See other cases
Pancreatic pseudoaneurysm
A 59-year-old patient, a chronic alcohol abuser, with no medical history, presents with hematemesis and abdominal pain for the past 12 hours.
Clinical – stable, pallor, BP = 120/80 mmHG, no abdominal pain, no hepatosplenomegaly.
Biological – hemoglobin – 8.2 g/dL, normal RBC indices.
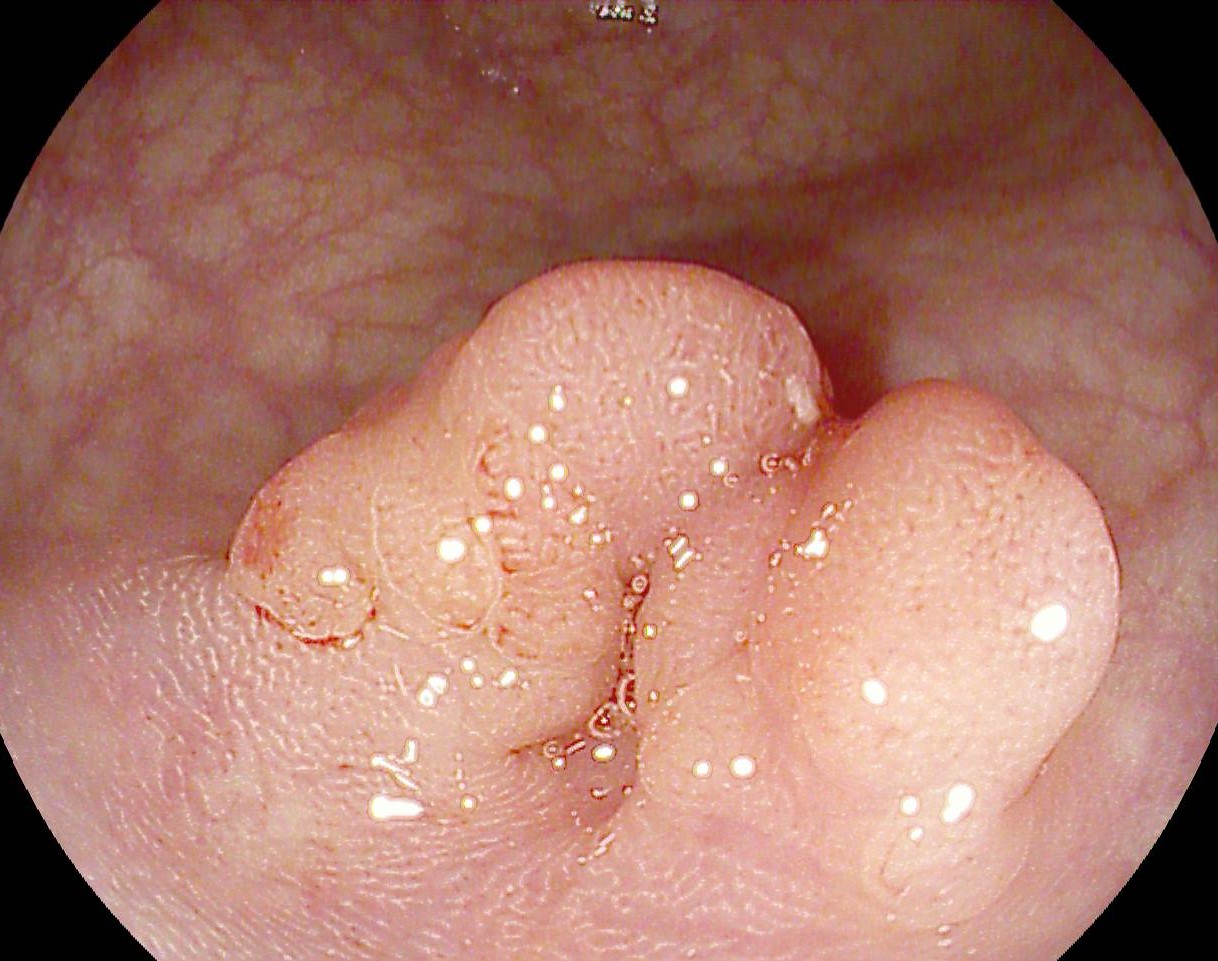
Emergency upper GI endoscopy revealed a large clot that almost completely occupied the esophageal lumen, which continued transcardially at the gastric level, occupying 2/3 of the gastric lumen up to the duodenal angle.
Endoscopic reevaluation at 24 h:esophagus and stomach with free lumen, gastric body with extrinsic compression on the greater curvature and intensely edematous mucosa at that level.
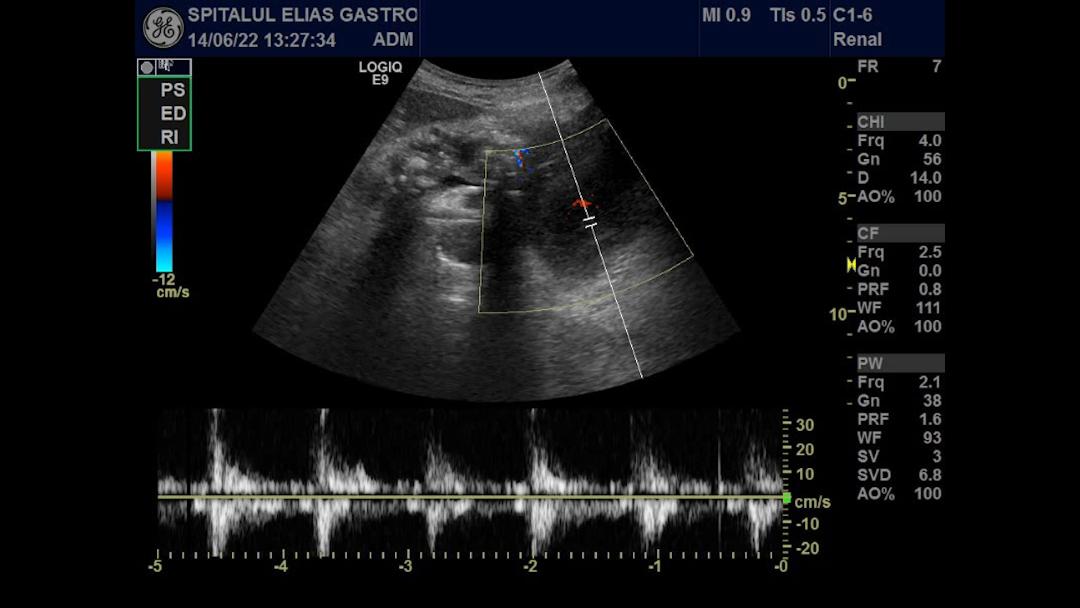
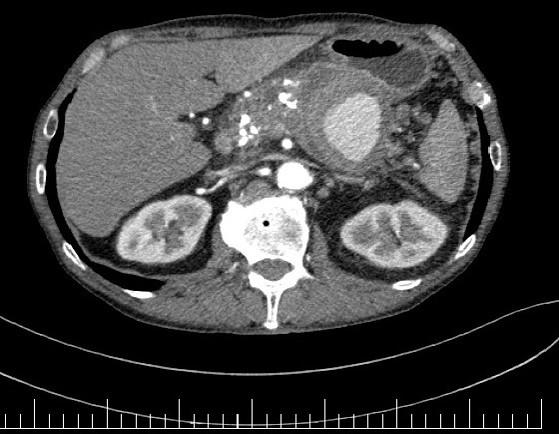
Abdominal ultrasound revealed multiple calcifications at the pancreatic head and body (lesions compatible with chronic pancreatitis), and a cystic formation of approximately 5 cm in the pancreatic tail, with a pulsed Doppler signal (Fig 1).
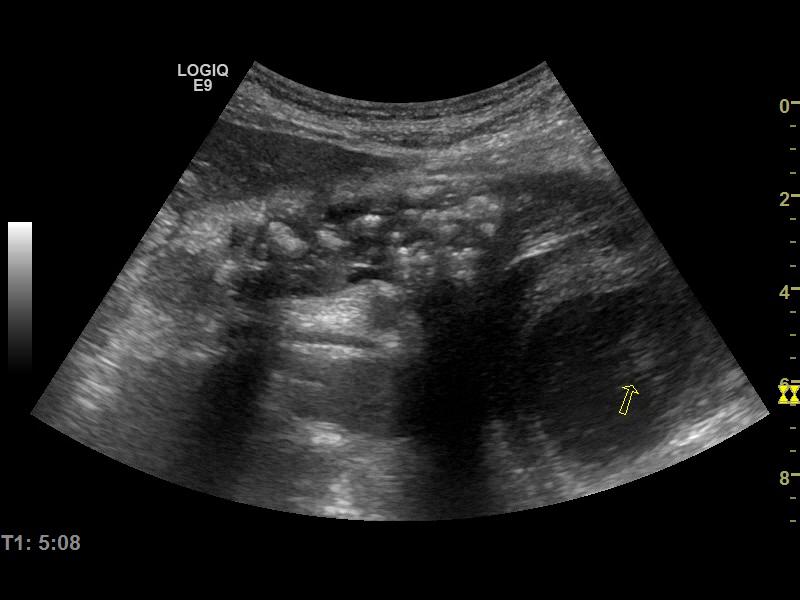
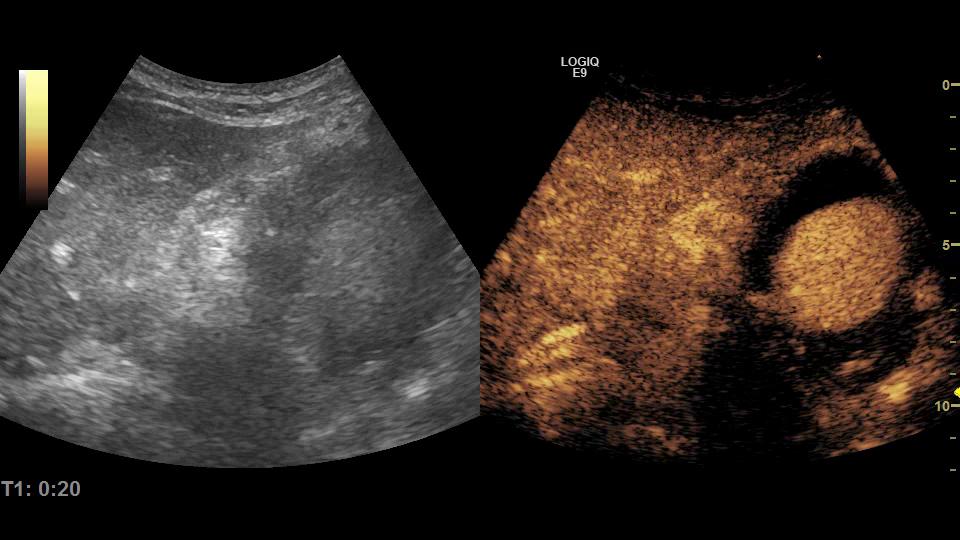
CEUS : the cyst showed arterial hyperenhancement in the center and absence of contrast in the periphery, with the same aspect in the portal and parenchymal phases (Fig 2 & 3).
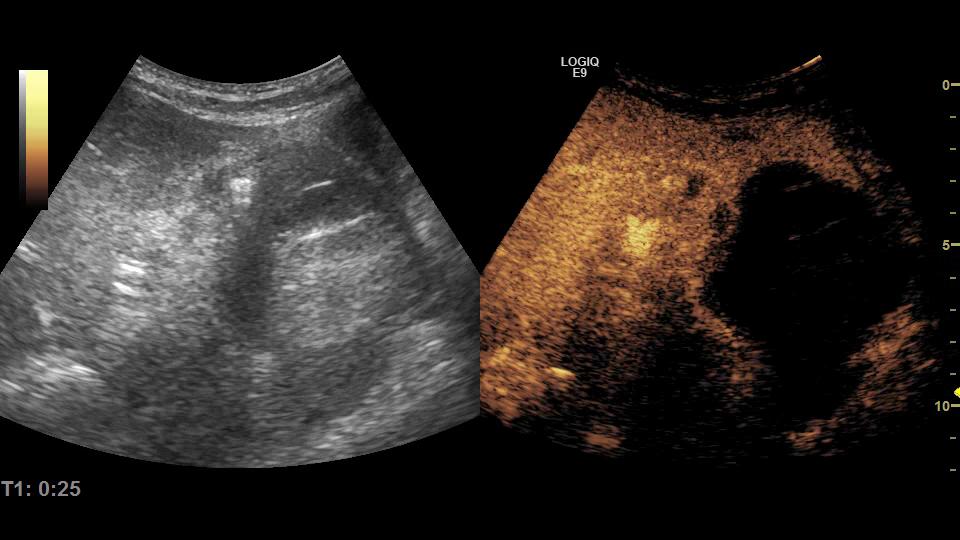
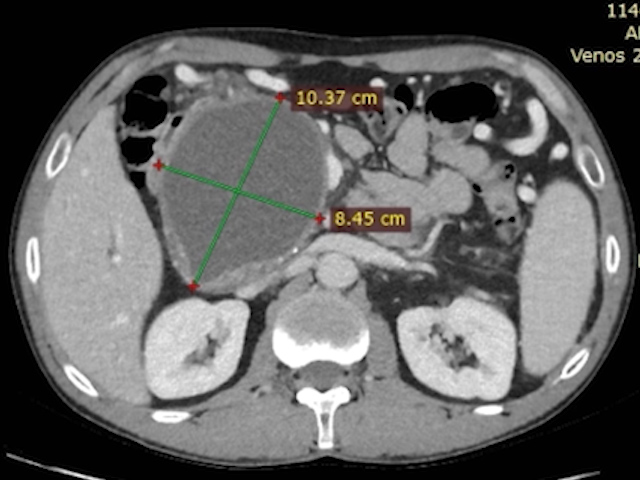
Abdominal and pelvic CT scan with contrast: in the pancreatic tail, a pseudoaneurysm of the splenic artery about 65/68/67 mm was revealed, with parietal thrombosis with a stratified appearance, which involved about 40% of the lumen, where contrast extravasations were highlighted (Fig 4), in direct contact with the geater curvature in the area of the gastric angle and chronic splenic vein thrombosis.
There was a suspicion of upper digestive bleeding secondary to a fistula between the pseudo-aneurysm of the splenic artery and the stomach, but also the possibility of a wirsungorrhagia, given the direct contact of the lesion with the pancreatic tail.
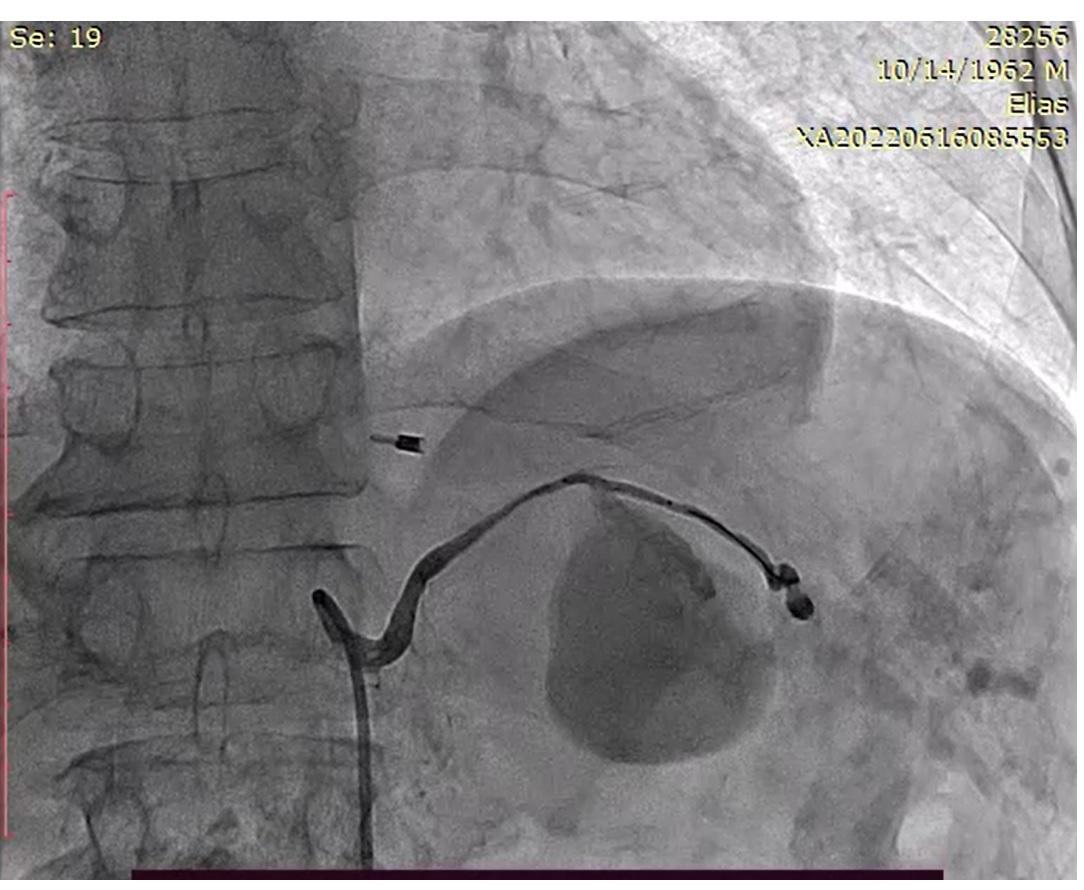
Abdominal angiography was performed, which revealed extravasation of the contrast substance at the splenic artery (Fig 5). Angioplasty was performed with a 3/18 mm Bentley type stent graft, with an optimal result, without extravasation of contrast and maintaining arterial patency (Fig 6).
CEUS reevaluation at 72h: hypoechoic mass, with no enhancement in the arterial phase, an aspect that was also maintained in the portal and parenchymal phase (Fig. 7 & 8).
Upper gastrointestinal bleeding secondary to a splenic artery pseudoaneurysm. Chronic ethanolic pancreatitis.
The case illustrates the multidisciplinary management of a rare cause of gastrointestinal bleeding.
Bleeding from splenic artery pseudoaneurysm is a rare and often fatal cause of gastrointestinal bleeding. Aneurysms of the splenic artery are the 3rd most common cause of intra-abdominal aneurysm after those of the aorta and iliac arteries, more common in men (4:1). By definition, an aneurysm has a wall consisting of intima, media, and adventitia, as opposed to a pseudo-aneurysm that consists of only intima and media. The most common causes are pancreatitis and abdominal trauma. In pancreatitis, pancreatic enzymes can cause vascular necrosis and rupture of the elastic tissue, leading to pseudoaneurysm formation. Another way can be through pseudocysts (41% of patients with pseudoaneurysms), through vascular erosion but also through direct compression which can cause ischemia.
In this patient’s case, the pseudoaneurysm most likely occurred secondary to a pseudocyst that eroded the splenic artery, with intracystic hemorrhage, which led to a localized hemorrhage and not to a hemoperitoneum, and subsequentlybled into the digestive tract, either transgastric or through the main pancreatic duct.
After stent placement by angiography, the patient had normal stools, with a favorable evolution at ultrasound re-evaluation at 1 month, with ultrasound remission of the mass.
1.Piscaglia F, Nolsøe C, Dietrich CF, Cosgrove DO, Gilja OH, et al. The EFSUMB Guidelines and Recommendations on the Clinical Practice of Contrast Enhanced Ultrasound (CEUS): update 2011 on non-hepatic applications. Ultraschall Med. 2012 Feb;33(1):33-59.
2. Massani M, Bridda A, Caratozzolo E, Bonariol L, Antoniutti M, Bassi N. Hemosuccus pancreaticus due to primary splenic artery aneurysm: a diagnostic and therapeutic challenge. JOP. 2009 Jan 8;10(1):48-52.
3. Maharaj R, Raghunanan B, Mohammed W, Rambally R, Sookdeo VD, Harnanan D, Warner WA. A rare case of massive lower gastrointestinal bleeding from a ruptured splenic artery aneurysm. J Surg Case Rep. 2018 Feb 3;2018(2):rjy003.
4. Al-Habbal Y, Christophi C, Muralidharan V. Aneurysms of the splenic artery—a review. Surgeon 2010;8:223–31.
5. Ierardi AM. Endovascular retreatment of a splenic artery aneurysm refilled by collateral branches of the left gastric artery: a case report. J Med Case Reports 2014;8:436.
6. Tessier DJ, Stone WM, Fowl RJ et al: Clinical features and management of splenic artery pseudoaneurysm: case series and cumulative review of literature. J Vasc Surg, 2003; 38(5): 969–974.