See other cases
Stent in stent in stent for a huge postoperative gastro-pleural fistula – an endoscopic challenge ?
A 73-year-old man was diagnosed with moderately differentiated adenocarcinoma (T3N0M0) of the esophagogastric junction. At the time of diagnosis, the tumor was stenotic and could not be bypassed with the gastroscope; at that time, it was decided to place an uncovered esophageal stent, and subsequently, the patient received neoadjuvant chemotherapy.
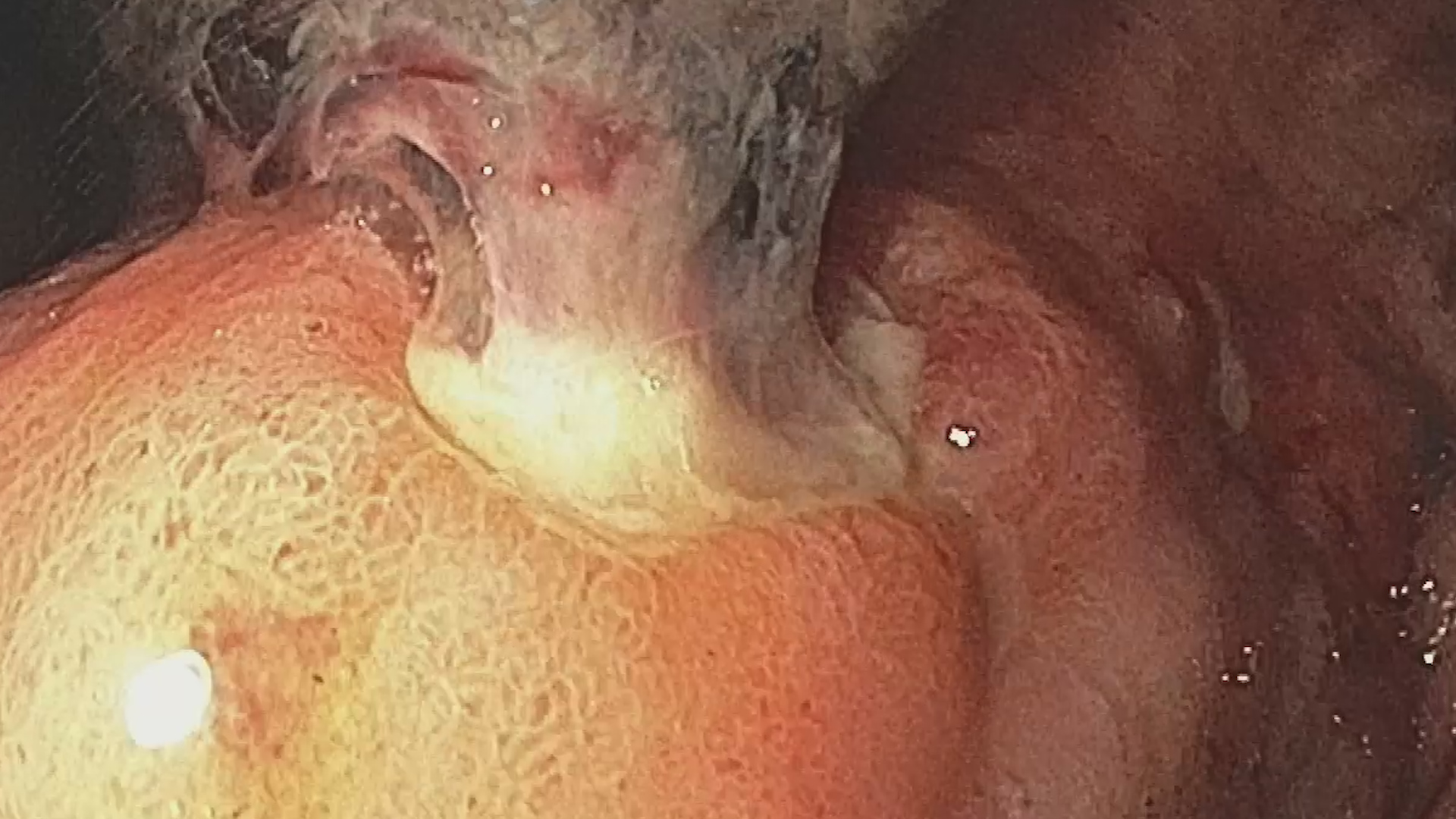
Four months later, the patient’s condition deteriorated, with progressive dysphagia, and he was urgently re-evaluated – a computed tomography (CT) scan followed by upper digestive endoscopy (EDS) confirmed esophageal stenosis due to the extensive tumor, with tumor ingrowth in the upper portion of the previously placed stent. The surgeon decided on an intervention involving subtotal esophagectomy associated with polar superior gastrectomy, with intrathoracic eso-gastroanastomosis; additionally, a jejunostomy was surgically placed, and the patient was put on nil per os (NPO). The surgery was challenging due to significant posterior mediastinal fibrosis caused by the previous placement of an uncovered esophageal stent. The esophagectomy was complicated by anastomotic insufficiency, resulting in a gastro-pleural fistula which required endoscopic treatment.
Clinical – ECOG score 2, febrile, intensely dyspneic, without abdominal pain, with subcutaneous emphysema in the anterior chest and pleural drainage tubes in situ.
Biological – significant inflammatory syndrome with CRP 300 mg/L, procalcitonin 11 ng/ml, severe normochromic anemia with Hb 7.5 g/dl and leukocytosis 17,000/mm³.
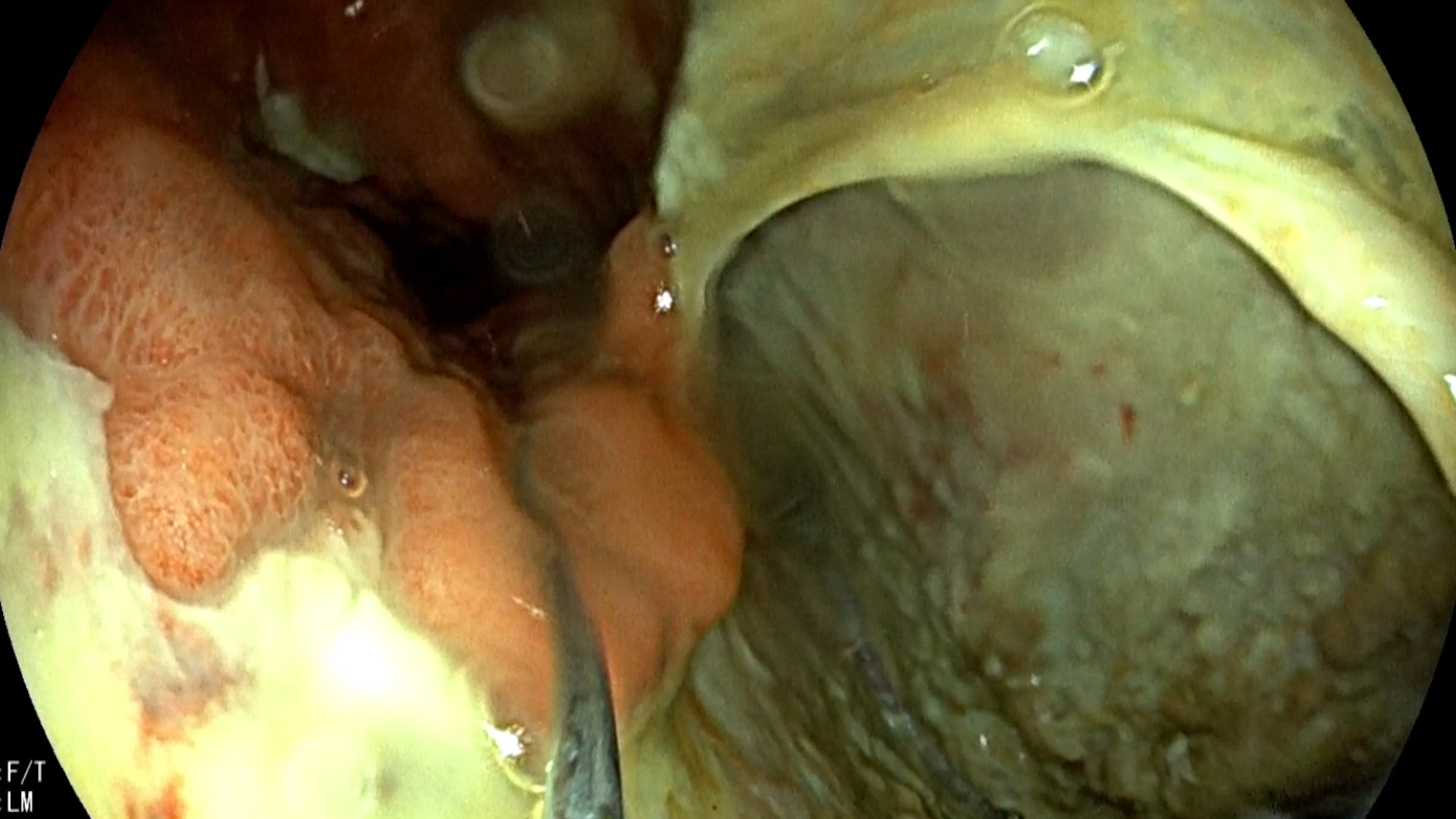
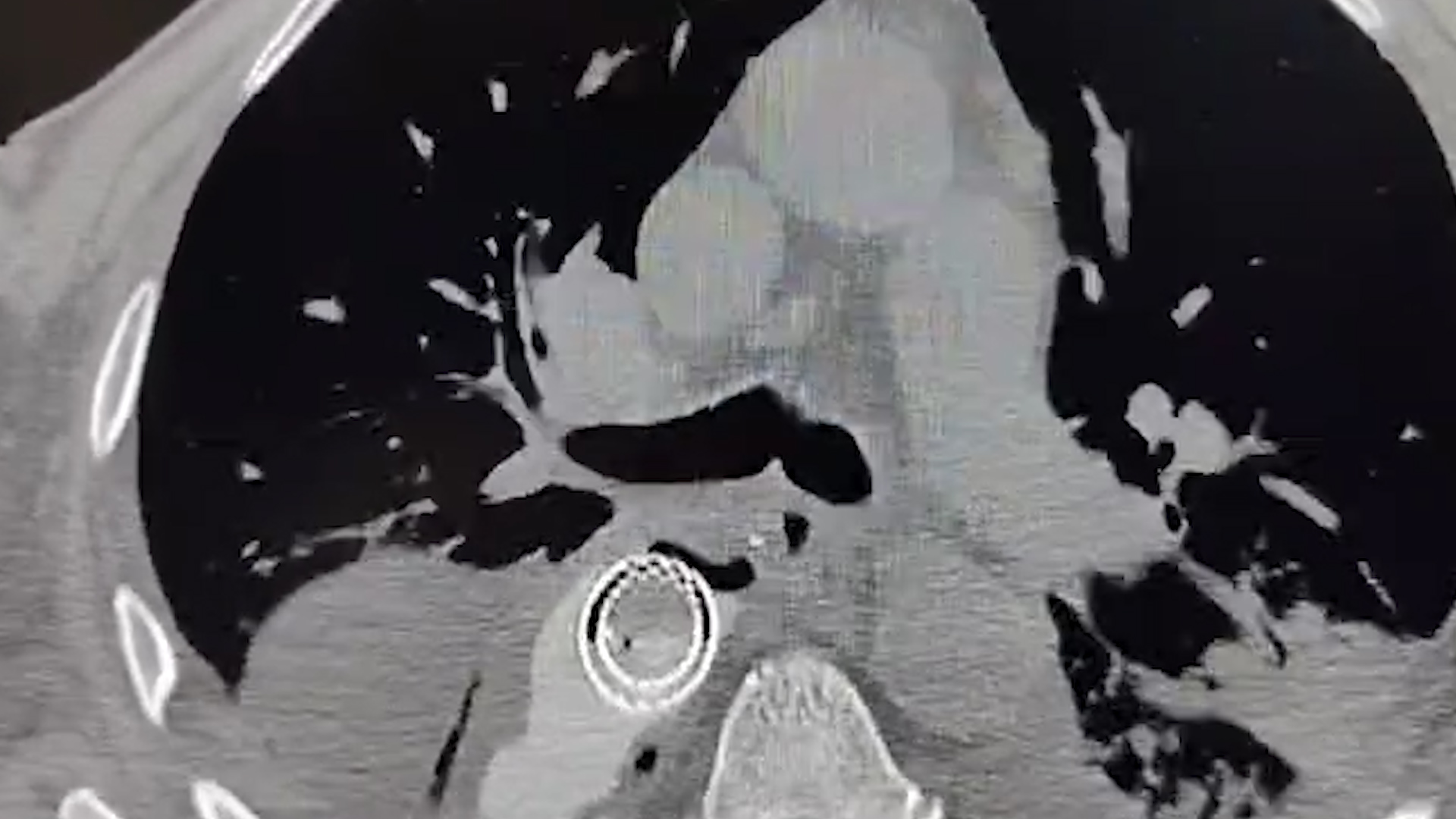
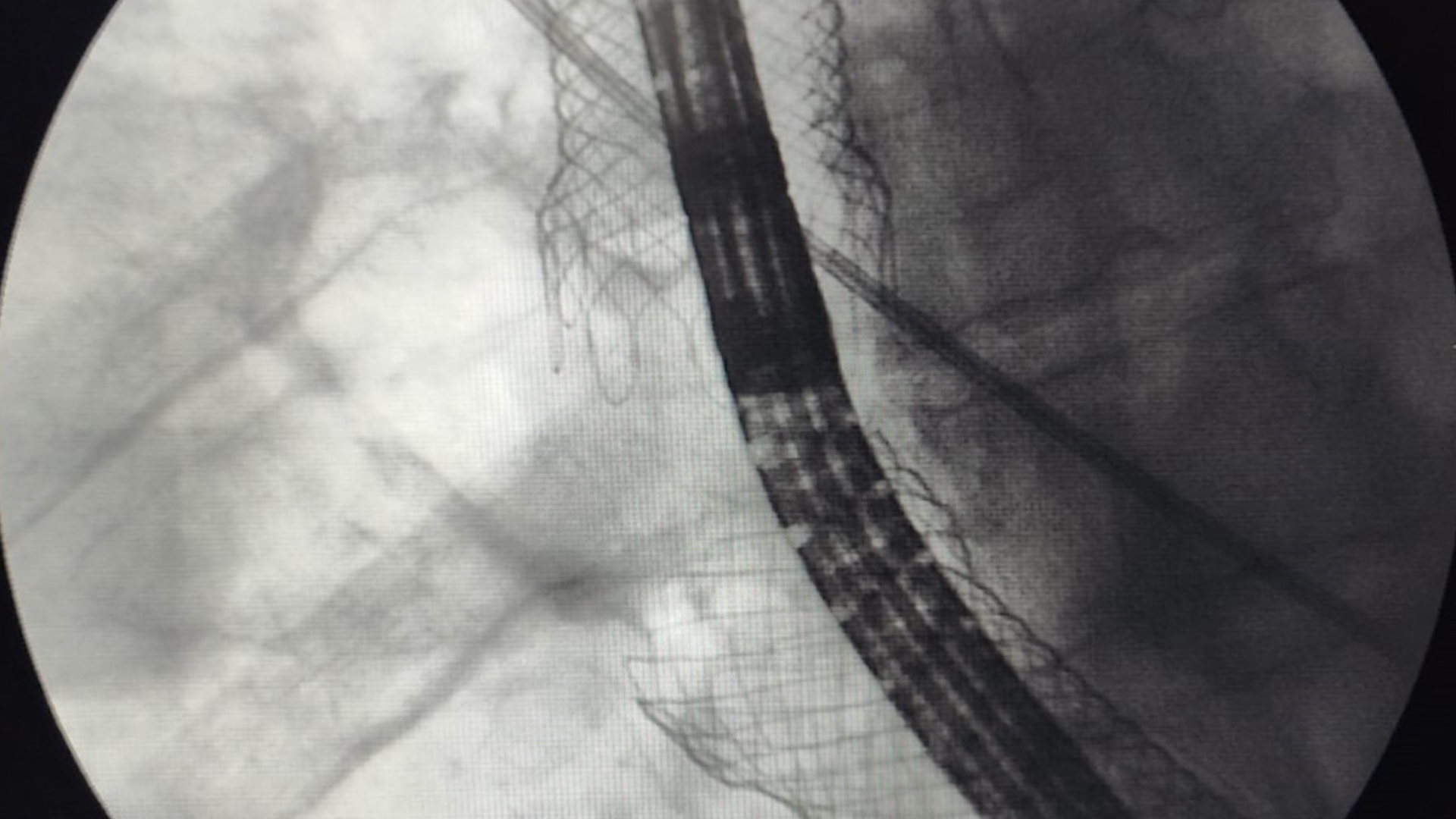
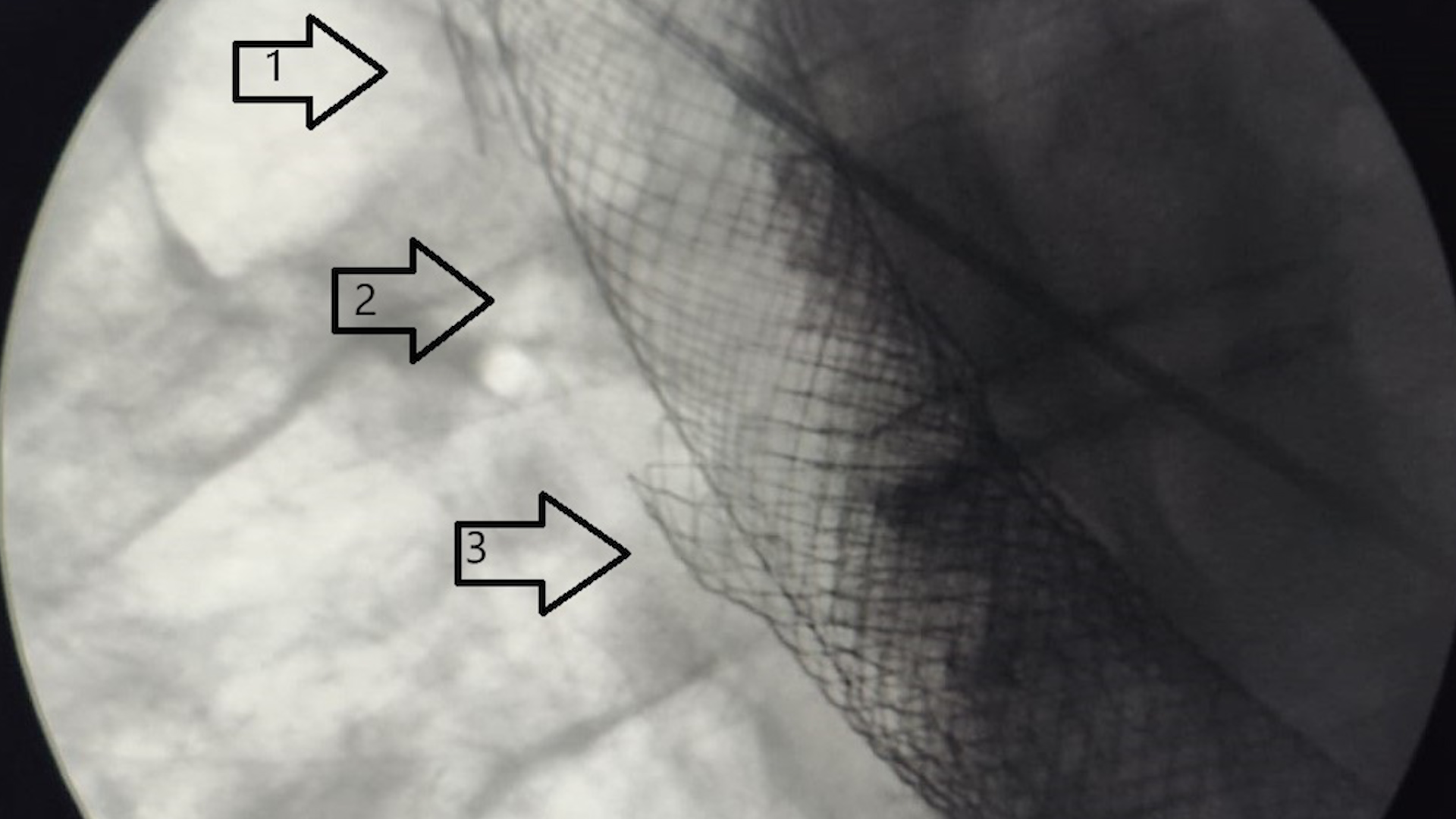
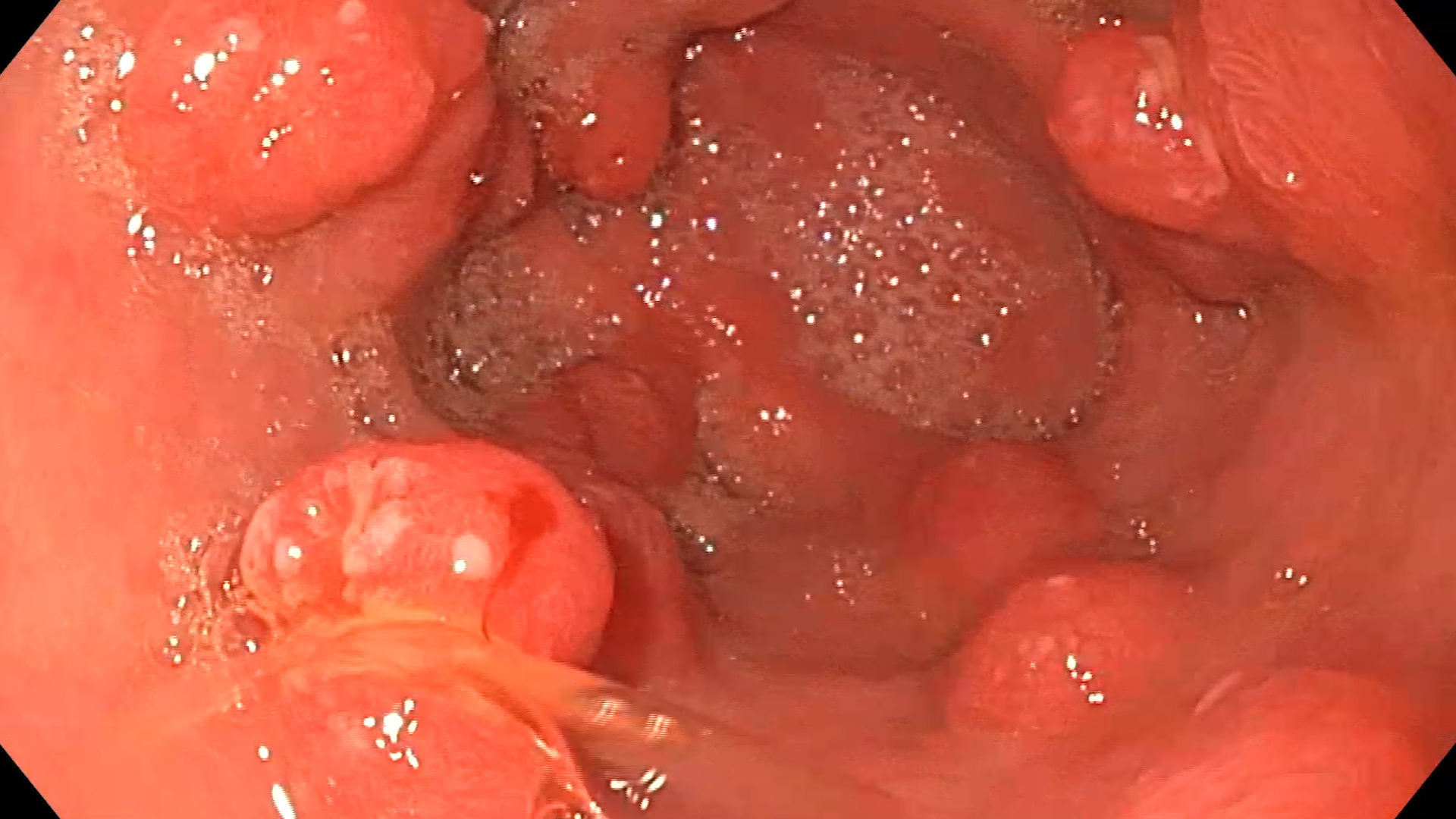
At the time of admission to our service, the CT examination of the chest noted the extravasation of orally administered contrast material outside the gastric lumen, forming a fistulous tract, with the accumulation of contrast in the right pleural cavity. Upper digestive endoscopy confirmed the presence of a massive 14 cm parietal defect. It was decided to undertake interventional endoscopic treatment to correct the postoperative fistula. To effectively cover the defect, it was decided to use two fully covered self-expandable esophageal metal stents (SEMS) measuring 23.5 x 105 mm (Wallflex™, Boston Scientific); under general anesthesia with orotracheal intubation and mechanical ventilation, and under fluoroscopic guidance, the stents were endoscopically advanced over a Savary guidewire and deployed sequentially. To prevent migration, the stent-in-stent method was used, and the upper prosthesis was anchored with multiple hemostatic clips to the esophageal mucosa. Additionally, continuous drainage of the pleural cavity was maintained.
CT examination with oral contrast of the chest at 24 hours post-procedure describes stents positioned in the eso-gastric area, fully expanded, with contrast passage up to the duodenal level without leakage into the pleural collection. After the placement of the esophageal stents, the patient received broad-spectrum antibiotic therapy, proton pump inhibitors, human albumin, analgesics, parenteral nutrition, and dynamic administration of red blood cell mass, leading to clinical and biochemical improvement of the patient.
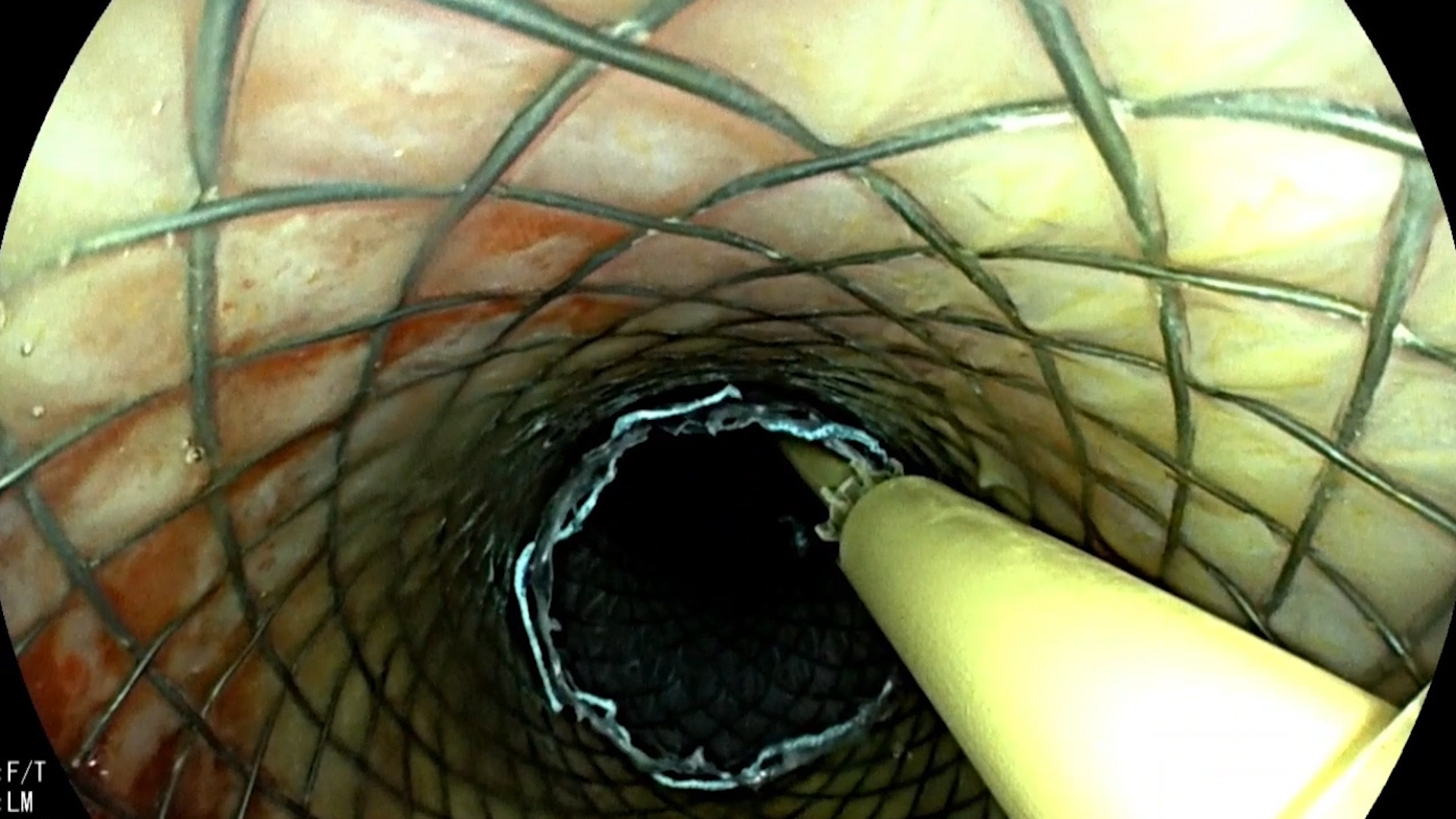
Six days post-procedure, the patient’s condition deteriorates again, with a significant inflammatory syndrome. The CT examination of the chest describes the downward migration of the lower stent, with the passage of orally administered contrast into the pleural cavity. An endoscopic reevaluation is decided, and it is observed that the previously placed lower esophageal stent has migrated into the gastro-pleural fistula cavity; using an alligator forceps, the stent is repositioned into the gastric lumen. At this point, it is observed that it is no longer possible to achieve a tight seal between the two stents, so the endoscopic team decides to endoscopically place a third fully covered metal stent, measuring 23.5 x 125 mm (Wallflex™, Boston Scientific), under fluoroscopic guidance to compactly join the two previously placed prostheses. The follow-up chest X-ray the next day confirms the presence of the three fully expanded stents covering the entire fistulous tract, without the extravasation of orally administered contrast agent.
Gastro-pleural fistula post-subtotal esophagectomy with polar superior gastrectomy.
Current guidelines reccomand placement of partially or fully covered self-expandable metal stents for palliation of malignant esophageal stenosis. On the other hand, esophageal fistula represents a severe postoperative complication, being an event with potentially severe progression and high mortality. Esophageal fistula can be approached endoscopically, with the method varying depending on the location and size. Small defects, under 2 cm, can be closed with repositionable clips or OTSC-type clips, while larger defects can be addressed by placing fully covered esophageal stents or by applying vacuum therapy. Simultaneously, the patient can benefit from the percutaneous placement of a gastrostomy/jejunostomy endoscopically, thus allowing feeding.
The placement of an esophageal stent in a patient without esophageal obstruction is associated with a high risk of migration, so it is recommended to use stents with the largest possible diameter, anchor the prosthesis with TTS/OTS-type clips, or approach the stent-in-stent method. Additionally, if mediastinal collections or collections in other locations are present, they should be surgically drained. The optimal duration for maintaining the stent is not standardized, varying between 4 and 8 weeks, after which the prosthesis is removed endoscopically.
Factors associated with successful primary closure of the fistula include a shorter time between the diagnosis of the esophageal fistula and the initial insertion of the stent, as well as a smaller defect size. On the other hand, it has been found that stenting failure was significantly more frequent in patients with a proximal cervical esophageal fistula, in prostheses that extend beyond the gastroesophageal junction, and in those with an esophageal defect longer than 6 cm.
Fully covered esophageal stents can be successfully used in the case of esophageal fistulas of various causes. Due to the relatively high risk of migration, it is recommended that these stents be anchored with TTS/OTS-type clips or by placing esophageal stents in a stent-in-stent manner.
- El Hajj II, Imperiale TF, Rex DK, Ballard D, Kesler KA, Birdas TJ, Fatima H, Kessler WR, DeWitt JM. Treatment of esophageal leaks, fistulae, and perforations with temporary stents: evaluation of efficacy, adverse events, and factors associated with successful outcomes. Gastrointest Endosc. 2014 Apr;79(4):589-98. doi: 10.1016/j.gie.2013.08.039. Epub 2013 Oct 11. PMID: 24125513.
- Freeman RK, Ascioti AJ, Giannini T, Mahidhara RJ. Analysis of unsuccessful esophageal stent placements for esophageal perforation, fistula, or anastomotic leak. Ann Thorac Surg. 2012 Sep;94(3):959-64; discussion 964-5. doi: 10.1016/j.athoracsur.2012.05.047. Epub 2012 Jul 12. PMID: 22795060.
- Rosianu, C.G.; Hoara, P.; Achim, F.; Birla, R.; Bolocan, A.; Mohssen, A.; Copca, N.; Constantinoiu, S. The Use of Esophageal Stents in the Management of Postoperative Fistulas—Current Status, Clinical Outcomes and Perspectives—Review. Life2023, 13, 966. https://doi.org/10.3390/life13040966
- Ishtiaq J, Sutton J, Ahmed W. A novel management of post-oesophagectomy gastro-pleural fistula. J Gastrointest Oncol. 2016 Dec;7(6):E93-E97. doi: 10.21037/jgo.2016.09.12. PMID: 28078131; PMCID: PMC5177580.
- Spaander MCW, van der Bogt RD, Baron TH, Albers D, Blero D, de Ceglie A, Conio M, Czakó L, Everett S, Garcia-Pagán JC, Ginès A, Jovani M, Repici A, Rodrigues-Pinto E, Siersema PD, Fuccio L, van Hooft JE. Esophageal stenting for benign and malignant disease: European Society of Gastrointestinal Endoscopy (ESGE) Guideline – Update 2021. Endoscopy. 2021 Jul;53(7):751-762. doi: 10.1055/a-1475-0063. Epub 2021 Apr 30. PMID: 33930932.