See other “How to”
How to do my first ESD? Tips and tricks.
Whenever your endoscopy journey leads you to more advanced luminal endoscopy procedures, you should try and follow technical advices that assist in having a smooth procedure and uneventful recovery for patients with large polypoid lesions. Performing endoscopic submucosal dissection (ESD) in the rectum requires a high level of expertise and attention to specific technical details to ensure both effectiveness and safety. Here are some tips and tricks for performing ESD in the rectum:
- Pre-Procedure Preparation:
Experience and Training: ESD in the rectum is technically challenging. Ensure adequate training and practice on animal models or under the supervision of experienced endoscopists before attempting on patients.
Teamwork: Work closely with an experienced endoscopy team, including nurses and anesthesiologists, to ensure patient safety and effective management of potential complications.
Patient Preparation: Ensure the bowel is adequately prepared to provide clear visualization. A complete bowel cleanse is necessary.
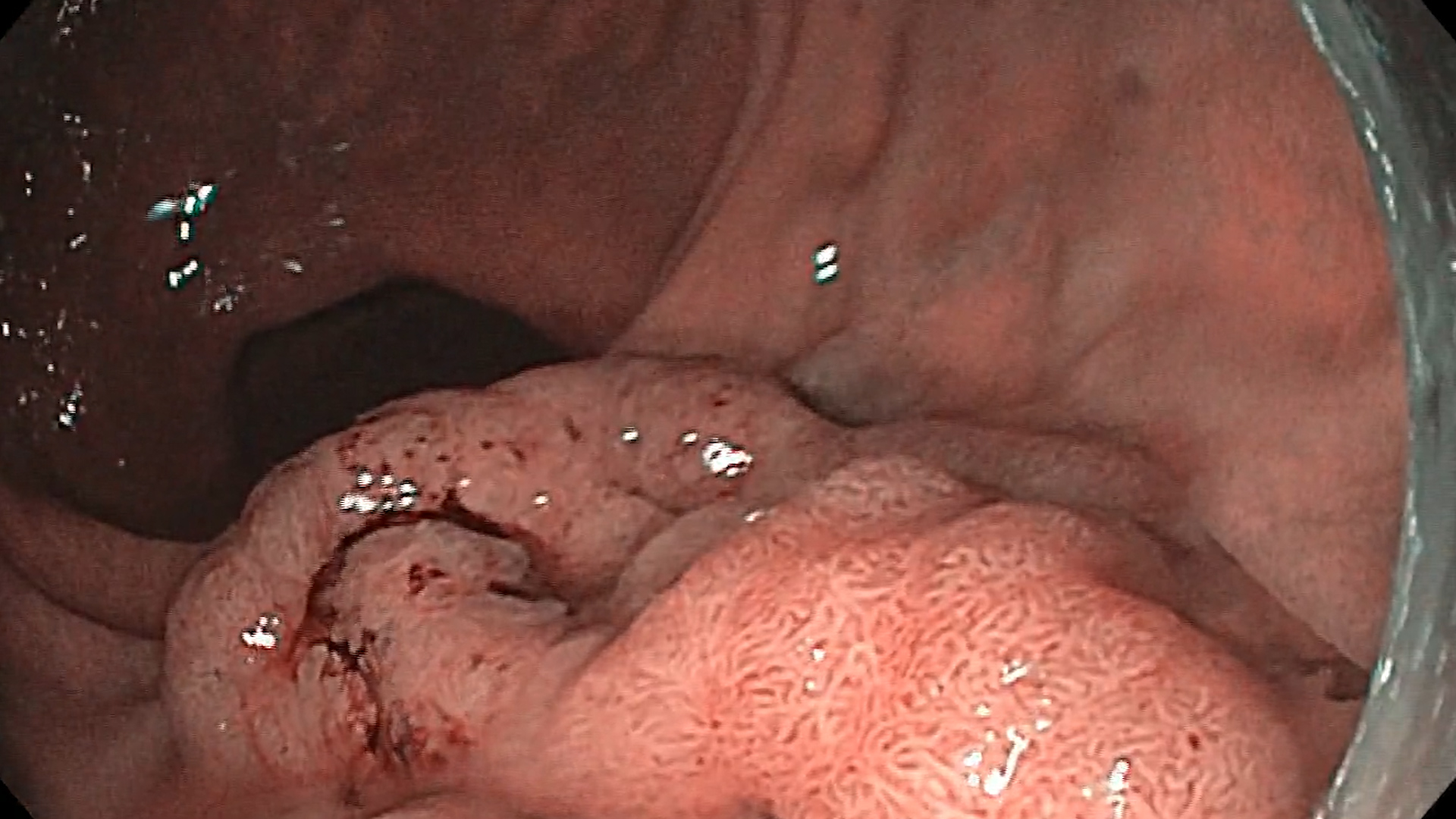
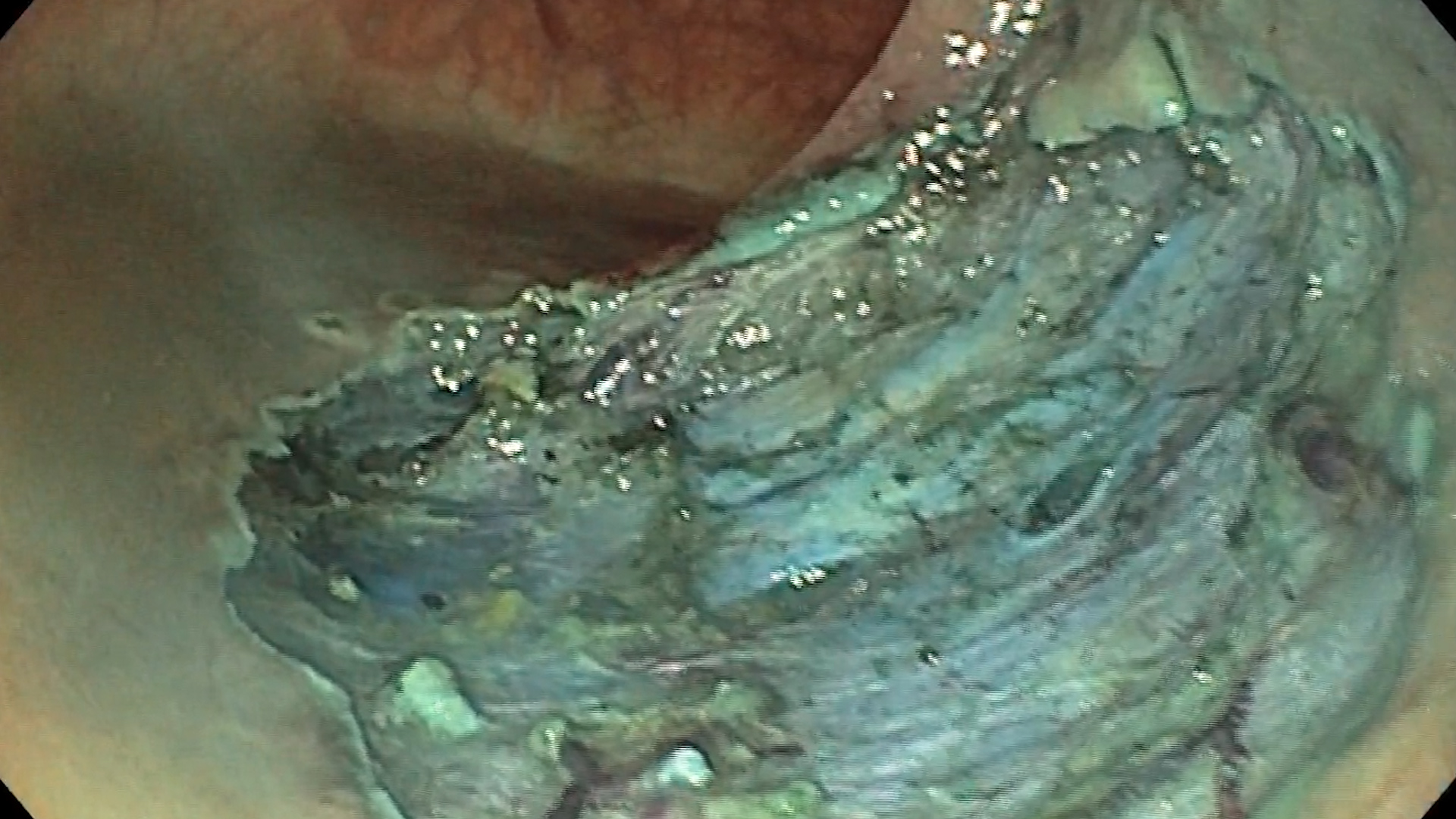
Lesion Assessment: Thoroughly assess the lesion with high-definition white-light endoscopy and chromoendoscopy to determine the boundaries and depth of invasion. Use magnification and narrow-band imaging (NBI) if available (Fig. 1).
Lesion staging: The lesions should be staged prior to the intervention with magnetic resonance imaging (MRI) and endoscopic ultrasound (EUS) in order to assess resectability and allow a proper discussion in a multidisciplinary setting (gastroenterology, surgery, oncology, pathology).
Equipment Selection: Use a high-definition endoscope with a water jet. Ensure you have all necessary accessories, including different types of knives (e.g., DualKnife, HookKnife, or ITKnife), hemostatic forceps, and injection needles.
- Procedure Technique:
Marking the Lesion: Use a soft coagulation mode to mark the periphery of the lesion about 5 mm from the edge. This helps in delineating the area for dissection.
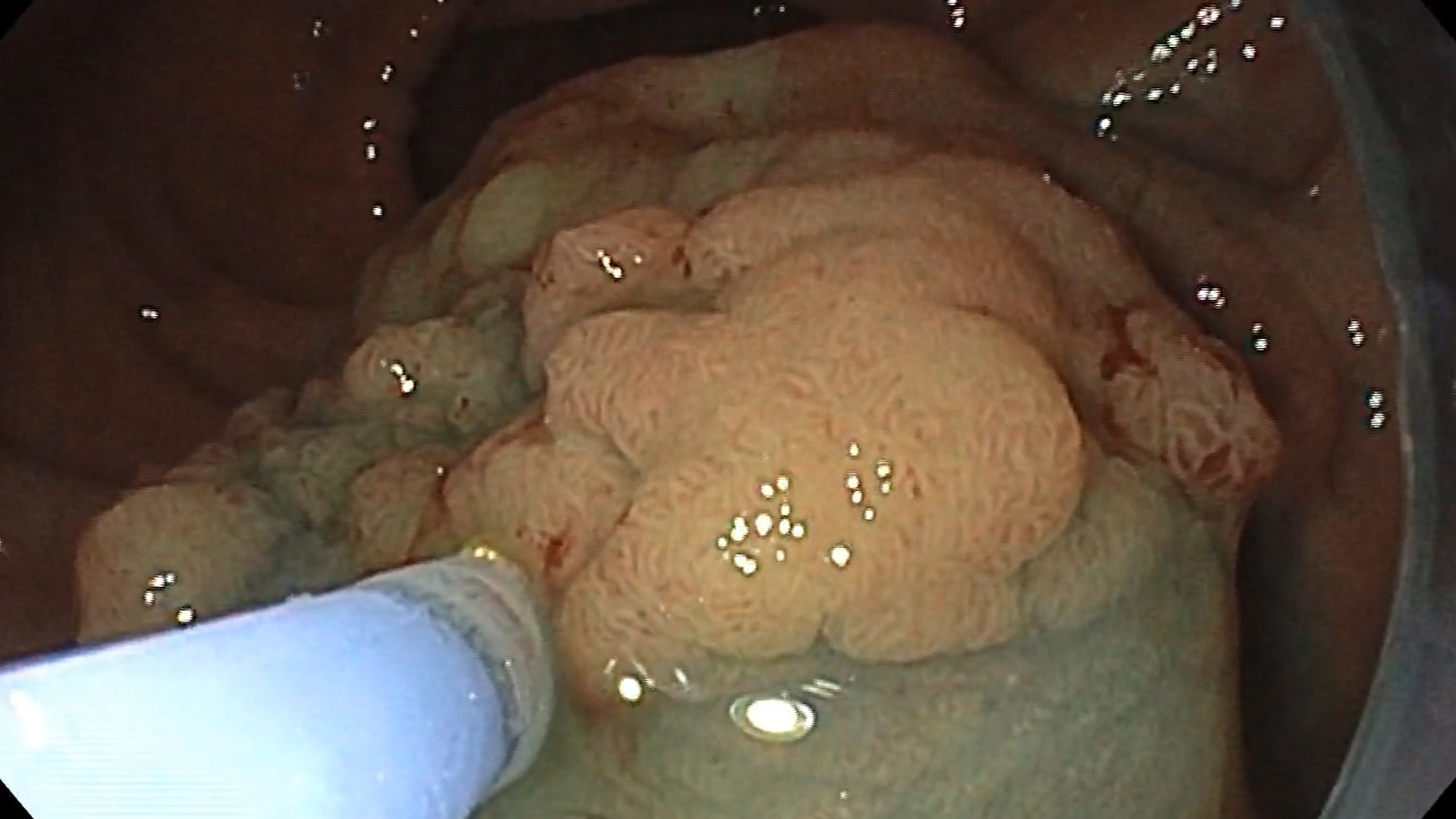
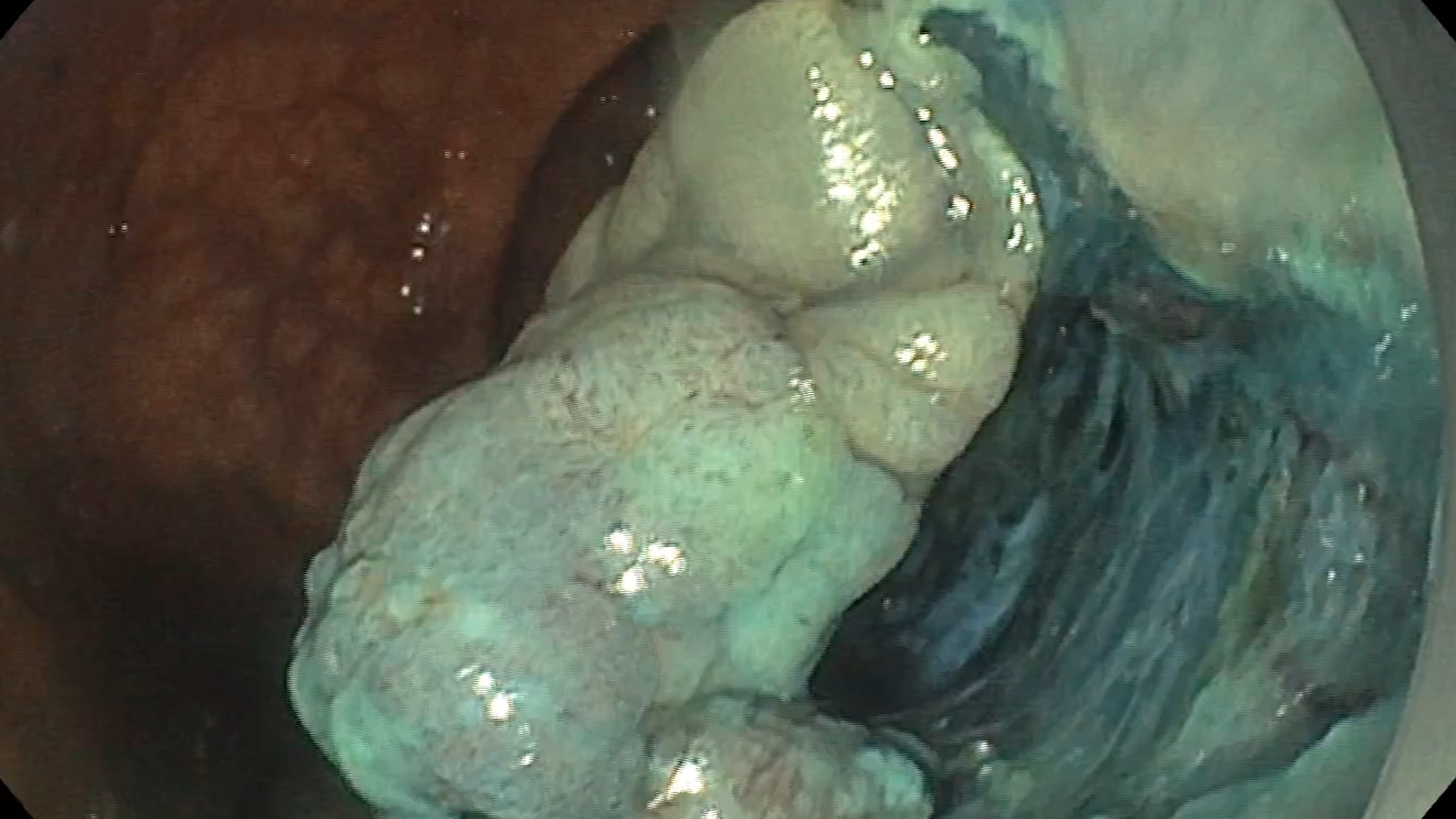
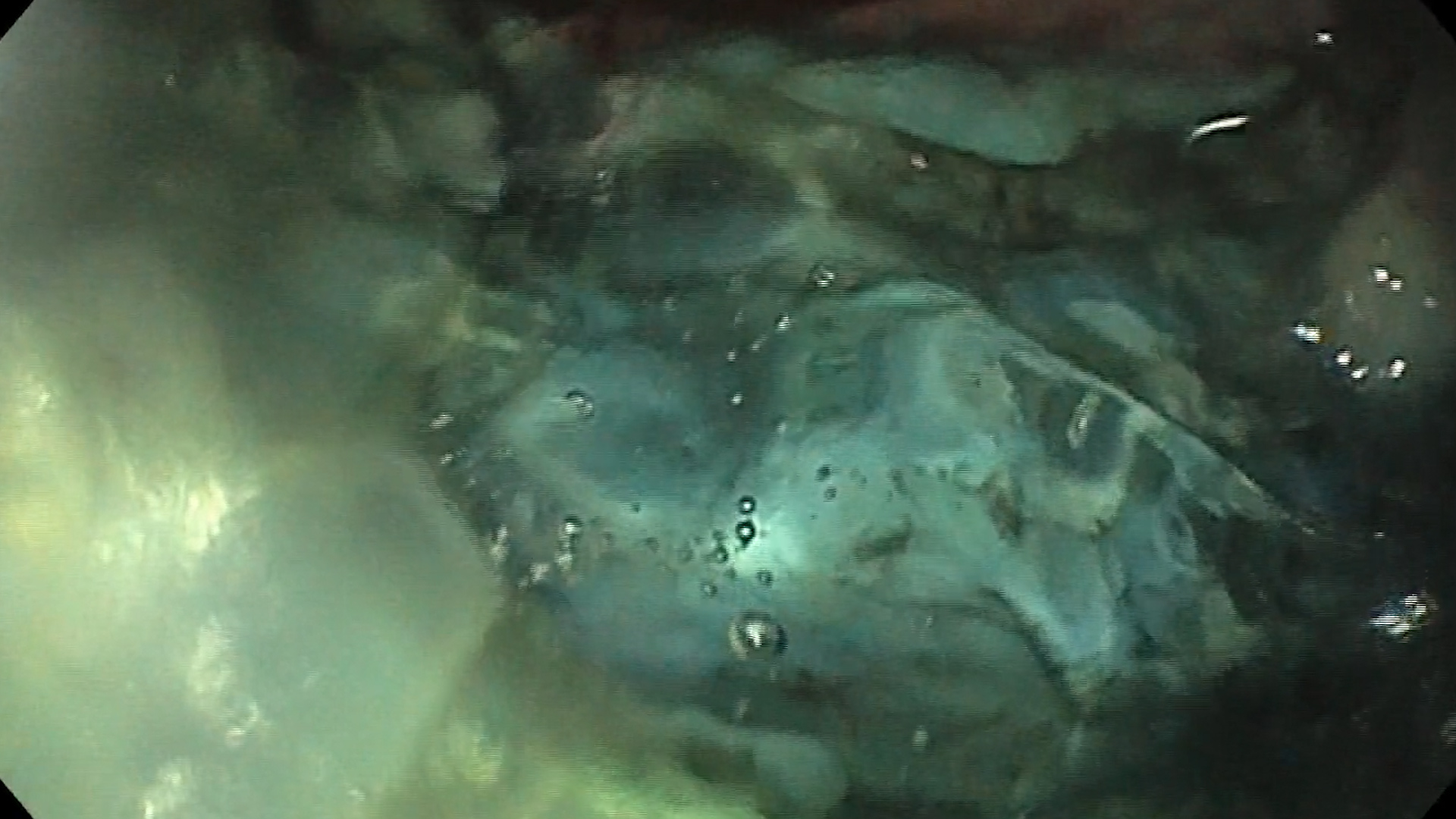
Injection Solution: Inject a solution (e.g., saline or succinylated gelatin with a small amount of epinephrine and a blue dye such as indigo carmine or methylene blue) into the submucosal layer to lift the lesion (Fig. 2). This creates a safe cushion for dissection.
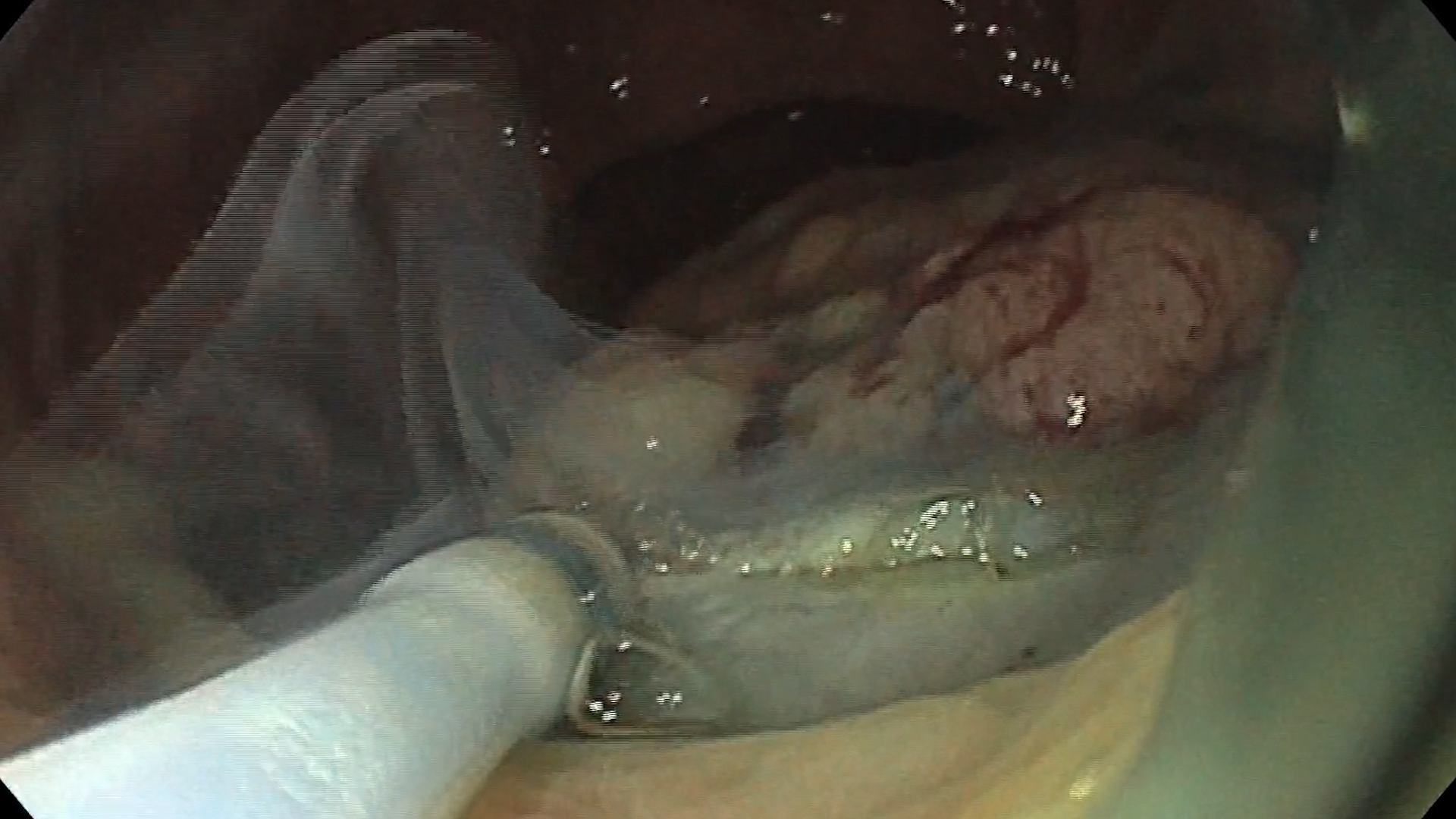
Initial Incision: Make a distal incision around the marked area using an appropriate ESD knife and then the proximal incision that delimitates the end of the tunnel. Start with a small incision to access the submucosal layer and then extend it (Fig. 3).
Submucosal Dissection: Carefully dissect the submucosal layer (Fig. 4). Use a combination of cutting and coagulating current to avoid bleeding. Maintain a clear view of the submucosal plane, and continuously inject the lifting solution to keep the area elevated.
Tunneling Technique: In some cases, creating a submucosal tunnel under the lesion can help in maintaining a clear plane and reduce perforation risk:
- Distal Side First (Towards the Anal Verge): Resecting the distal side initially can help in maintaining better visualization and control (Fig. 5). This approach allows the endoscope to have a more stable position, and gravity can assist in keeping the pocket open.
- Proximal Side Next (Closest to the Proximal Colon): Opening the proximal side in retroversion ensures that you maintain good traction and visibility throughout the procedure, knowing where exactly to end the submucosal dissection (Fig. 6).
- Lateral Sides (Antigravitational and Gravitational) Last: After the distal side is resected, moving to the lateral sides allows for the creation of a larger working space within the pocket (Fig. 7).
Pocket creation: when performing ESD using the pocket-creation method (PCM) in the rectum (Fig. 8), the sequence of resection can influence the ease and safety of the procedure, with a step-by-step approach. Using saline immersion therapeutic endoscopy (SITE) might be also useful to create a better resection plane that can prevent the lesion from collapsing into the pocket, which would make the dissection more challenging.
Countertraction: Use techniques such as clip-with-line or clip-and-snare methods to create countertraction, improving visibility and access to the submucosal layer.
Bleeding Control: Anticipate and manage bleeding promptly. Use hemostatic forceps to coagulate any visible vessels during dissection. Specific settings for electrocautery like DryCut (circumferential cutting) and SwiftCoag (submucosal dissection) help tremendously to reduce intraprocedural bleeding.
Preemptive Coagulation: Coagulate larger submucosal vessels before cutting to prevent significant bleeding. A coag-grasper or a larger hot biopsy forceps reduce the risk of bleeding.
- Post-Procedure Care:
Inspection: After resection, carefully inspect the resection bed for any signs of bleeding or perforation (Fig. 9). Coagulate any visible vessels.
Hemostatic gels: Purastat® (3-D Matrix Ltd, Tokyo, Japan) can be used after large rectal ESDs, to enhance hemostasis by forming a 3D protective barrier and support faster healing and a smooth recovery (Fig. 10).
Closure: Consider prophylactic closure of the mucosal defect with endoclips if the resection area is large or if there’s a high risk of delayed perforation or bleeding.
Post-Procedure Monitoring: Monitor the patient for any signs of complications such as bleeding, perforation, or infection. Provide appropriate post-procedure care and follow-up.
Follow-up: It is decided based on full pathology results, most probably after 3-6 months (Fig. 11).
By following these tips and maintaining a meticulous approach, you can enhance the success rate and safety of rectal ESD procedures.
References:
- Yamamoto H, Hayashi Y, Despott EJ. The pocket-creation method for endoscopic submucosal dissection combined with saline-immersion: another potential option to overcome challenges in colorectal endoscopic submucosal dissection. Gastrointest Endosc. 2019 Aug;90(2):288-289. doi: 10.1016/j.gie.2019.04.244.
- Mavrogenis G, Ntourakis D, Wang Z, Tsevgas I, Zachariadis D, Kokolas N, Kaklamanis L, Bazerbachi F. The learning experience for endoscopic submucosal dissection in a non-academic western hospital: a single operator’s untutored, prevalence-based approach. Ann Gastroenterol. 2021 Nov-Dec;34(6):836-844. doi: 10.20524/aog.2021.0649.
- Tantau M, Tantau A, Mosteanu O, Pop T, Mester G, Pascu O. Endoscopic submucosal dissection of superficial digestive tumors after evaluation through magnification chromoendoscopy and endoscopic ultrasound with miniprobes. Report of three cases. J Gastrointestin Liver Dis. 2011 Mar;20(1):89-92.
- Pimentel-Nunes P, Libânio D, Bastiaansen BAJ, Bhandari P, Bisschops R, Bourke MJ, Esposito G, Lemmers A, Maselli R, Messmann H, Pech O, Pioche M, Vieth M, Weusten BLAM, van Hooft JE, Deprez PH, Dinis-Ribeiro M. Endoscopic submucosal dissection for superficial gastrointestinal lesions: European Society of Gastrointestinal Endoscopy (ESGE) Guideline – Update 2022. Endoscopy. 2022 Jun;54(6):591-622. doi: 10.1055/a-1811-7025.
- Libânio D, Pimentel-Nunes P, Bastiaansen B, Bisschops R, Bourke MJ, Deprez PH, Esposito G, Lemmers A, Leclercq P, Maselli R, Messmann H, Pech O, Pioche M, Vieth M, Weusten BLAM, Fuccio L, Bhandari P, Dinis-Ribeiro M. Endoscopic submucosal dissection techniques and technology: European Society of Gastrointestinal Endoscopy (ESGE) Technical Review. Endoscopy. 2023 Apr;55(4):361-389. doi: 10.1055/a-2031-0874.