See other cases
Postoperative esophageal perforation
52-year-old smoker, hypertensive patient who underwent surgery for a ruptured aneurysm of the thoracic aorta 7 days before, is transferred for the endoscopic management of post-operative esophageal perforation.
Altered general condition, pale skin, rhythmic heart with 100 bpm, BP 105/60 mmHg, oxygen saturation 90% room air, abdomen without signs of peritoneal irritation, intrathoracic drain tubes in situ.
Biological: Hb 7.8, leukocytes 13k with neutrophilia, C reactive protein 120, serum albumin 2.80, Procalcitonin >10;
IV contrast CT scan revealed posterior, median and left paramedian mediastinum mixed collection with a drain tube in position, right pleurisy, right pleurostomy tube, left hydropneumothorax, pleurostomy tube with the distal end located at the level of the left pleura, pneumomediastinum and small size hydropneumopericardium. Oral contrast showed wide parietal tears in the middle and lower third of the thoracic esophagus, with the opacification of the mediastinal collection, left pleural fluid, and also of the trachea; contrast in both bronchial trees was suggestive of eso-bronchial/tracheal fistula.
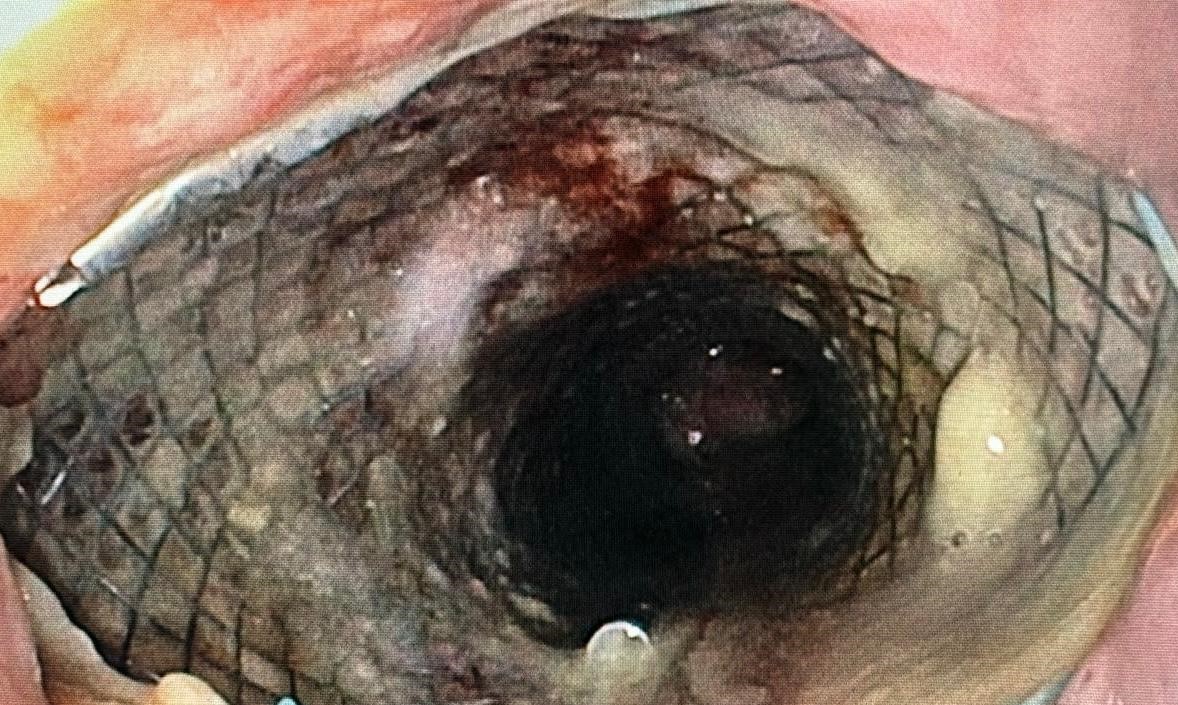
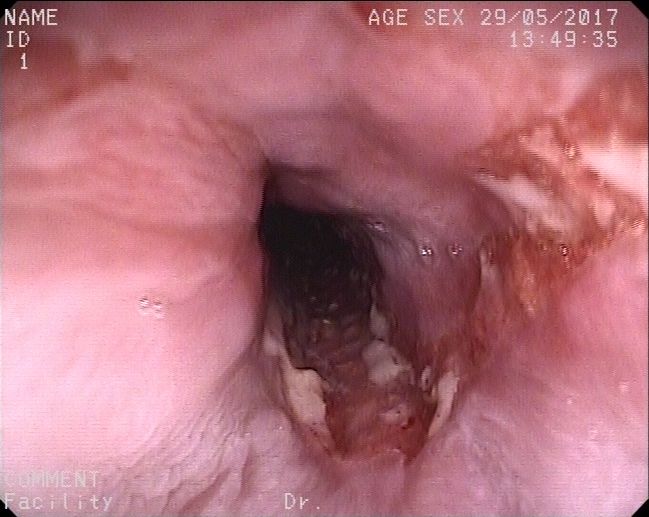
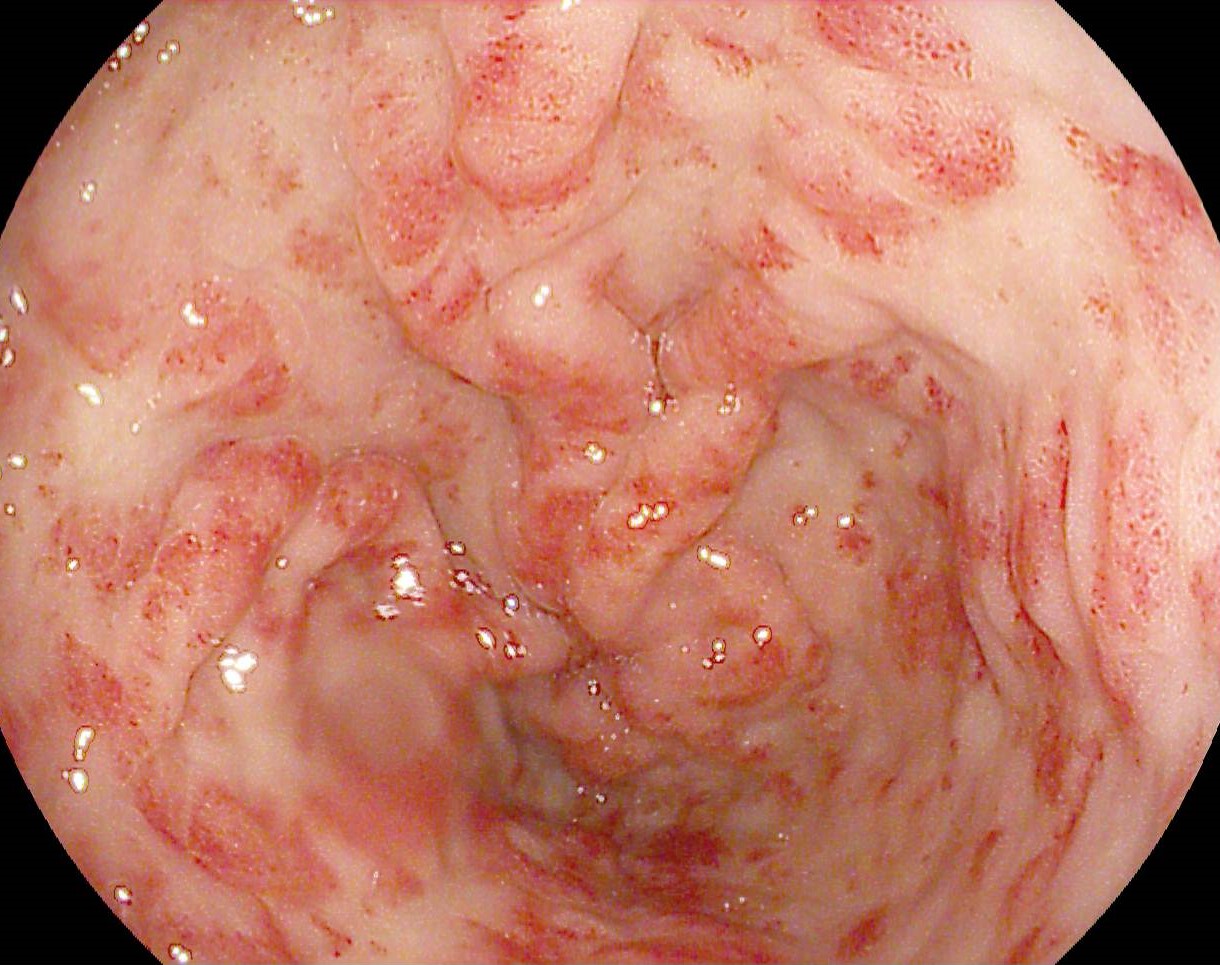
Upper digestive endoscopy with self-expanding metallic esophageal stents insertion: at approximately 28 cm from incisors – large eso-pleural/eso-mediastinal cavity, which extends to approximately 37 cm from incisors. Eso-gastric junction at approximately 42 cm from incisors. Stomach and duodenum without remarkable lesions.
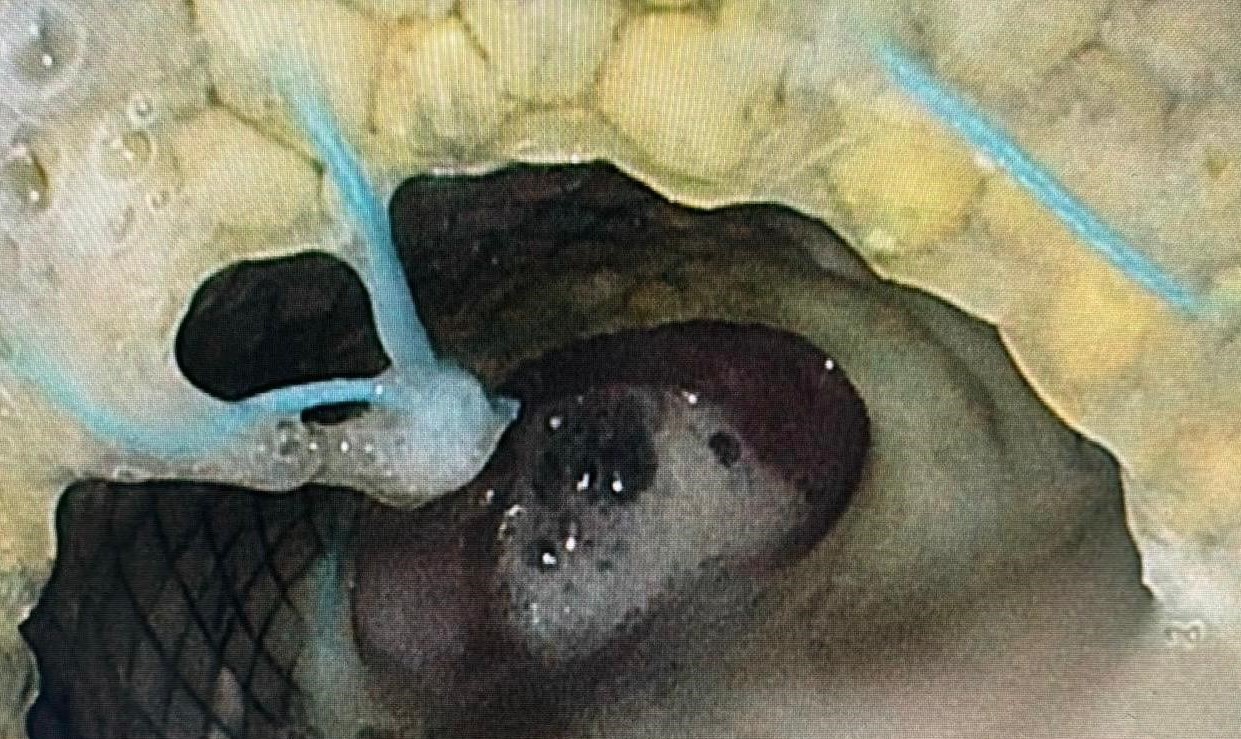
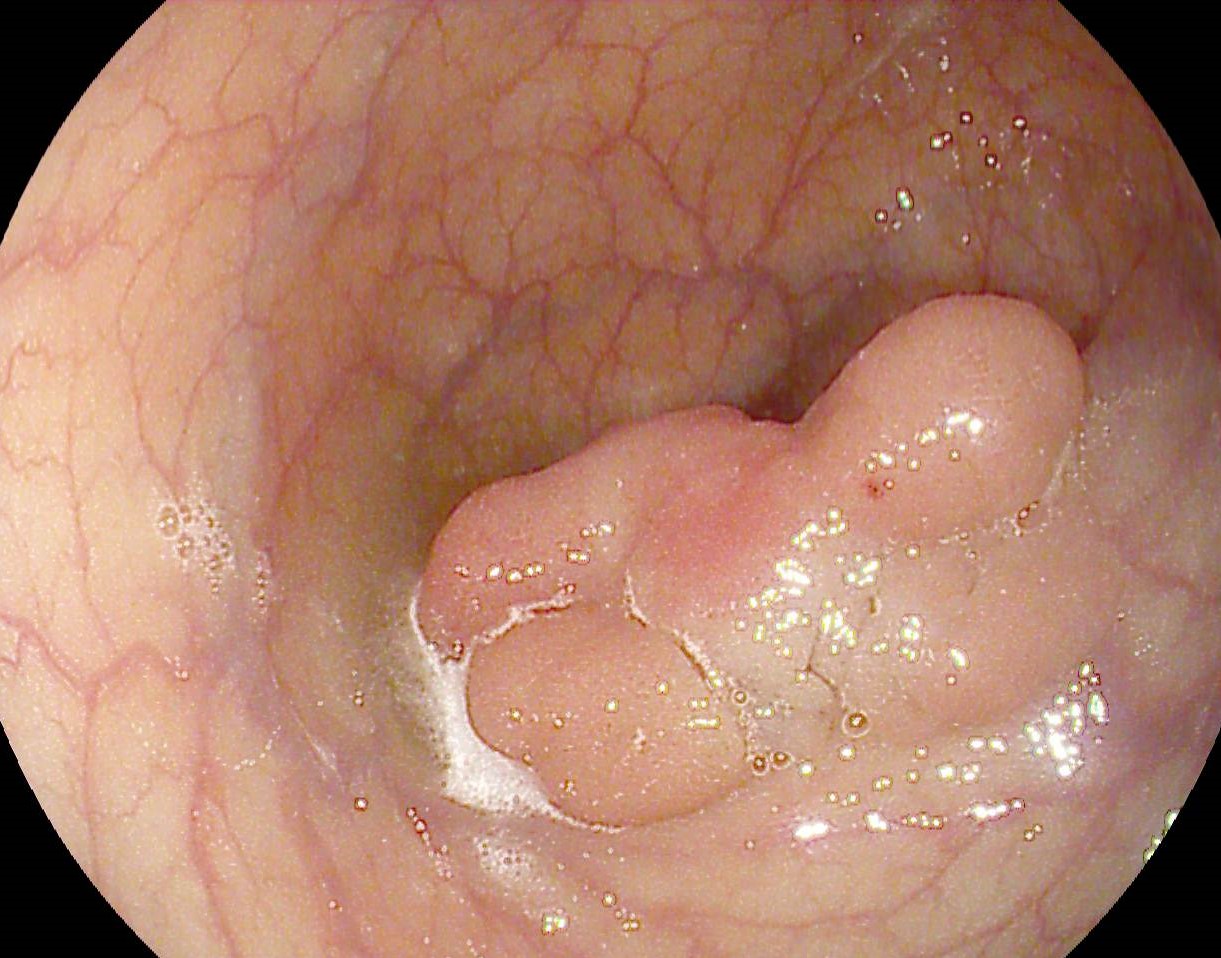
A Savary guidewire is inserted into the working channel of the endoscope, up to the level of the gastric antrum, then a 24/100 mm fully covered esophageal stent is pushed and expanded under endoscopic and radiological guidance. The proximal end of the stent is located 25 cm from the incisors. A second fully covered 24/100 mm esophageal stent, with antireflux valve, in continuity of the first esophageal stent (stent in stent) is inserted . The proximal end of the second esophageal stent is located 32 cm from incisors. Endoscopic control is carried out – the eso-pleuro-mediastinal fistula/perforation is no longer visible and fully expanded esophageal stents are in position
Treatment with broad-spectrum antibiotics, PPI, human albumin, analgesics, parenteral and oral nutrition is carried out with secondary improvement of the clinical status. Follow up CT scans with oral and IV contrast are carried out for control: esophageal stents in position, esophageal extravasation of the contrast material is no longer visible and the remission of the mediastinal collection, of the bilateral pleurisy and left hydropneumothorax is seen.
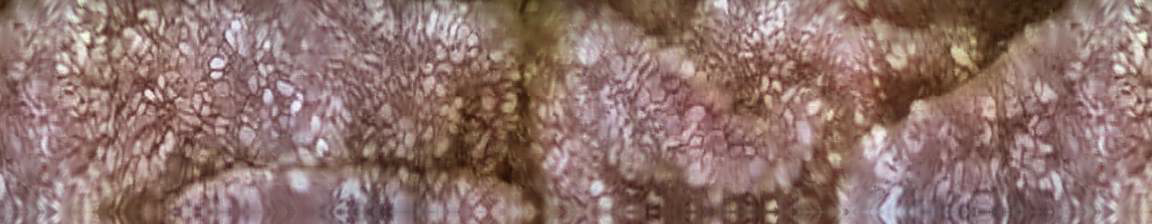
6 weeks after the insertion of the esophageal stents an upper digestive endoscopy is performed for endoscopic extraction with alligator forceps of the two esophageal stents; after extraction, the eso-pleuro-mediastinal fistula is no longer visible. Stomach, pylorus, duodenum I/II – normal appearance.
Control CT scan with iv and oral contrast post extraction of SEMS ( self expandable metal stents) reveals the absence of eso-pleuro-mediastinal fistula/perforation and the complete remission of the mediastinal collection, bilateral pleurisy and of the left hydropneumothorax.
Endoscopic management with SEMS insertion of postoperative eso-pleuro-mediastinal fistula/perforation.
Esophageal fistula/perforation represents a severe postoperative complication with increased mortality. Esophageal perforation can be approached endoscopically, the method varying according to location and size. Small defects, under 2 cm, can be closed with repositionable or OTSC clips, and the large ones can be addressed by inserting fully covered esophageal stents or applying vacuum therapy. Simultaneously, the patient can benefit from the placement of a percutaneous endoscopic gastrostomy feeding tube. Inserting an esophageal stent in a patient without esophageal obstruction is associated with an increased risk of migration, so anchoring the prosthesis with TTS / OTS type clips or inserting stent-in-stent is advisable. Also, if mediastinal or other localized collections are present, they must be surgically drained. The optimal duration of keeping the stents in position is not standardized, varying between 4 and 8 weeks, after which the prosthesis is removed endoscopically.
Fully covered esophageal stents can be used successfully in esophageal perforations of various causes. Due to the relatively high risk of migration, it is recommended that these stents be anchored with TTS/OTS clips.
- Spaander MCW, van der Bogt RD, Baron TH, et al. Esophageal stenting for benign and malignant disease: European Society of Gastrointestinal Endoscopy (ESGE) Guideline – Update 2021. Endoscopy. 2021;53(7):751-762