See other cases
Rectal LST-G
A 54-year-old male patient presented for colonoscopic evaluation as part of an opportunistic screening program.
Within normal limits.
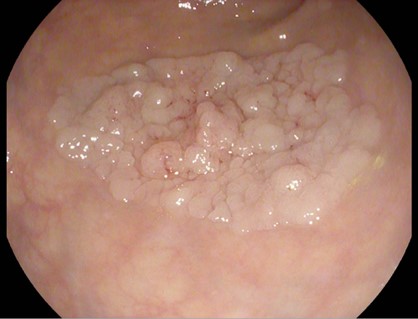
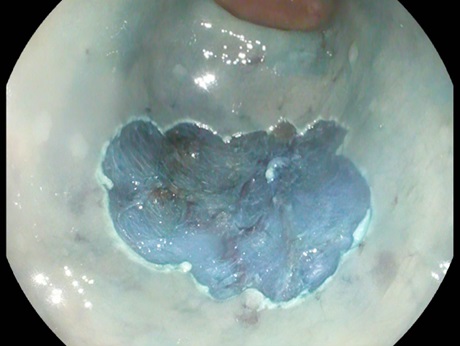
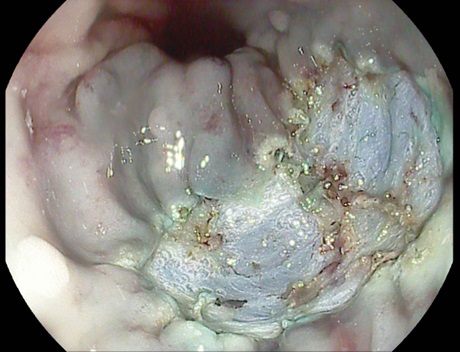
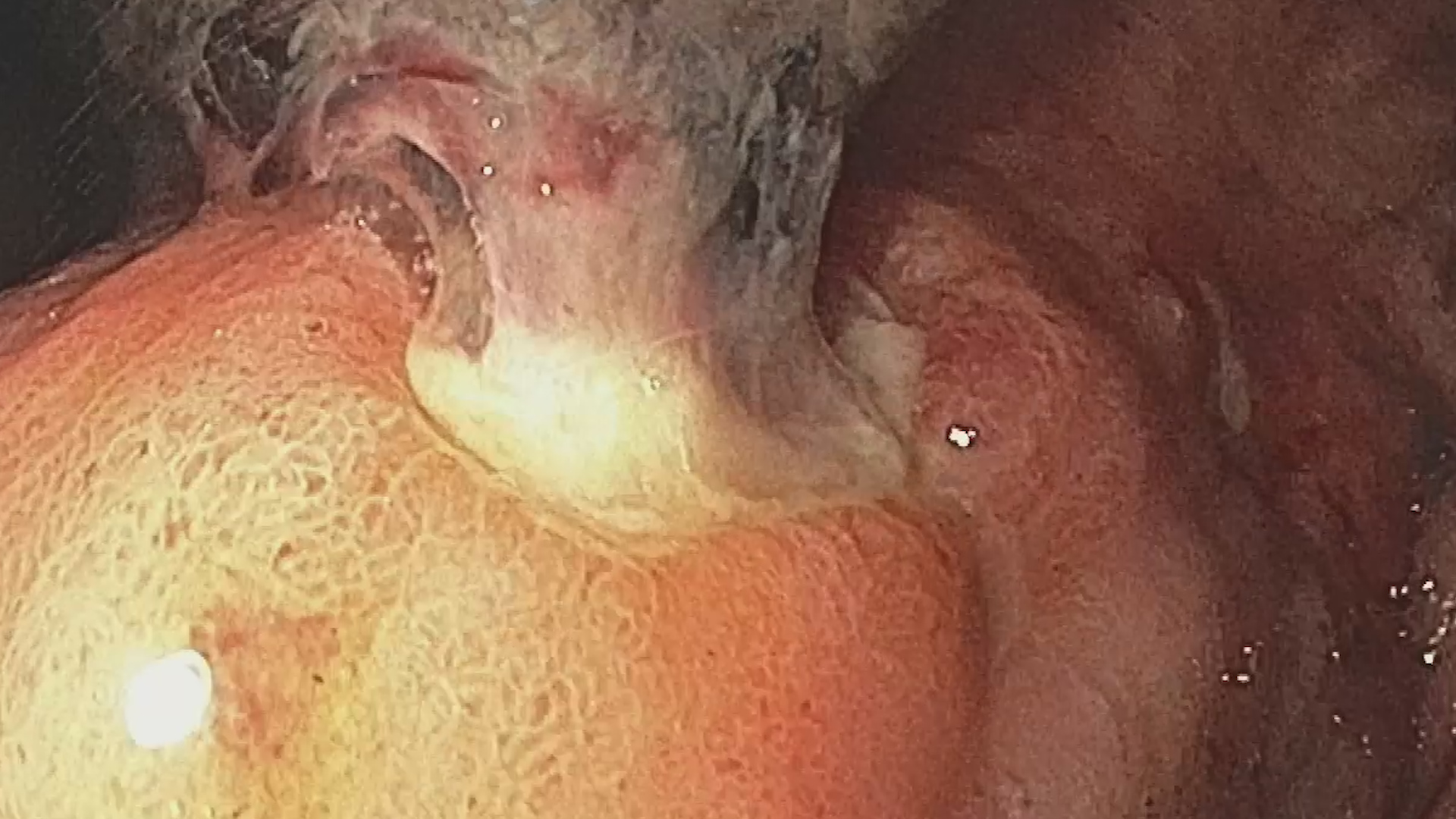
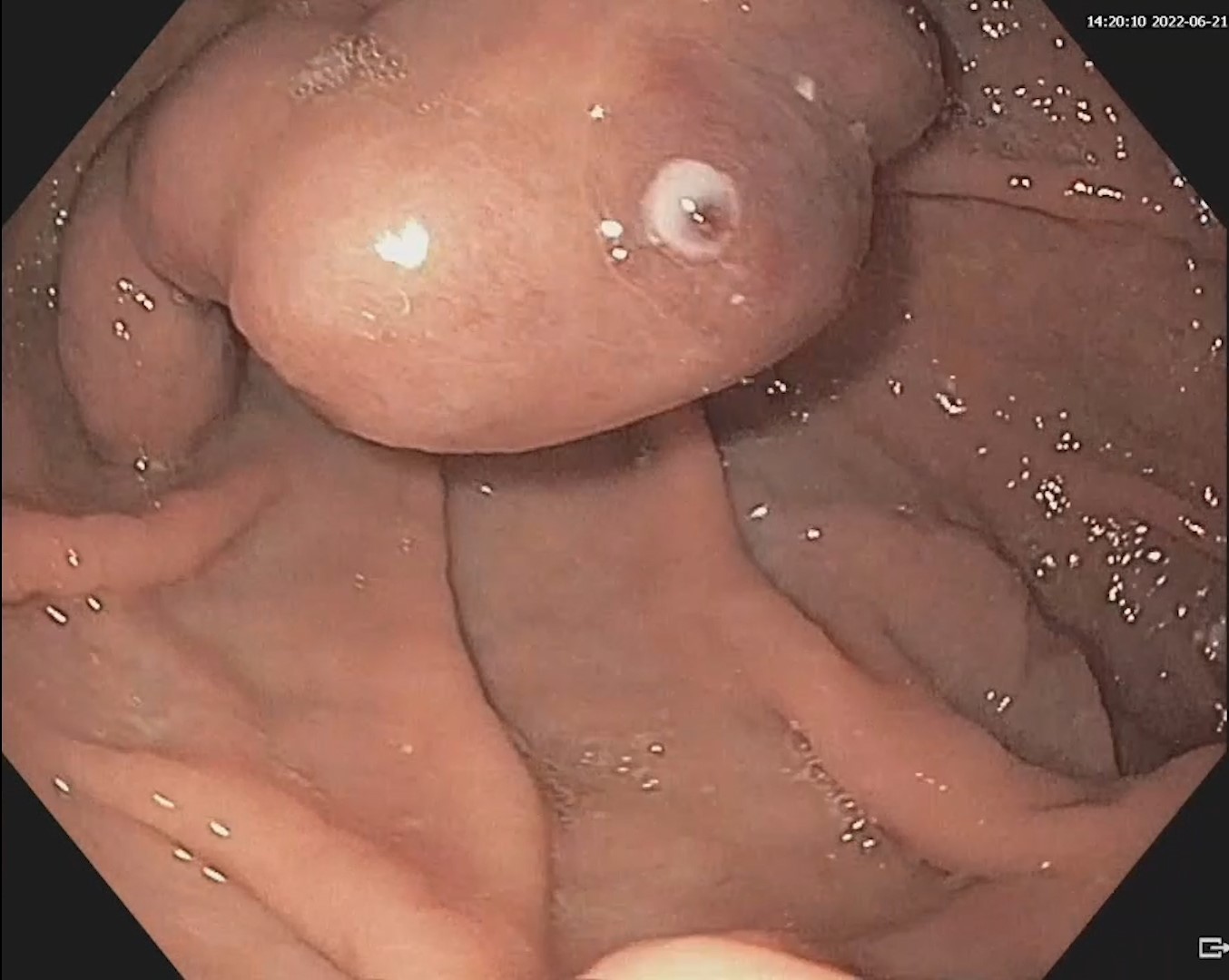
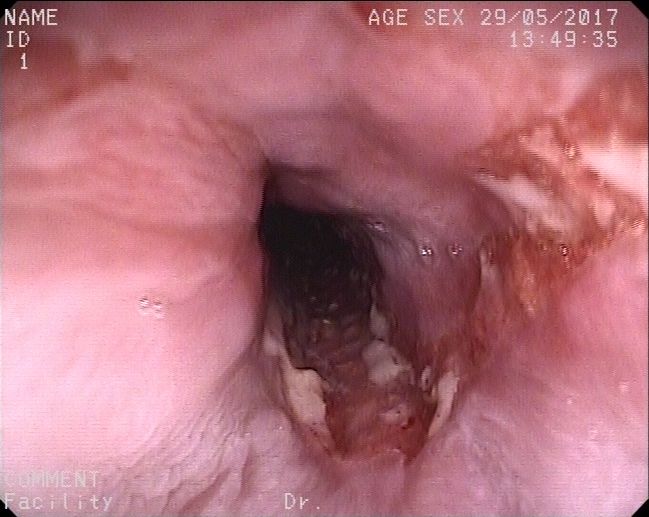
Colonoscopy identified a granular lateral spreading tumor, nodular-mixed type (LST-G-NM) of approximately 25/35 mm, located in the middle rectum (Fig. 1). The lesion was classified as Paris Is+IIA, KUDO IIIL, NICE 2 (JNET 2A) (Fig. 2). ”Piece-meal” endoscopic mucosal resection (p-EMR) was performed and the fragments were retrieved for pathological evaluation. At the end of the procedure, the visible vessels at the resection site were electrocoagulated with a Coagrasper forceps (Fig. 3,4).
The diagnosis was based on the histopathological evaluation of the resected specimen which revealed a tubulo-villous adenoma with low-grade and focal high-grade dysplasia.
Detailed assessment of lesion morphology through HD endoscopy with chromoendoscopy is mandatory before resection as it allows estimation of lesion histology and provides important information regarding the risk of submucosal invasion, granular nodular LST being associated with a 10% risk of submucosal invasion.
Endoscopic mucosal resection represents the method of choice for the removal of granular lateral spreading lesions (LST-G). The method requires submucosal injection of a solution that contains normal saline (or another type of plasma-expander), methylene blue and sometimes epinephrine. The purpose of the submucosal injection is separating the mucosal and submucosal planes from the muscularis propria in order to avoid a deep resection that involves a high risk of perforation. The use of methylene blue allows the delineation of the resection planes as it is selectively absorbed by the submucosa though not by the muscularis propria. Epinephrine is used for the prophylaxis of immediate bleeding in order to maintain a clean field of view; however, it does not prevent bleeding from large vessels and late postprocedural hemorrhage.
The resection may be completed in a single fragment (”en bloc”), when the size of the lesion allows this (usually in lesions of 20 mm or less), or through the piece-meal technique, in multiple fragments. pEMR has a good safety profile however it is associated with a 14-16% risk of lesion recurrence. Although less accesibile, endoscopic submucosal dissection (ESD) is superior to EMR regarding complete and en-bloc resection rates, being at the same time associated with lower recurrence risk.
Piece-meal EMR is the method of choice for the resection of LST lesions, particularly when ESD is not readily available.
- Kaltenbach T, Anderson JC, Burke CA, Dominitz JA, Gupta S, Lieberman D, Robertson DJ, Shaukat A, Syngal S, Rex DK. Endoscopic Removal of Colorectal Lesions: Recommendations by the US Multi-Society Task Force on Colorectal Cancer. Am J Gastroenterol. 2020 Mar;115(3):435-464
- Ferlitsch M, Moss A, Hassan C, Bhandari P, Dumonceau JM, Paspatis G, Jover R, Langner C, Bronzwaer M, Nalankilli K, Fockens P, Hazzan R, Gralnek IM, Gschwantler M, Waldmann E, Jeschek P, Penz D, Heresbach D, Moons L, Lemmers A, Paraskeva K, Pohl J, Ponchon T, Regula J, Repici A, Rutter MD, Burgess NG, Bourke MJ. Colorectal polypectomy and endoscopic mucosal resection (EMR): European Society of Gastrointestinal Endoscopy (ESGE) Clinical Guideline. Endoscopy. 2017 Mar;49(3):270-297.
- Russo P, Barbeiro S, Awadie H, Libânio D, Dinis-Ribeiro M, Bourke M. Management of colorectal laterally spreading tumors: a systematic review and meta-analysis. Endosc Int Open. 2019 Feb;7(2):E239-E259.
- Mathews AA, Draganov PV, Yang D. Endoscopic management of colorectal polyps: From benign to malignant polyps. World J Gastrointest Endosc. 2021 Sep 16;13(9):356-370.