See other cases
Pseudochist vs walled-off necrosis?
A 64-year-old man with a history of acute biliary pancreatitis 8 weeks ago, complicated with a peripancreatic fluid collection was referred for endoscopic assisted transgastric drainage.
Clinical: nausea, postprandial epigastric fullness
Biological: mild inflammatory syndrome (CRP=6mg/dL)
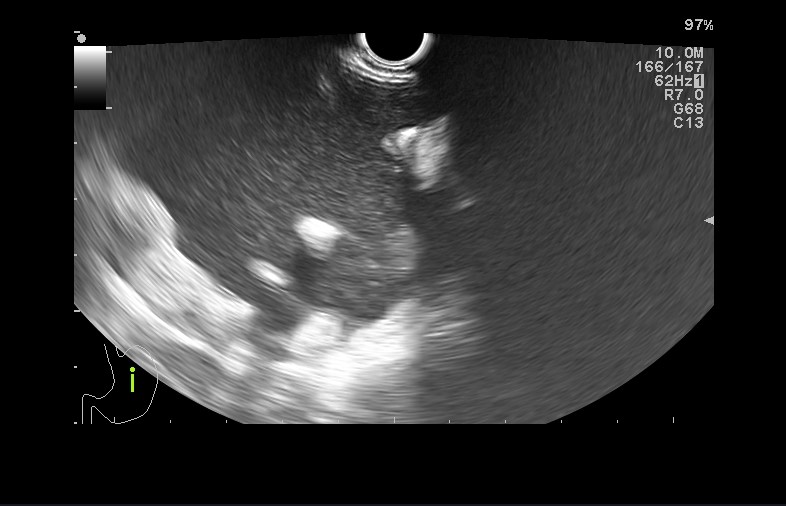
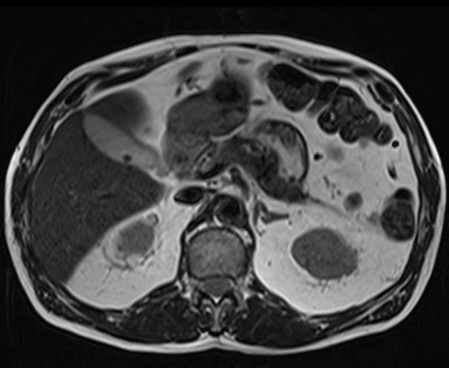
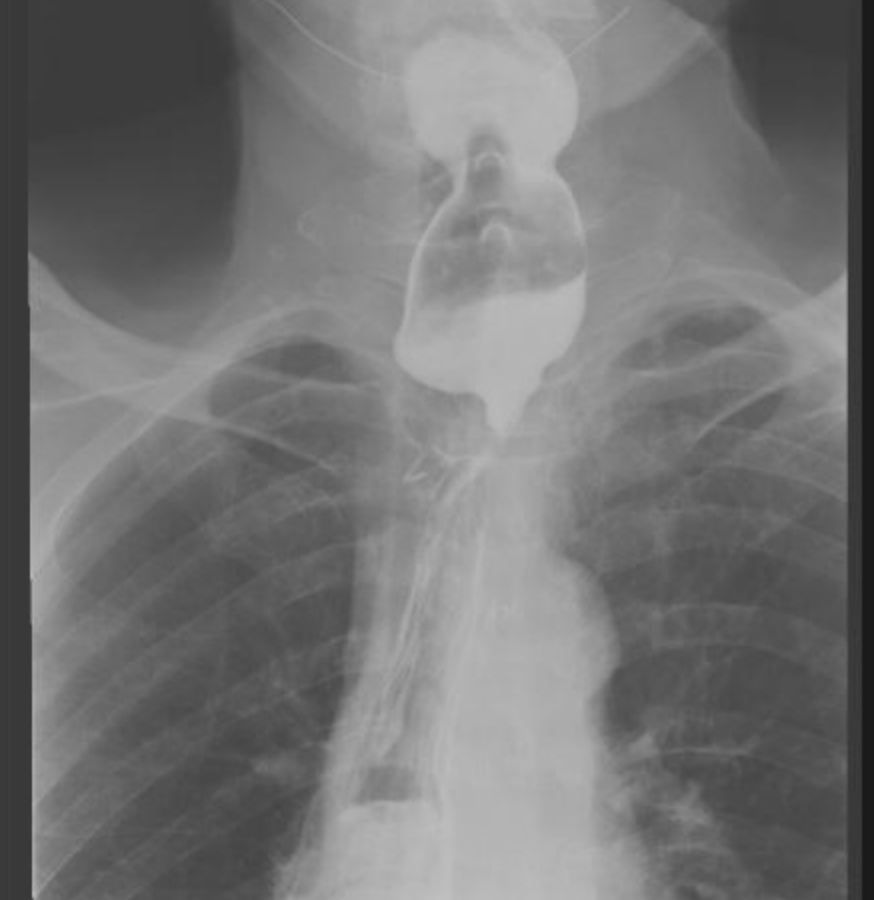
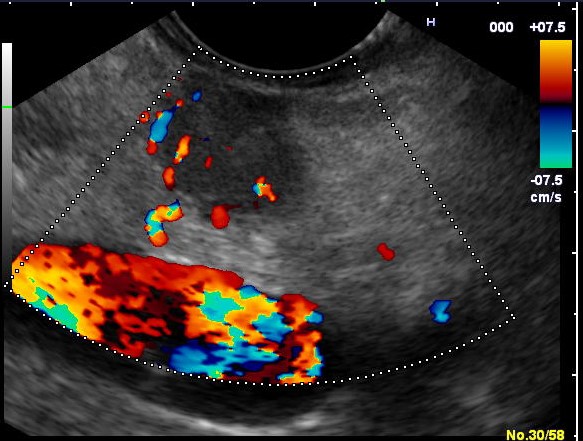
MRI was performed and described a peripancreatic fluid collection with possible necrotic debris included suggesting a pancreatic pseudocyst (Fig. 1 and 2).
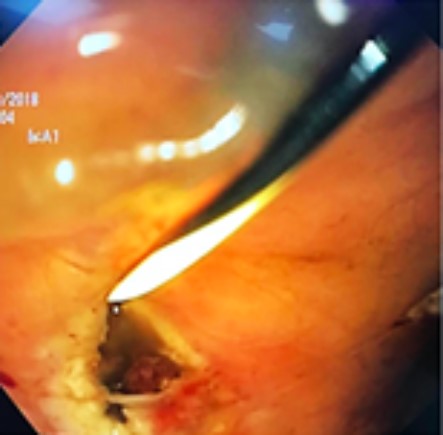
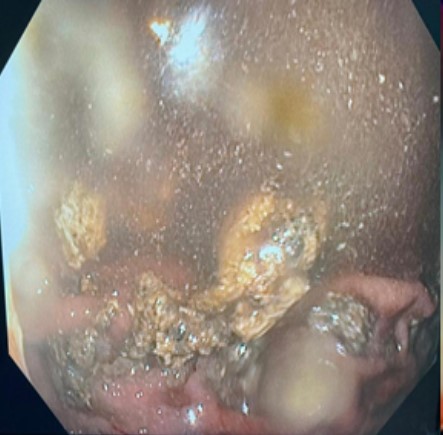
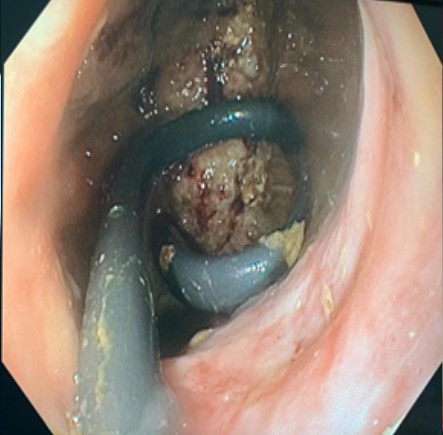
Initially interpreted as a pancreatic pseudocyst, a transgastric drainage was performed with the placement of a 10 Fr, 5 cm double-pigtail plastic stent (Fig 3, 4 and 5). Post-procedural the patient had an unfavorable evolution with fever and poor general state. Biological: leukocytosis with neutrophilia and marked inflammatory syndrome (leukocytes =19,000/mm3, CRP=150 mg/dL). Ultrasound revealed a peripancreatic collection with solid content. It was thus decided to practice endoscopic necrosectomy with prior dilation of the communication tract using a 10 mm CRE balloon. The polypectomy loop combined with constant lavage of the cavity was mainly used to extract the necrosis (Fig 6, 7, 8 and 9).
The patient showed a favorable clinical and biological evolution and the plastic stent was removed 6 months later.
Walled-off pancreatic necrosis.
Currently, the European Society of Gastrointestinal Endoscopy guidelines do not clarify the stent to be used for WON, while the American Gastroenterological Association favor the use of metal stents (LAMS) when necrosis is present. LAMS are preferred as they have a larger diameter, facilitating access inside the cavity in order to perform necrosectomy, if necessary. Because plastic stents are more cost-effective compared to LAMS, many experts prefer their use in pseudocyst drainage or WON with low content of necrotic material (below 10%).
There are still no well-defined criteria regarding the quantification of necrosis during EUS examination and the underestimation may also underestimate the need for necrosectomy. MRI in the T1 signal remains the investigation of choice for quantifying the necrotic content, but a good interpretation depends on the performance of the device, respectively on the experience of the examiner.
Additional studies are needed to standardize an algorithm for endoscopic ultrasound evaluation of peripancreatic collections as well as clear criteria regarding their therapeutic approach.
- Dorrell R, Pawa S, Pawa R. Endoscopic Management of Pancreatic Fluid Collections. J Clin Med. 2021 Jan 14;10(2):284.
- Yan L, Dargan A, Nieto J, Shariaha RZ, Binmoeller KF, Adler DG, DeSimone M, Berzin T, Swahney M, Draganov PV, Yang DJ, Diehl DL, Wang L, Ghulab A, Butt N, Siddiqui AA. Direct endoscopic necrosectomy at the time of transmural stent placement results in earlier resolution of complex walled-off pancreatic necrosis: Results from a large multicenter United States trial. Endosc Ultrasound. 2019 May-Jun;8(3):172-179.
- Bazerbachi F, Sawas T, Vargas EJ, Prokop LJ, Chari ST, Gleeson FC, Levy MJ, Martin J, Petersen BT, Pearson RK, Topazian MD, Vege SS, Abu Dayyeh BK. Metal stents versus plastic stents for the management of pancreatic walled-off necrosis: a systematic review and meta-analysis. Gastrointest Endosc. 2018 Jan;87(1):30-42.e15.