See other cases
You gonna get it with patience
A 75-year-old female patient with multiple cardiovascular comorbidities: class IV NYHA heart failure, mitral stenosis with insufficiency, greatly dilated left atrium (10cm), permanent atrial fibrillation for which she is undergoing coumarinic anticoagulant treatment, aortic stenosis, and high BP. Over one year, she presented three episodes of digestive bleeding externalized as haematochezia with severe anemic syndrome (hemoglobin down to 5.4g/dl).
Clinically: fatigue, pale skin, dyspnea.
Biologically: severe hypochromic, microcytic anemia (hemoglobin 5.4g/dl); INR 2.25.
After volume re-equilibration (2 transfusion units and colloidal solutions), the patient’s condition improved, and she was hemodynamically stable for investigations.
First episode (08.2022):
> Upper GI Endoscopy: esophageal diverticulum, no hemorrhagic lesions.
> Lower GI Endoscopy: ulceration at the cecum level, hemostasis by adrenalinated serum injection 1/10000.
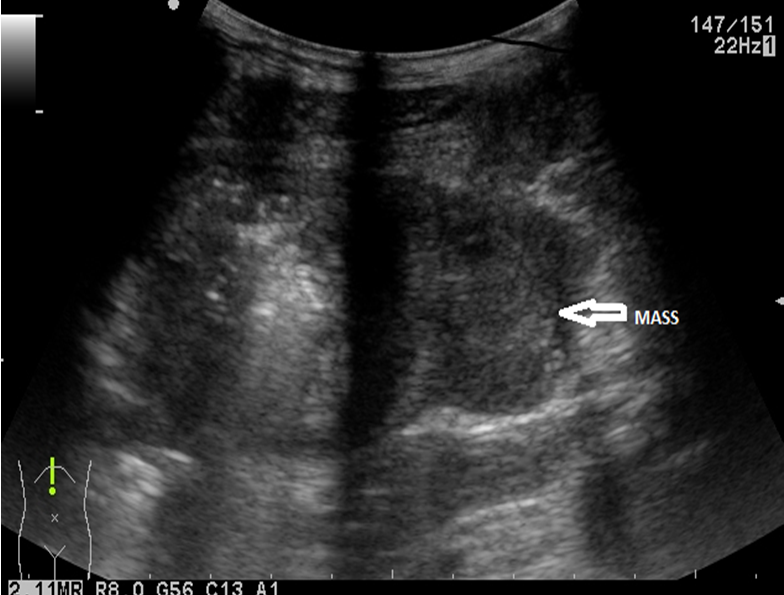
> Abdominal CT: rectal thickening – without endoscopic correspondence.
> EnteroCT: no abnormalities.
> AngioCT: no contrast extravasation.
Second episode (08.2023)
> Upper and Lower GI Endoscopy: no hemorrhagic lesions.
Third episode (10.2023)
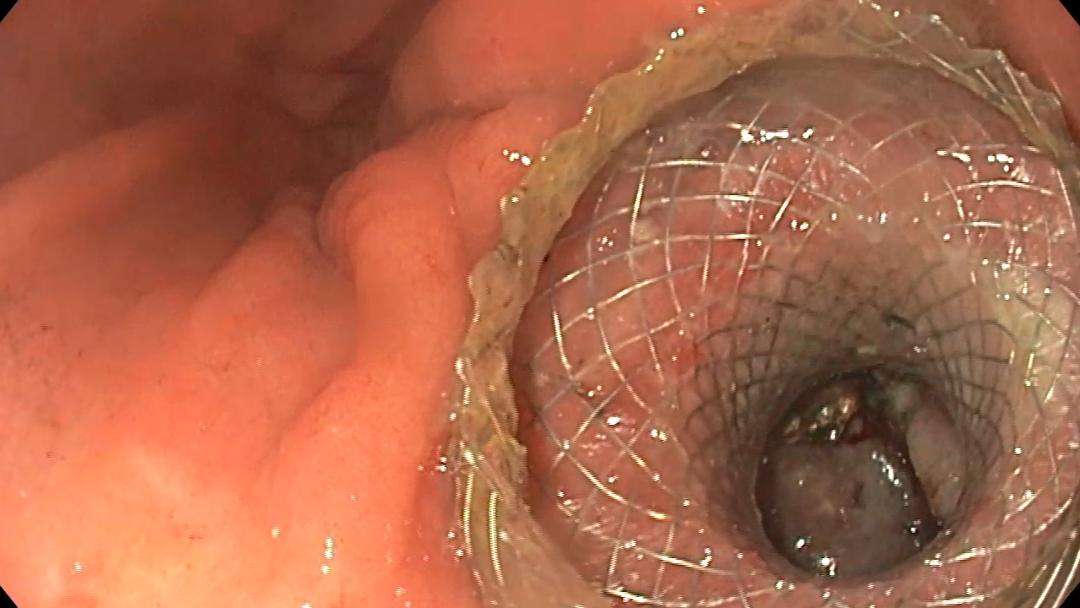
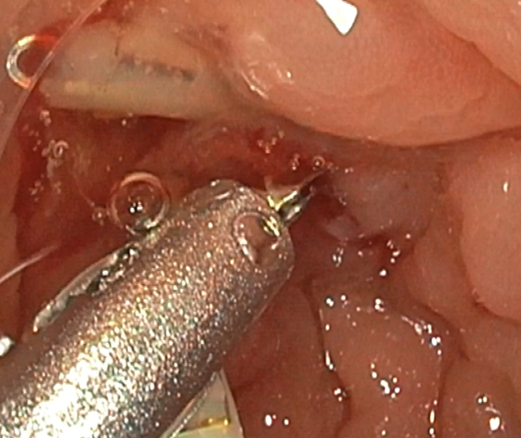
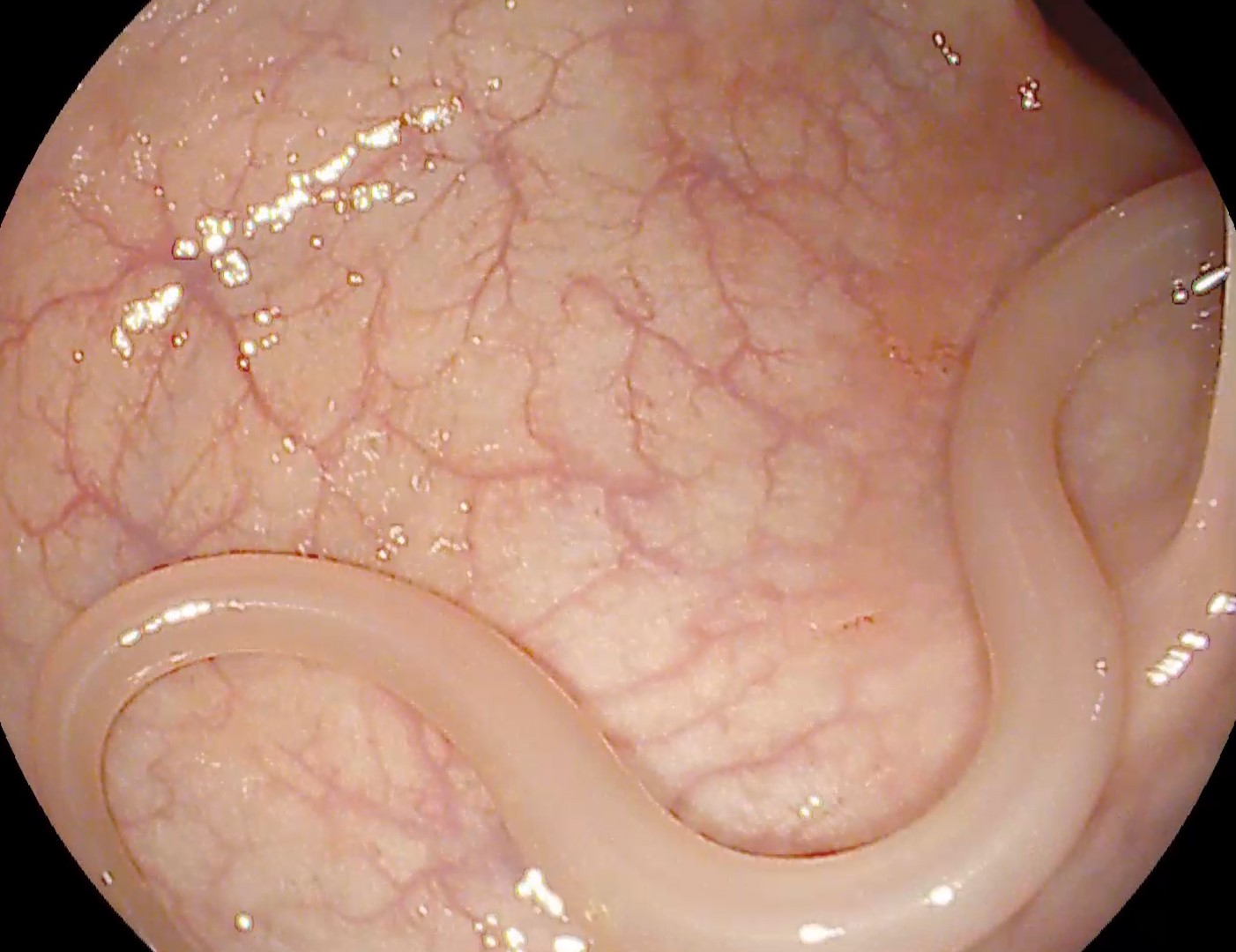
> Lower GI Endoscopy: fresh red blood coating the mucosa from the ascending colon and cecum; the colon was examined with an endoscopic cap for better visualization, including retroversion of the right colon, without detecting a source; repetitive lavage with active bleeding was observed from the colonic wall, three folds away from the cecum – suggestive for a Dieulafoy lesion (Fig 1) – 3 hemostatic metal clips were applied: the first 16mm Lockado clip for lesion localization between the folds and the following two Olympus clips achieved effective hemostasis (Fig 2).
Dieulafoy lesion of the ascending colon.
Considering the endoscopic features observed, the diagnosis of a Dieulafoy lesion was established. This lesion refers to a submucosal artery of significant size (1-3 mm in diameter) which maintains its caliber along its entire path, being about ten times larger than the maximal diameter of normal vessels that gradually decrease in size towards the periphery. The exact etiology remains unclear, but it is presumed that repetitive mechanical factors – such as the passage of the food bolus – or mucosal atrophy contribute to its erosion through a mucosal defect. When the artery erodes in this way, it can protrude into the lumen of the gastrointestinal tract, often leading to dramatic clinical presentations marked by hemodynamic instability and increased need for blood transfusions. Endoscopically, the typical appearance is that of a blood vessel without an associated ulcer or an adherent clot in the absence of an ulcer. When there are no signs of recent or active bleeding, the adjacent mucosa may appear unaffected. Dieulafoy’s lesion is identified in approximately 70% of cases in the stomach, on the lesser curvature, but it can also occur in other segments of the gastrointestinal tract, such as the duodenum, small intestine, and as observed in our case, the colon 1,2.
Currently, there is no clear consensus on the treatment of Dieulafoy’s lesion. Therapeutic endoscopy offers a variety of options for controlling hemorrhage, using methods such as electrocoagulation, application of clips via TTS technique or the OVESCO system, banding, or injection of fibrosing agents. In situations where the lesion is not endoscopically accessible or has not been identified, alternatives such as angiography, CT angiography, or nuclear imaging studies can be used. However, among these methods, only angiography also allows for direct therapeutic interventions. It is noteworthy that, in the case encountered in our clinic, CT angiography was chosen to locate the source of bleeding, but the attempt failed due to insufficient bleeding rate (a rate of over 0.35 ml/min is necessary for CT angiography) or because the bleeding was not active at the time of examination – a common feature in Dieulafoy’s lesions, known for their intermittent bleeding 3,4
- Mark Feldman, Lawrence Friendman. Chapter 20 Part III: Gastrointestinal Bleeding – Symptoms, Signs, and Biopsychosocial Issues. Sleisenger and Fordtrans’s Gastrointestinal and Liver Disease. Elsevier. 2020 – 11th edition. Page 295.
- Nojkov B, Cappell MS. Gastrointestinal bleeding from Dieulafoy’s lesion: Clinical presentation, endoscopic findings, and endoscopic therapy. World J Gastrointest Endosc. 2015; 7(4): 295-307.
- Baxter M, Aly EH. Dieulafoy’s lesion: current trends in diagnosis and management. Ann R Coll Surg Engl. 2010; 92(7): 548-54.
- Hacking C. Lower gastrointestinal bleeding (17.10.2023). https://radiopaedia.org/articles/lower-gastrointestinal-bleeding