See other cases
When esophageal tumors bleed, stents may be the last line of defense
A 63-year-old patient with a history of skin cancer and lymphoma, as well as severe associated cardiovascular conditions, was diagnosed with moderately differentiated adenocarcinoma of the esophagogastric junction (T3N0M0), previously treated with chemoradiotherapy. He presented with two episodes of hematemesis and worsening dysphagia. A surgically placed feeding gastrostomy tube had been inserted prior to this presentation.
Clinical – ECOG performance status of 2, afebrile, cachectic, with skin pallor; digital rectal examination revealed melena. The Rockall score was 8, primarily due to the extent of the malignant esophageal disease; the patient was hemodynamically stable.
Biology – Blood tests showed mild anemia, with a hemoglobin level of 10.4 g/dl, while platelet count, coagulation profile, liver and renal functions were within normal limits.
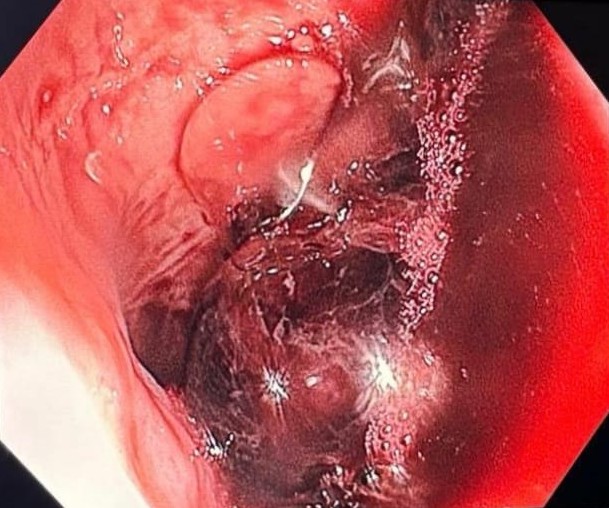
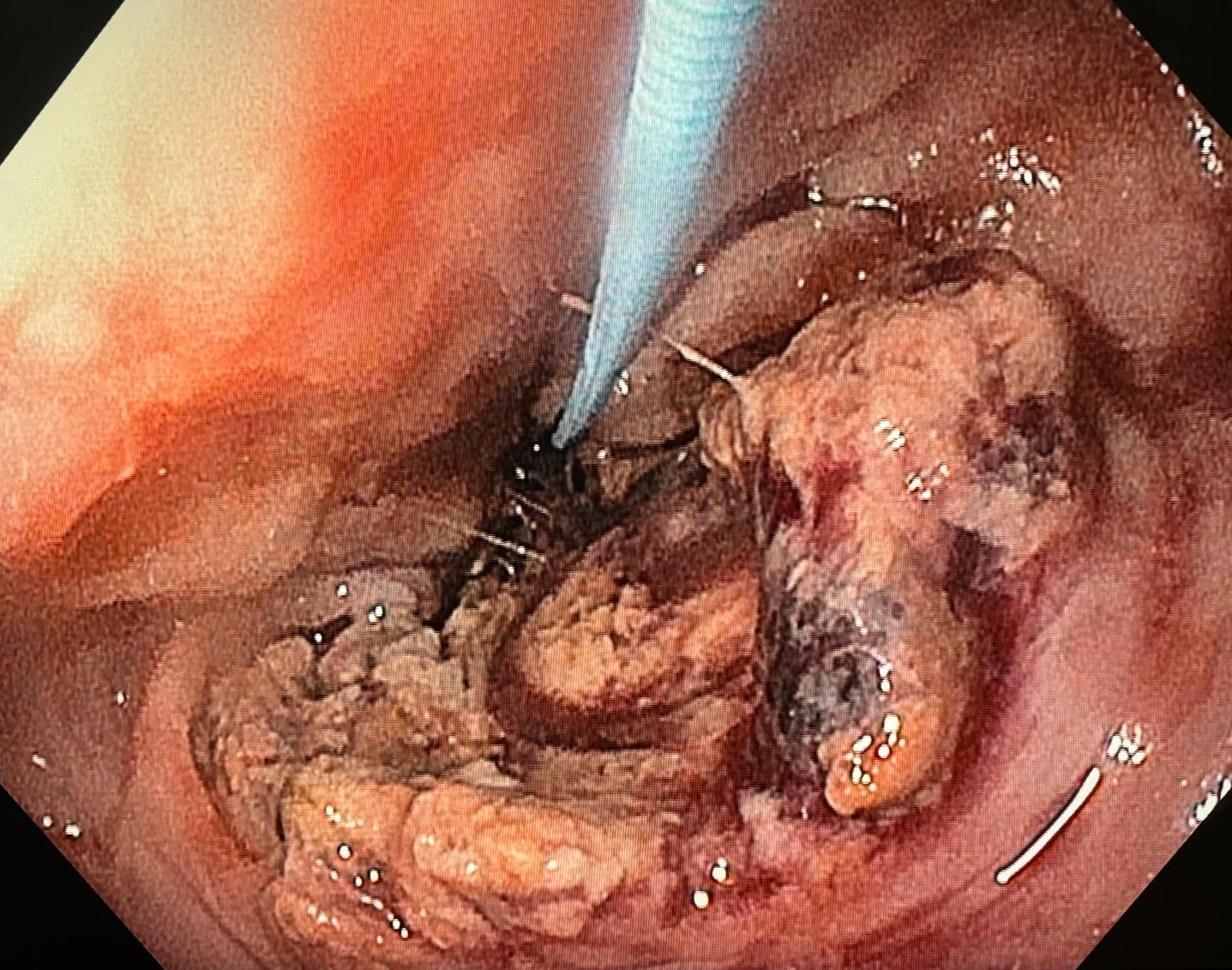
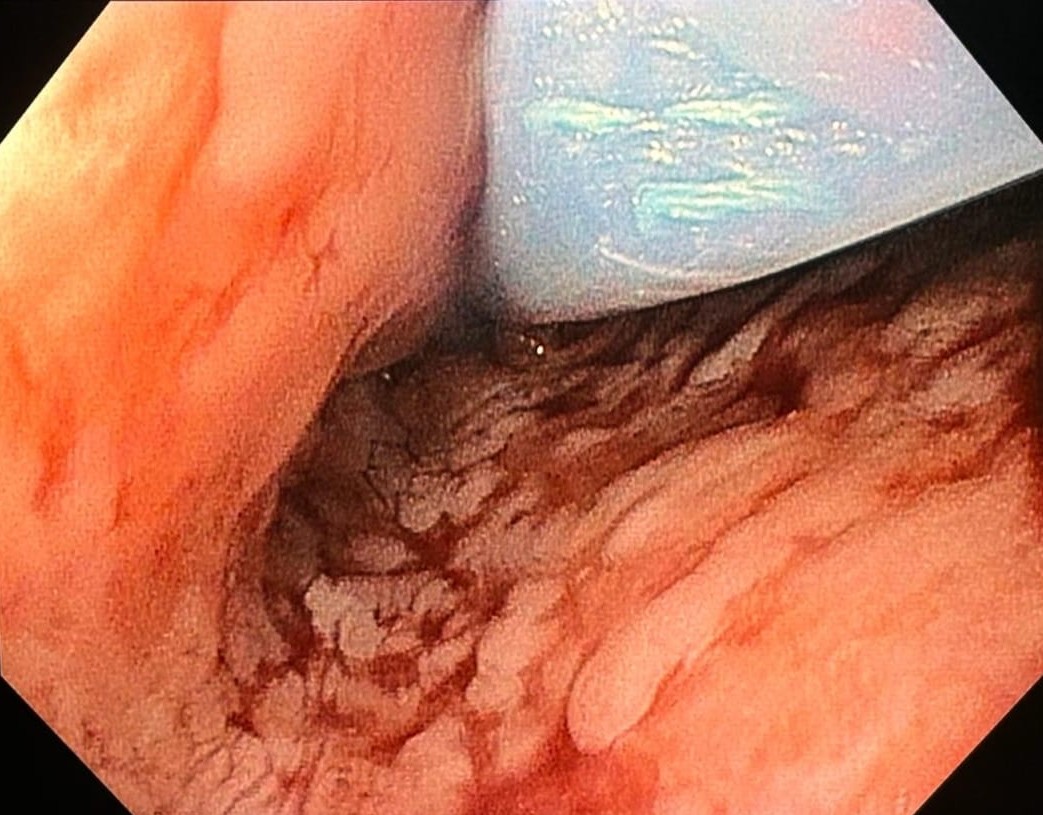
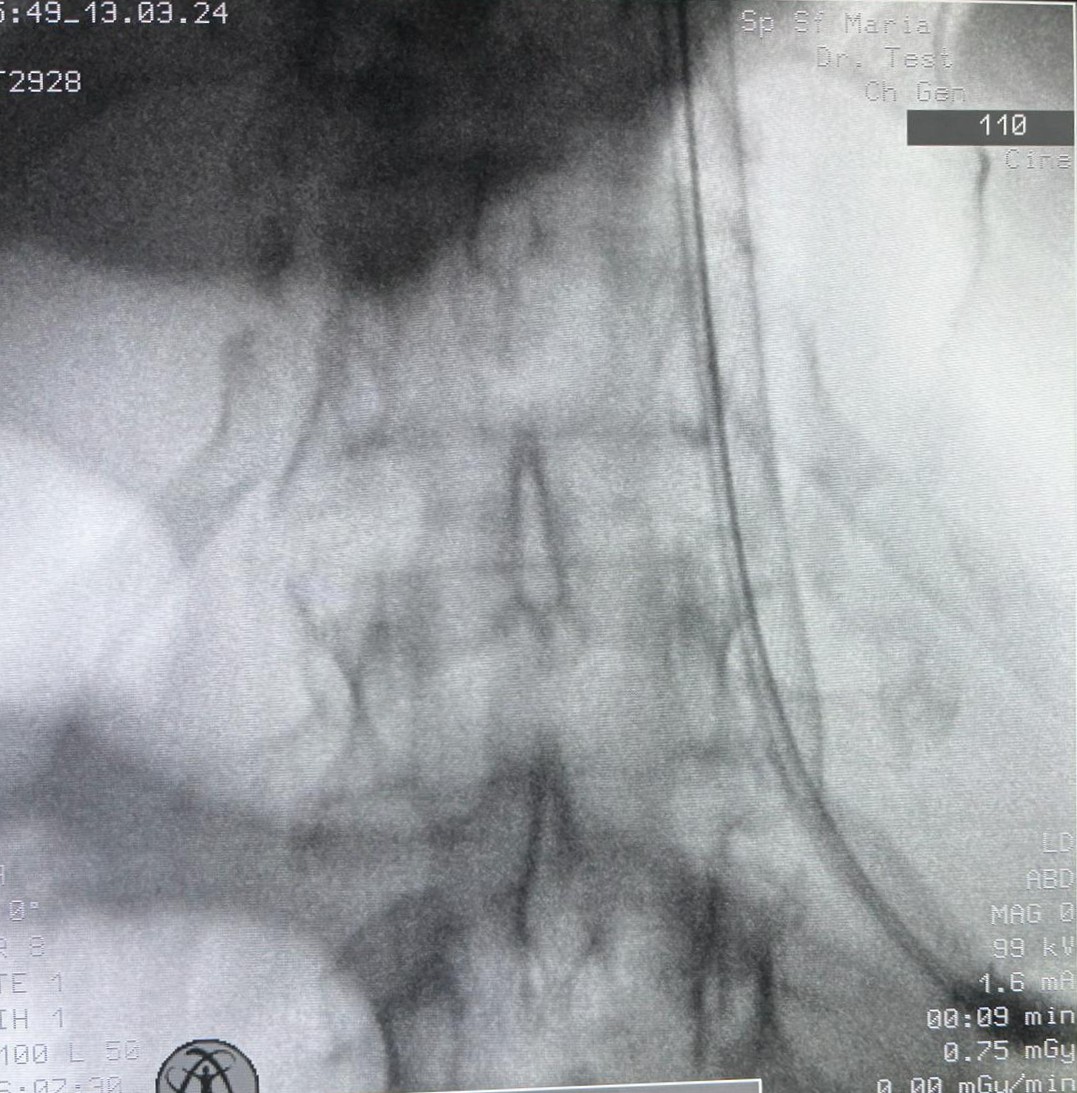
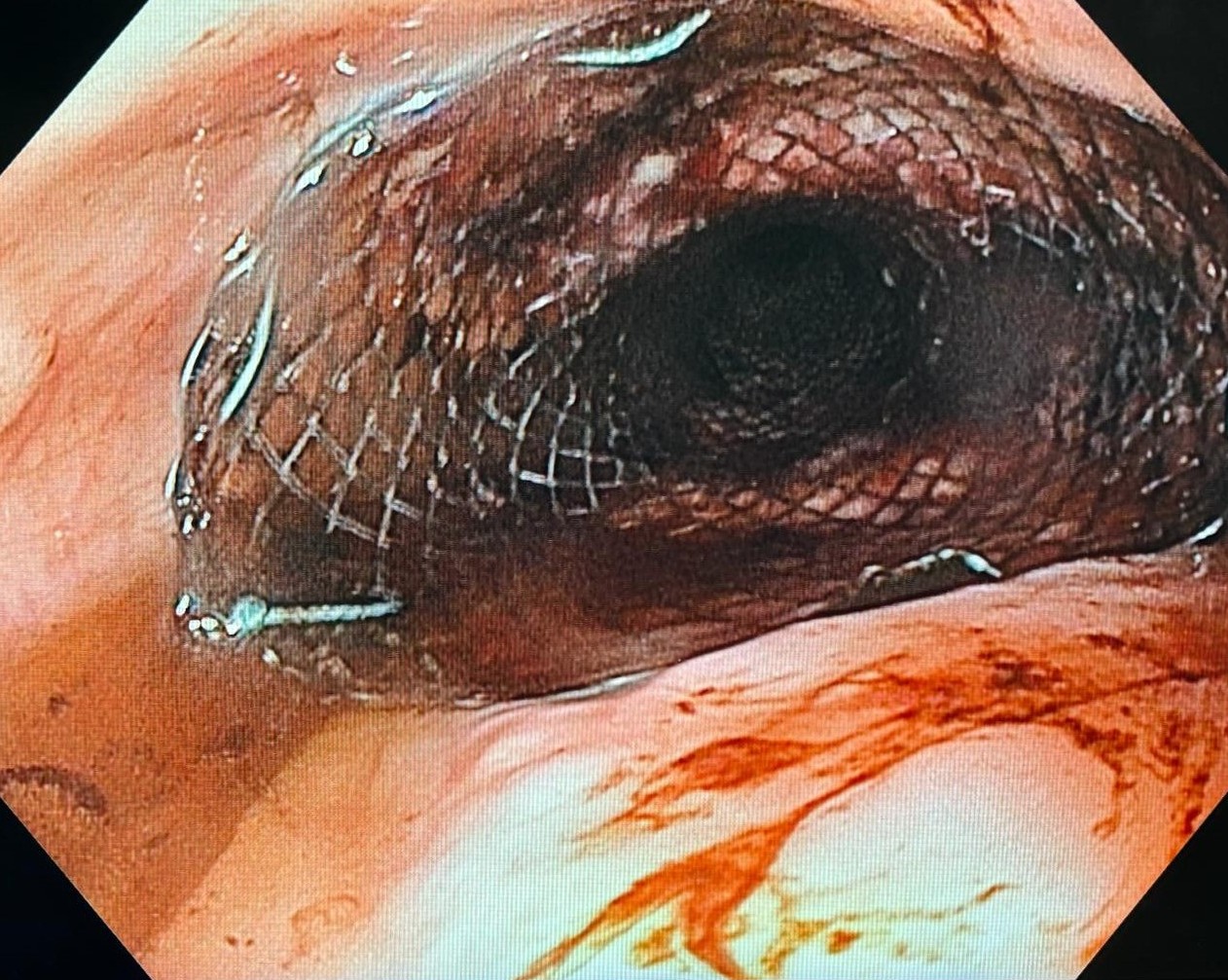
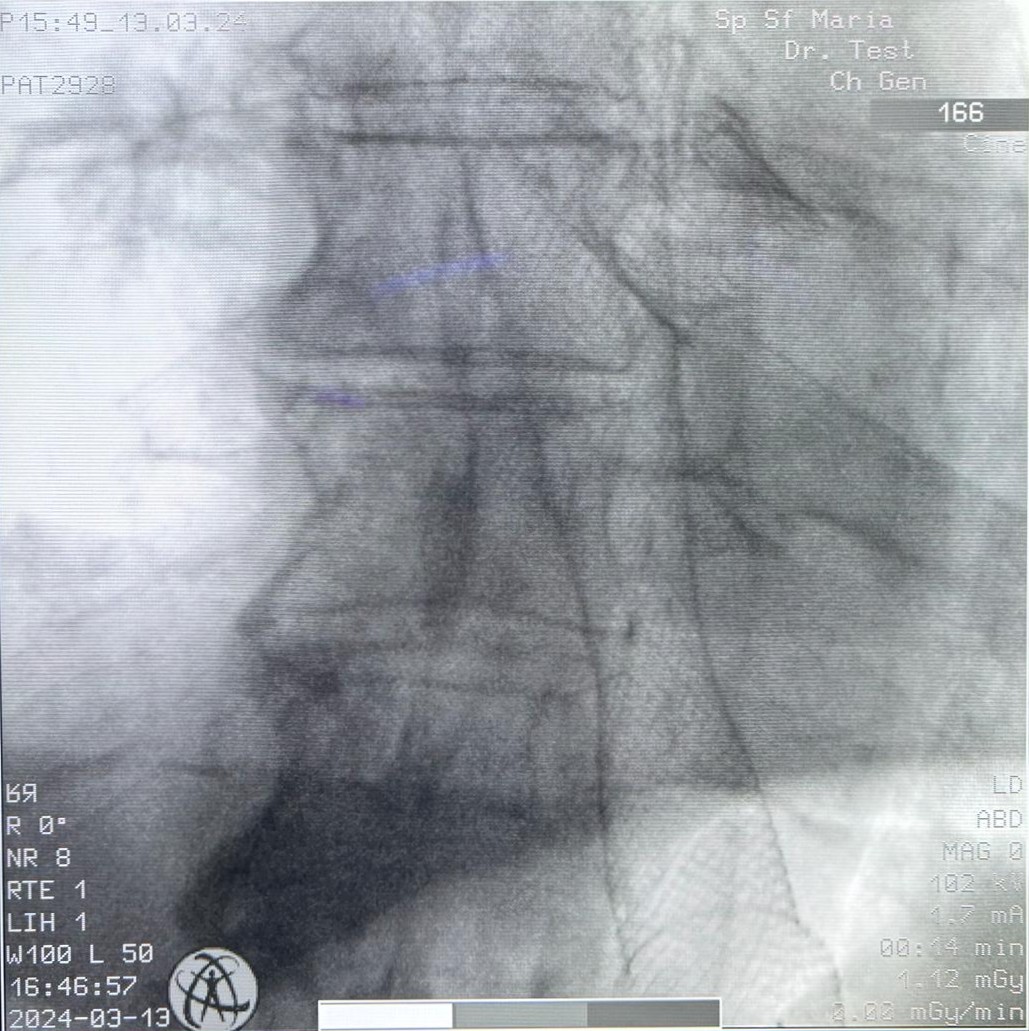
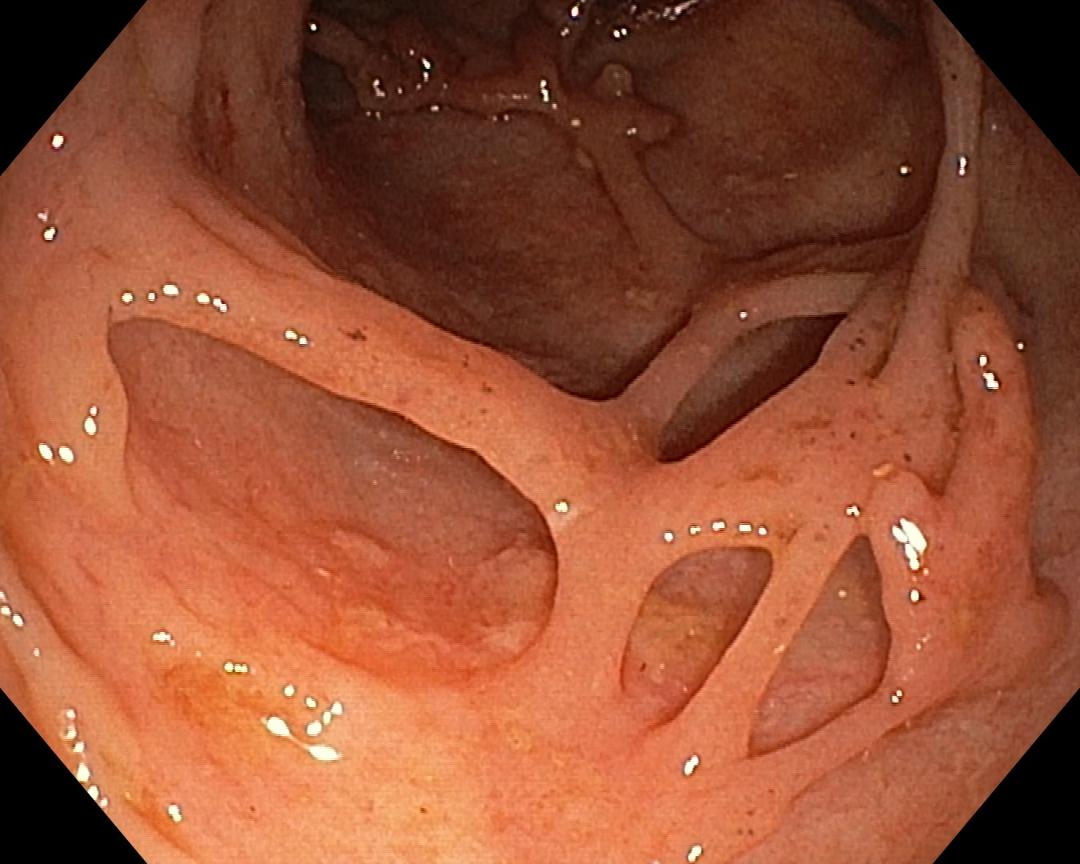
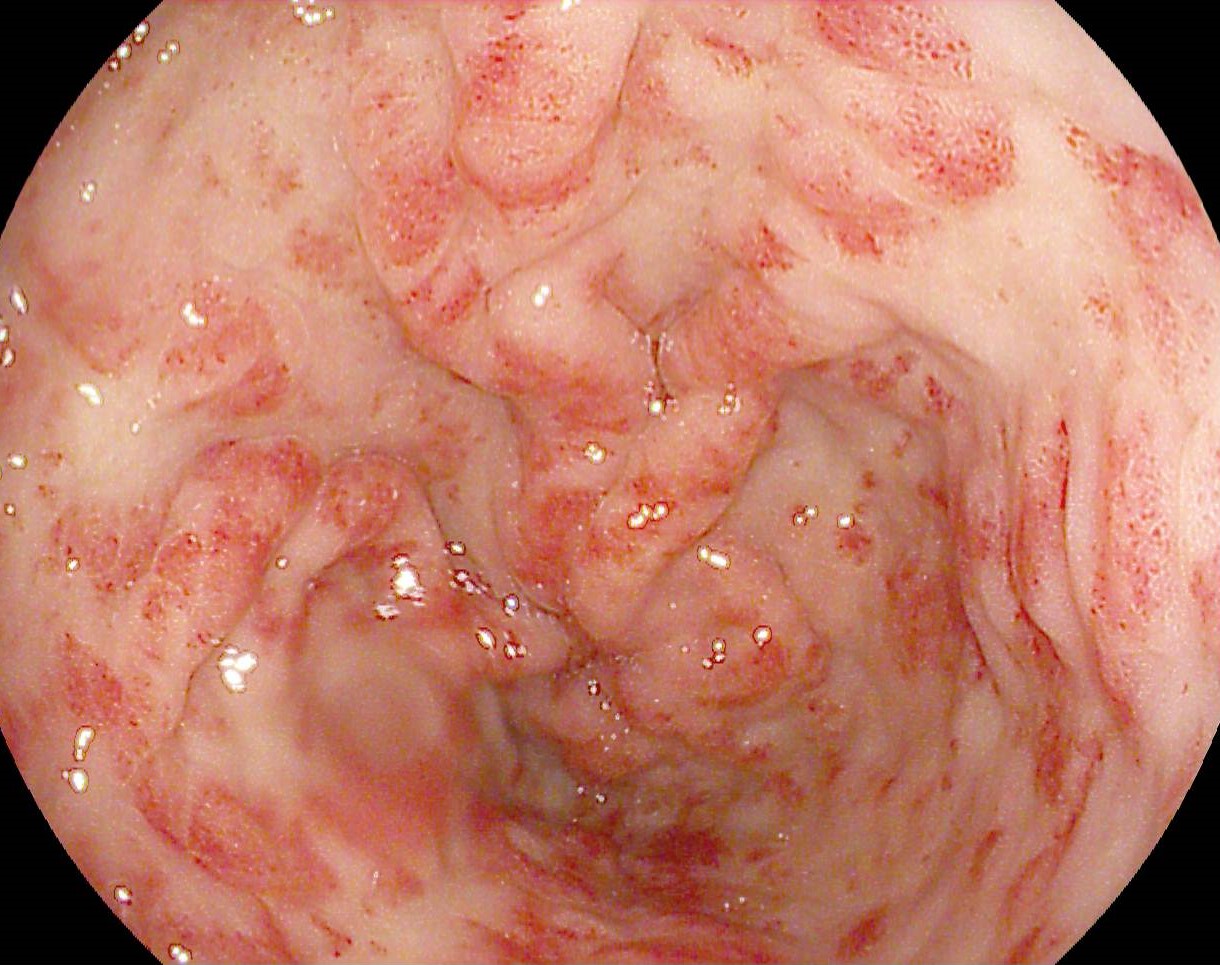
The patient was placed on nil per os (NPO) status and continuous proton pump inhibitor (PPI) infusion therapy was initiated. After obtaining informed consent, an upper gastrointestinal endoscopy was performed, revealing a stenosing tumor located 35 cm from the dental arcade, which could not be passed with the diagnostic gastroscope. The tumor showed multiple adherent clots and active bleeding (Image 1). Initial attempts to control the bleeding with conventional available methods, such as adrenaline injection, thermal coagulation and cold water lavage, were unsuccessful. Given the stenosing nature of the tumor and ongoing bleeding despite these measures, the decision was made to place a fully covered self-expandable metallic stent (FCSEMS) measuring 18 mm × 100 mm. The procedure aimed not only to restore luminal patency but also to control bleeding via tamponade effect. A Savary guidewire was advanced beyond the stricture, with its position confirmed fluoroscopically. The FCSEMS was then introduced over the guidewire under both direct visualization and fluoroscopic guidance (Images 3, 4) and was successfully deployed, aligning precisely over the described stricture (Images 5, 6). Following stent placement, the patient experienced no further episodes of hematemesis or melena, and no additional hemoglobin drop was observed. He was monitored in the hospital for 72 hours and discharged without postprocedural complications. Unfortunately, the patient was lost to further gastrointestinal endoscopic follow-up, but he continued with chemotherapy and radiotherapy.
Upper gastrointestinal bleeding secondary to esophageal adenocarcinoma.
The placement of metallic stents has become a standard therapy for benign and malignant gastrointestinal tract strictures. Traditionally, in esophageal pathology, metal stents were first introduced to relieve obstruction caused by esophageal tumors. These stents not only help alleviate obstruction but also appear to be useful in the management of tracheoesophageal fistulas, esophageal perforations, and post-operative esophageal leaks. Despite success rates approaching 80%, their use has often been associated with significant complications, such as stent migration, obstruction, and perforation.
Bleeding, occurring in approximately 1%–5% of upper gastrointestinal tract tumors, represents another significant challenge. Endoscopic therapy is considered the first-line approach for achieving hemostasis and includes techniques such as local adrenaline injection, thermal probes, argon plasma coagulation, radiofrequency ablation, cryotherapy, and hemospray. Despite the variety of available techniques, rebleeding is frequent. Although metallic stents are used as salvage therapy in cases of refractory variceal bleeding, their role in managing malignant gastrointestinal hemorrhage is not yet well established.
In this case, a stent was placed in a diffusely bleeding esophageal tumor that also caused severe luminal obstruction. The intervention led to complete symptom resolution, with no recurrence of bleeding, and the patient was discharged after 72 hours.
In this case, the use of fully covered self-expandable metallic stents (FCSEMSs) proved to be a safe and effective method for managing recurrent or refractory malignant gastrointestinal bleeding.
- Orii T, Karasawa Y, Kitahara H, et al. Efficacy of self-expandable metallic stent inserted for refractory hemorrhage of duodenal cancer. Case Rep Gastroenterol 2016; 10(1): 151–156
- Spaander Manon CW, Baron TH, Siersema PD, et al. Esophageal stenting for benign and malignant disease: ESGE clinical guideline. Endosc 2016; 48: 939–948.
- Rabenstein T. Palliative endoscopic therapy of esophageal cancer. Viszeralmedizin 2015; 31: 354–359.
- Martinez JC, Puc MM, Quiros RM. Esophageal stenting in the setting of malignancy. ISRN Gastroenterol 2011; 2011: 719575.
- Rockall TA, Logan RF, Devlin HB, et al. Risk assessment after acute upper gastrointestinal haemorrhage. Gut 1996; 38(3): 316–321.
- Ofosu A, Ramai D, Latson W, et al. Endoscopic management of bleeding gastrointestinal tumors. Ann Gastroenterol 2019; 32(4): 346–351.
- Escorsell A, Bosch J. Self-expandable metal stents in the treatment of acute esophageal variceal bleeding. Gastroenterol Res Pract 2011; 2011: 910986.
- Bilal S, Saeed SM, Siddique MZ, Saqib M, Mehmood S, Yusuf MA. Salvage therapy of bleeding esophageal tumor by fully covered self-expandable metallic stent: A case report. SAGE Open Med Case Rep. 2021 Feb 24;9:2050313X21997198. doi: 10.1177/2050313X21997198. PMID: 33717487; PMCID: PMC7925943.