): 66-72. doi: 10.1136/gutjnl-2021-325632.