See other cases
Scar Resection assisted by Band-Ligation for incomplete EMR
Female, 66-year-old, obese patient, with multiple known heart conditions was admitted to our clinic for colonoscopy. The patient was complaining of tenesmus and proctalgia.
Clinical exam: normal bowel habit, with normal stool.
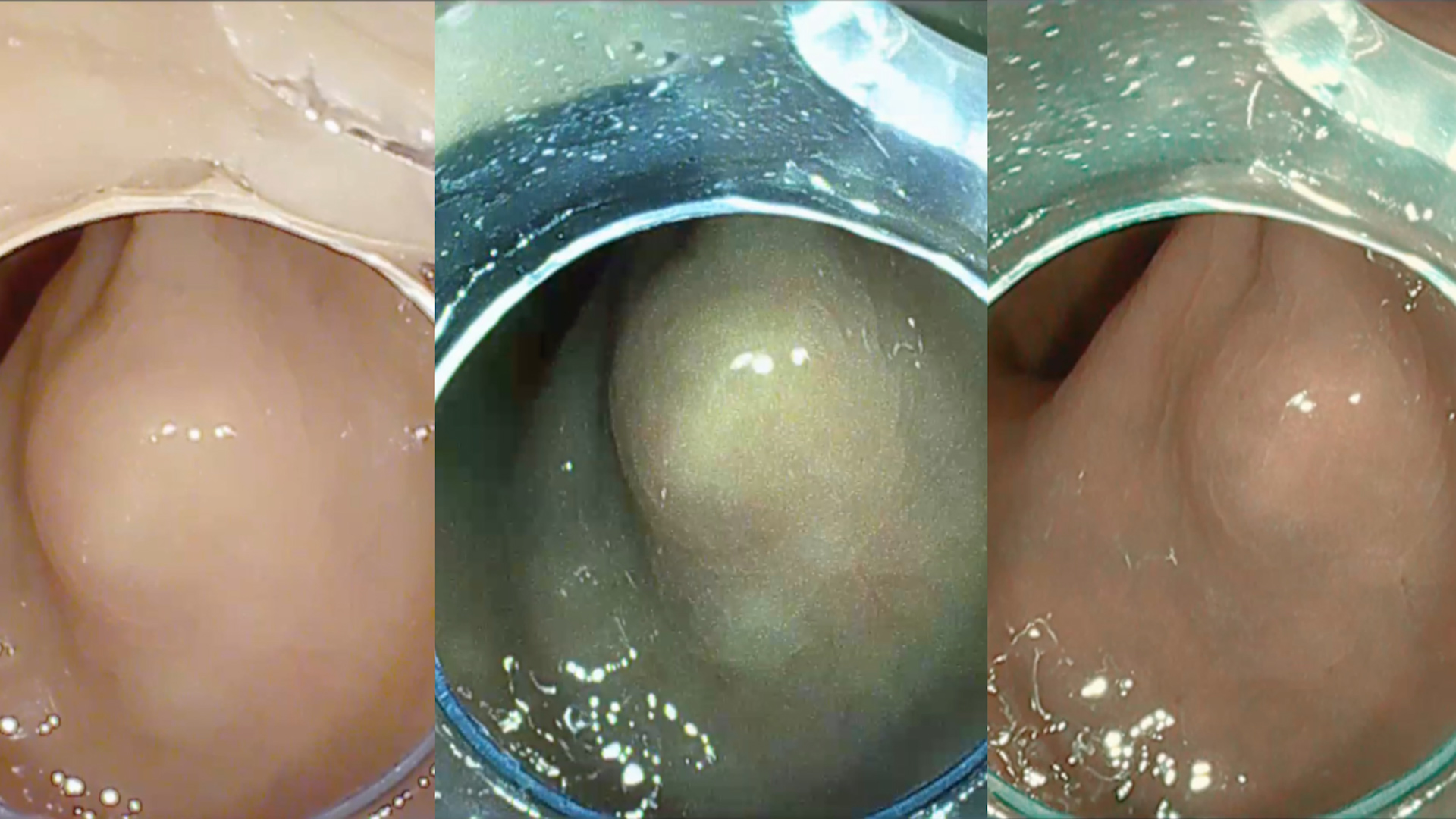
Colonoscopy: An incidental subepithelial lesion located in the rectum was identified, with normal surface mucosa, approximately 10 mm in size (Figure 1). A recommendation of follow-up with endoanal ultrasound was issued.
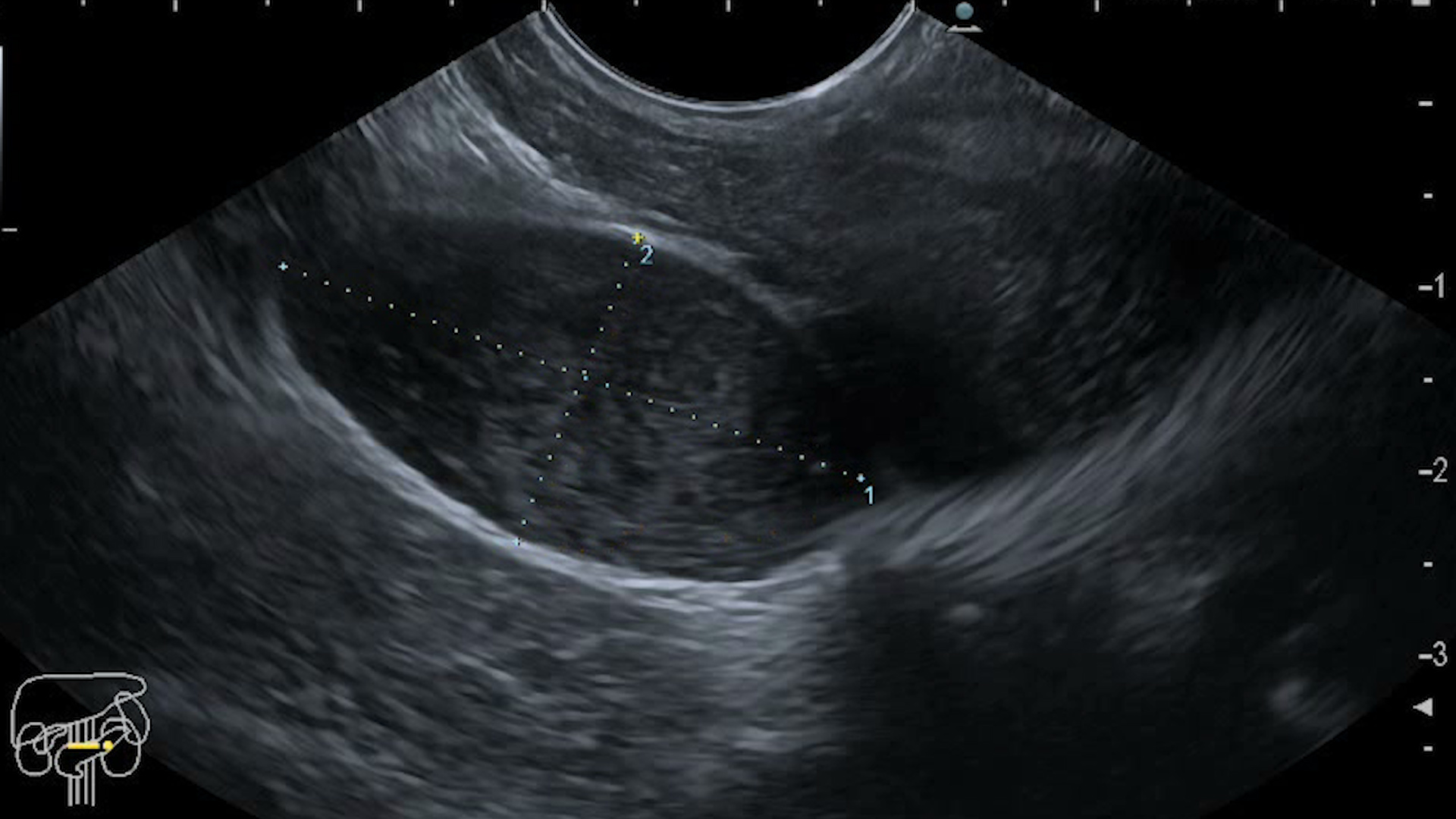
Endoanal ultrasound: Located approximately 6 cm from the anal verge – hypoechoic, roundish mass, with a few hyperechoic spots inside, emerging from the second layer of the rectal wall (hypoechoic – muscularis mucosae), without invading the over/underlying strata (Figure 2).
Rectoscopy for biopsy of subepithelial lesion: Multiple “bite on bite” biopsies from the lesion. The pathological exam revealed a well-differentiated (G1) neuroendocrine tumor infiltrating the mucosa and focally the submucosa visible on the specimen.
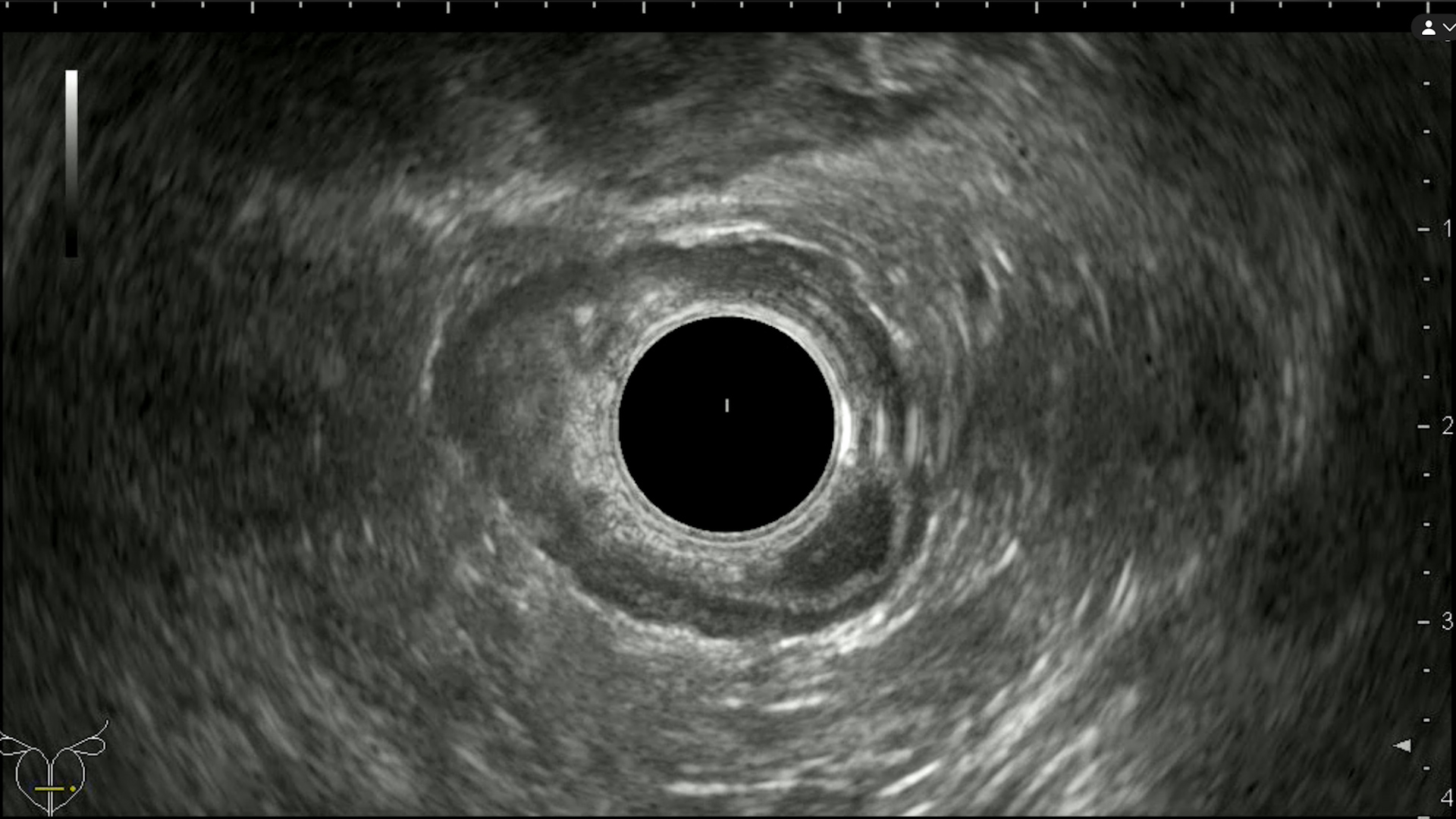
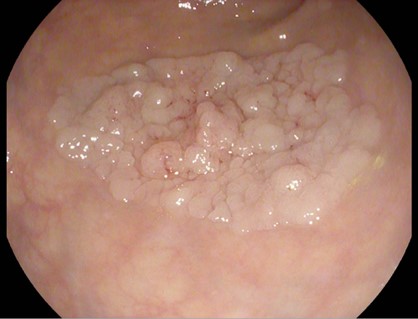
Rectoscopy: En bloc conventional endoscopic mucosal resection (EMR) of the tumor was attempted, with residual millimetric tumor tissue visible in the center of the resection defect (Figure 3). The residual tissue was, subsequently, resected using a snare. The pathological exam showcases a well-differentiated (G1) neuroendocrine tumor, invading the mucosa and submucosa (pT1a). Tumor tissue is present at the resection margin. In these circumstances, we decided to complete the endoscopic resection.
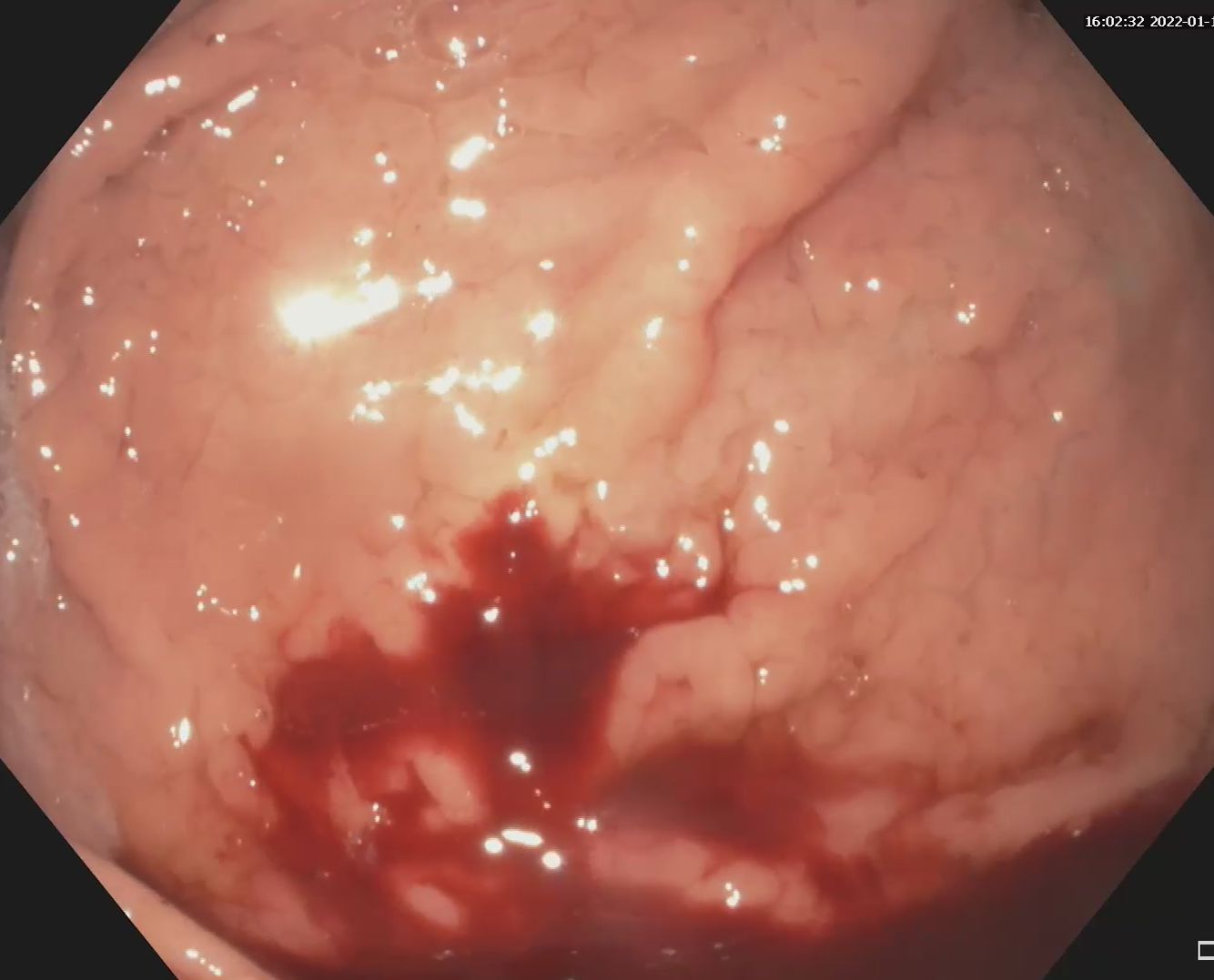
Rectosigmoidoscopy (6 months after initial resection): Post-resection scar was identified. The perimeter of the scar was marked with the tip of the snare, after which the scope was reinserted with the banding system preinstaled. The scar was suctioned into the cap while checking that the markings were also withing the cap, after which a band was released (Figure 4). Next, the snare was applied below the elastic ring. The thus-formed pseudo-polyp was mobilized, to check for captured muscularis propria, after which the resection was completed. The resulting defect had a normal appearance and was also closed using a large clip (Figure 5). The resection piece contained a fragment of rectal scar mucosa and submucosa with no evidence of tumor infiltration and no other significant pathological abnormalities.
Well differentiated neuroendocrine tumor WHO grade 1, invading the submucosa and mucosa.
In most cases, rectal neuroendocrine tumors are small, originating from the mucosa or submucosa. Patients are frequently asymptomatic, and the tumors are an incidental finding. Their size correlated well with the presence of metastases. The risk of concomitant metastases for rectal NETs ≤1 cm is approximately 2% [1].
Tumors ≤ 1 cm in size, originating from the mucosa and submucosa (T1), can generally be resected endoscopically, especially in the absence of other risk factors. The local extent can be estimated using transanal ultrasound using a rigid probe or endoscopic ultrasound (whichever is available). More advanced endoscopic techniques, such as band-ligation assisted EMR, can be used, which allow for a higher rate of negative histological margins [2]. The technique is similar in principle to underwater EMR (UEMR). Both techniques are performed without the need for submucosal injection and facilitate the proper ensnaring of tissue, including scar tissue (after previous EMR or biopsy). In this situation, band-assisted EMR of the scar tissue was preferred (because of positive histological margins of the initial resection), as water retention in the rectum is difficult to obtain. Band-assisted EMR is performed by aspiration of the mucosa into the endocap, reducing the intraluminal pressure, after which an elastic band is released, strangling the mucosa and submucosa and separating them from the muscularis propria. Vigorous aspiration should be avoided, such as in the case of variceal banding, because this can lead to the capture of deep wall strata and, consequently, to perforation. Band-assisted EMR, as well as UEMR, are considered optimal techniques for resecting rectal NETs, especially in cases where scar tissue is present [3, 4].
Band-assisted EMR is an efficient method for en-bloc resection of rectal neuroendocrine tumors, especially those ≤1 cm, facilitating a higher rate of complete resection. Although endoscopic reevaluation did not show local recurrence, in this particular case we preferred to complete the resection using band-assisted EMR, in order to exclude any residual neuro-endocrine tissue, given the initial histology report.
- Mani S, Modlin IM, Ballantyne G, Ahlman H, West B. Carcinoids of the rectum. J Am Coll Surg 1994;179(2):231.
- Ono A, Fujii T, Saito Y, Matsuda T, Lee DT, Gotoda T, Saito D. Endoscopic submucosal resection of rectal carcinoid tumors with a ligation device. Gastrointest Endosc 2003;57(4):583.
- Shi, H., Wang, C., Wu, J. et al. Underwater endoscopic mucosal resection for rectal neuroendocrine tumors (with videos): a single center retrospective study. BMC Gastroenterol 2022;22:276.
- Herman T, Megna B, Pallav K, Bilal. M. Endoscopic mucosal resection: tips and tricks for gastrointestinal trainees. Transl Gastroenterol Hepatol 2023;8:25.