See other cases
Pancreatic NETs: Diagnostic Challenges and Management
A 51-year-old female patient with a medical history of thrombophilia (Factor V Leiden mutation) presented for evaluation after an incidental finding of a pancreatic lesion.
Clinical: There were no reports of abdominal pain, jaundice, or weight loss.
Biological: Routine blood work was unremarkable, with no signs of abnormal liver function or significant elevations in tumor markers (CA 19-9 and CEA within normal ranges).
Previously, an abdominal ultrasound revealed an inhomogeneous hypoechoic lesion measuring 25 x 25 x 25 mm in the head of the pancreas. Subsequent imaging with CT and MRI confirmed the lesion, which remained stationary in size. The patient underwent three separate endoscopic ultrasound-guided fine needle aspiration (EUS-FNA) procedures, none of which provided conclusive diagnostic results. The first procedure was complicated by acute pancreatitis, and none of the FNA samples provided a conclusive diagnosis. There was a suggestion of a serous cystadenoma based on imaging findings.
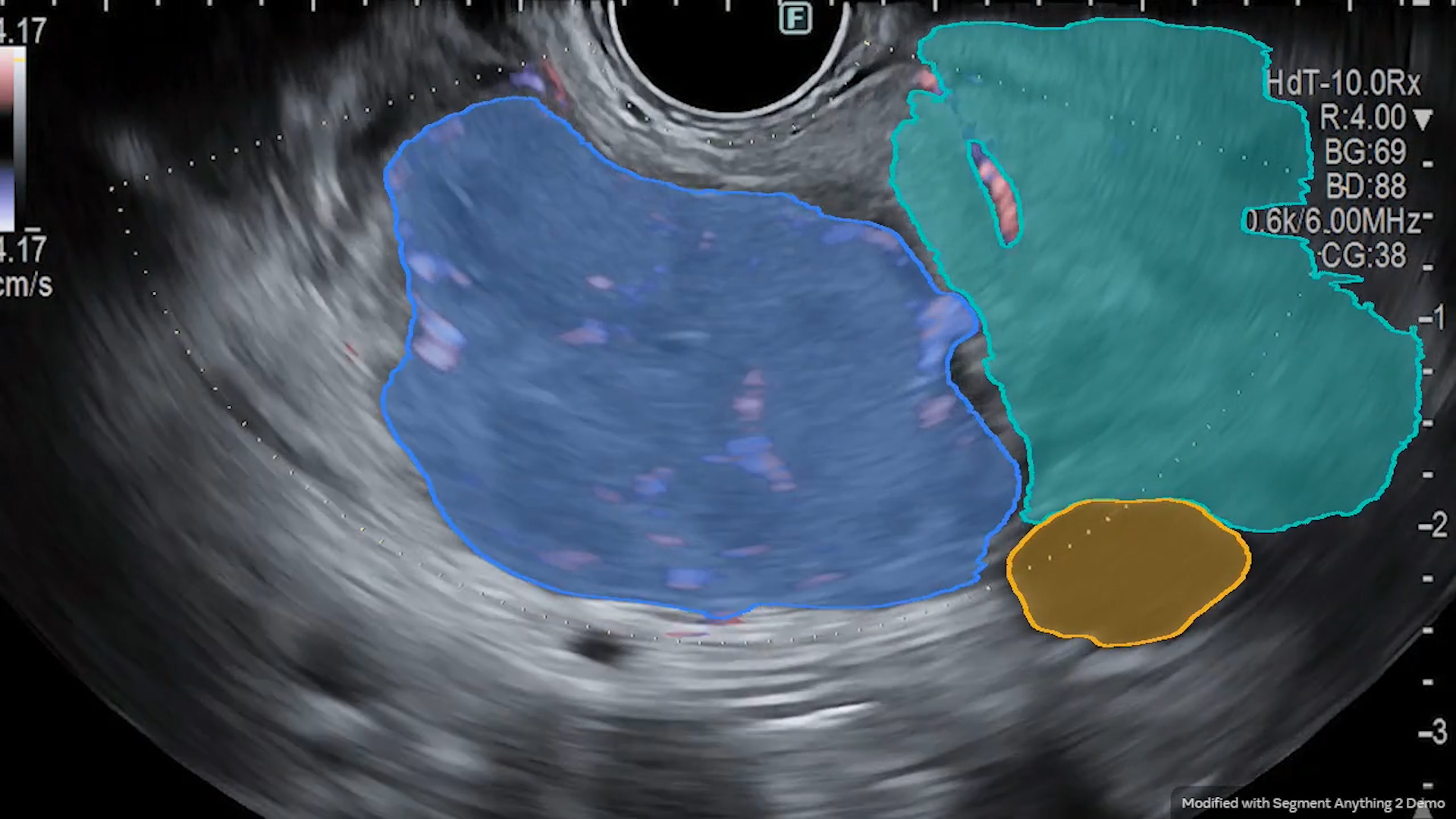
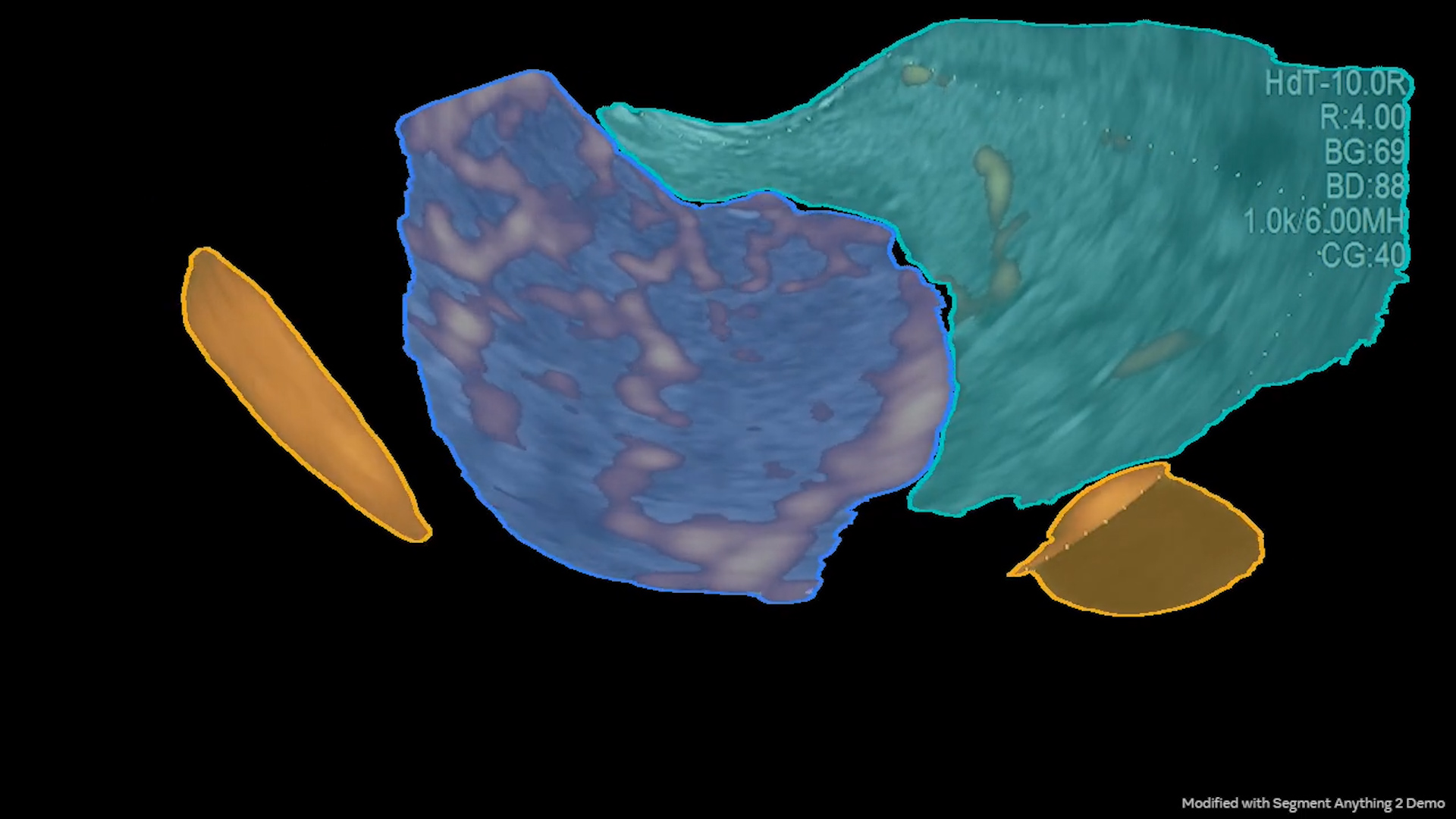
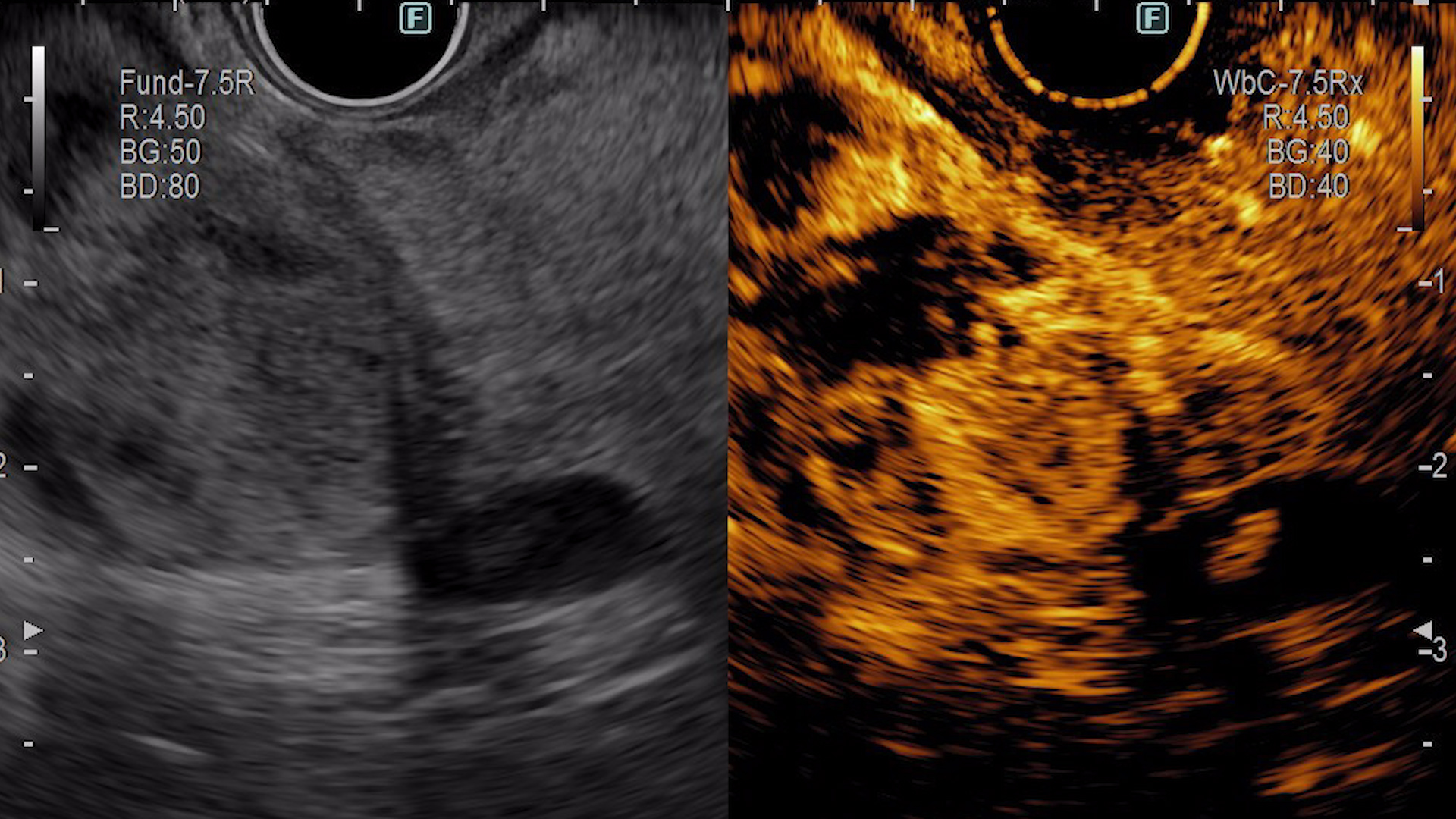
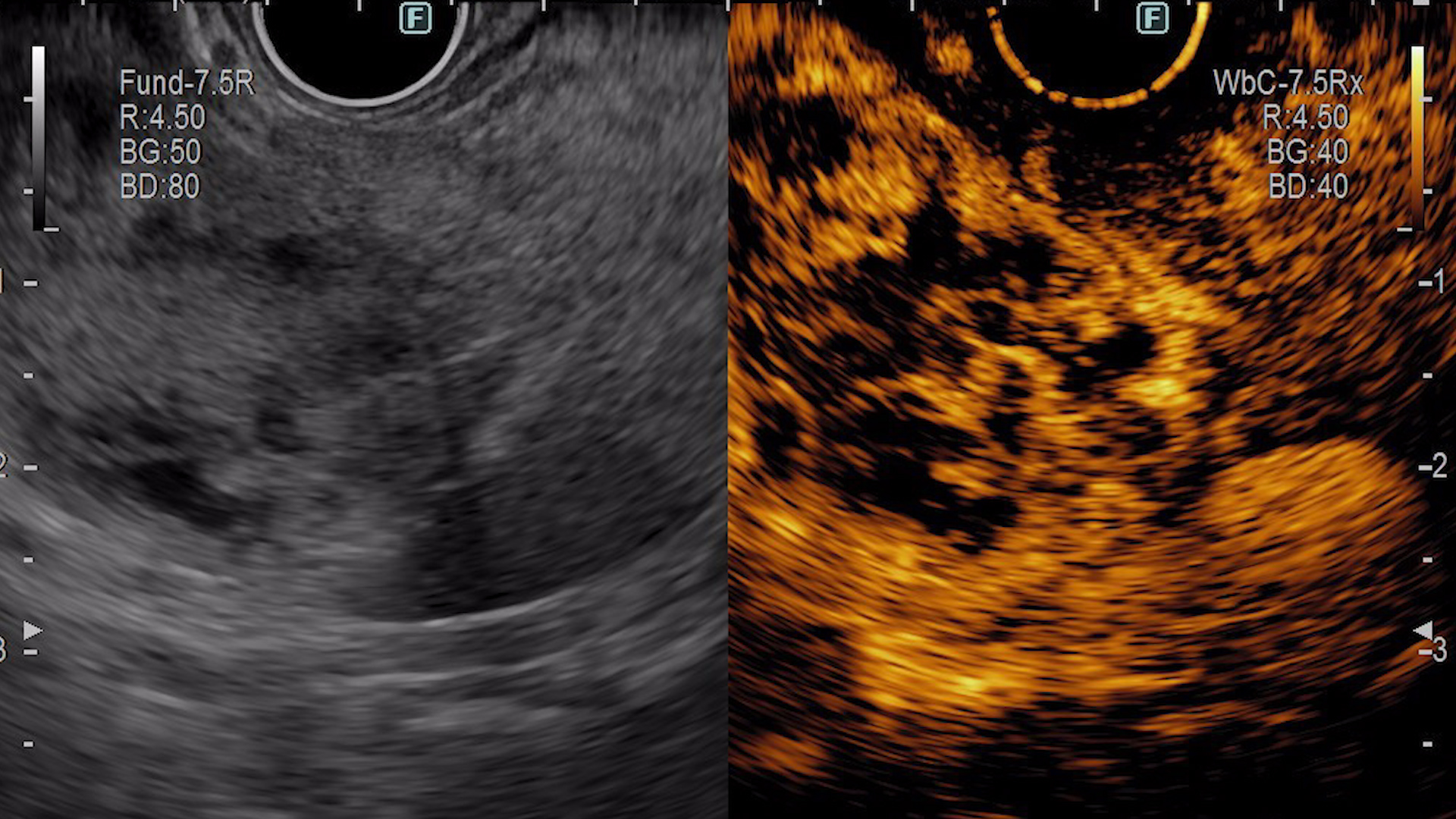
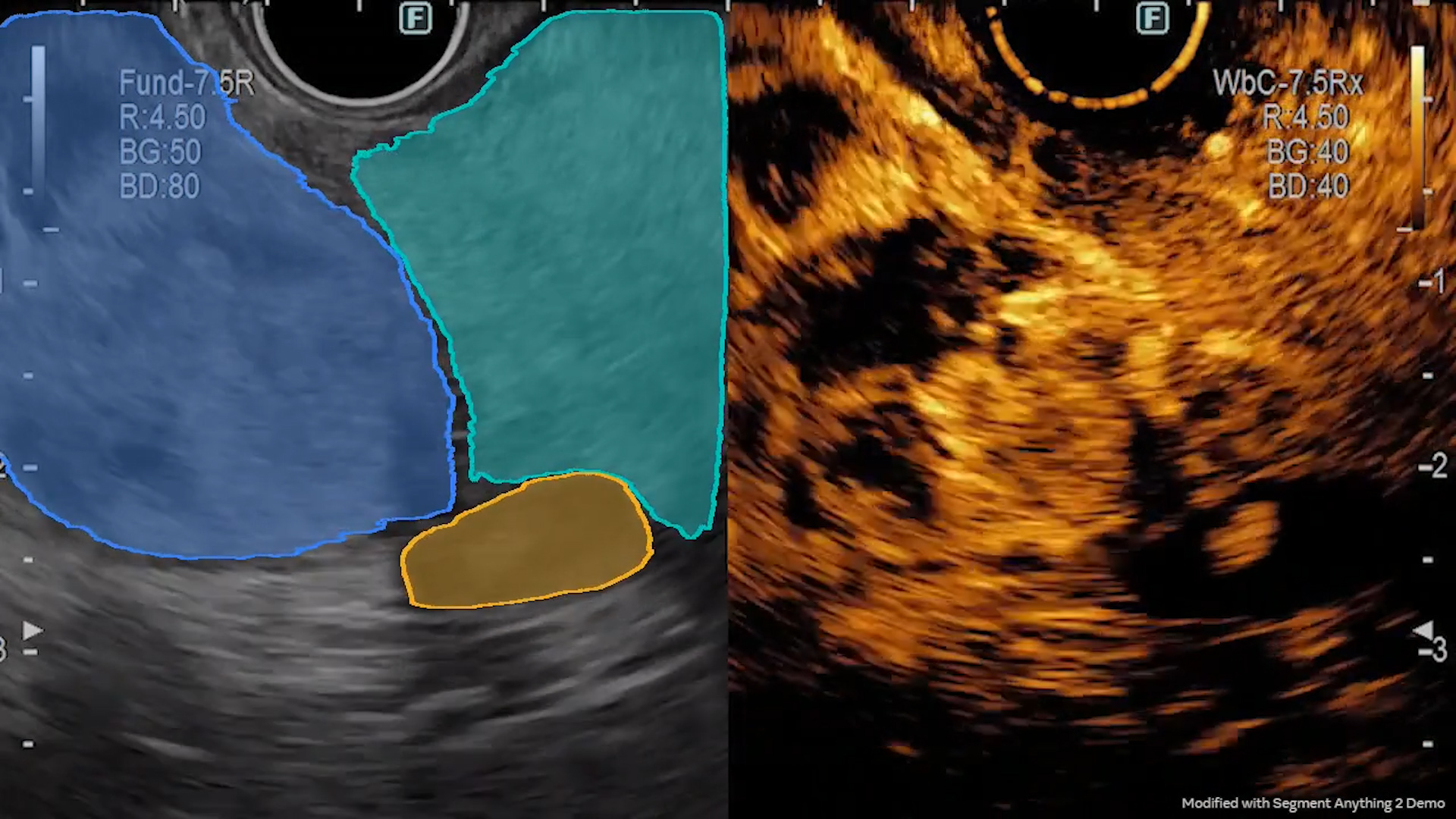
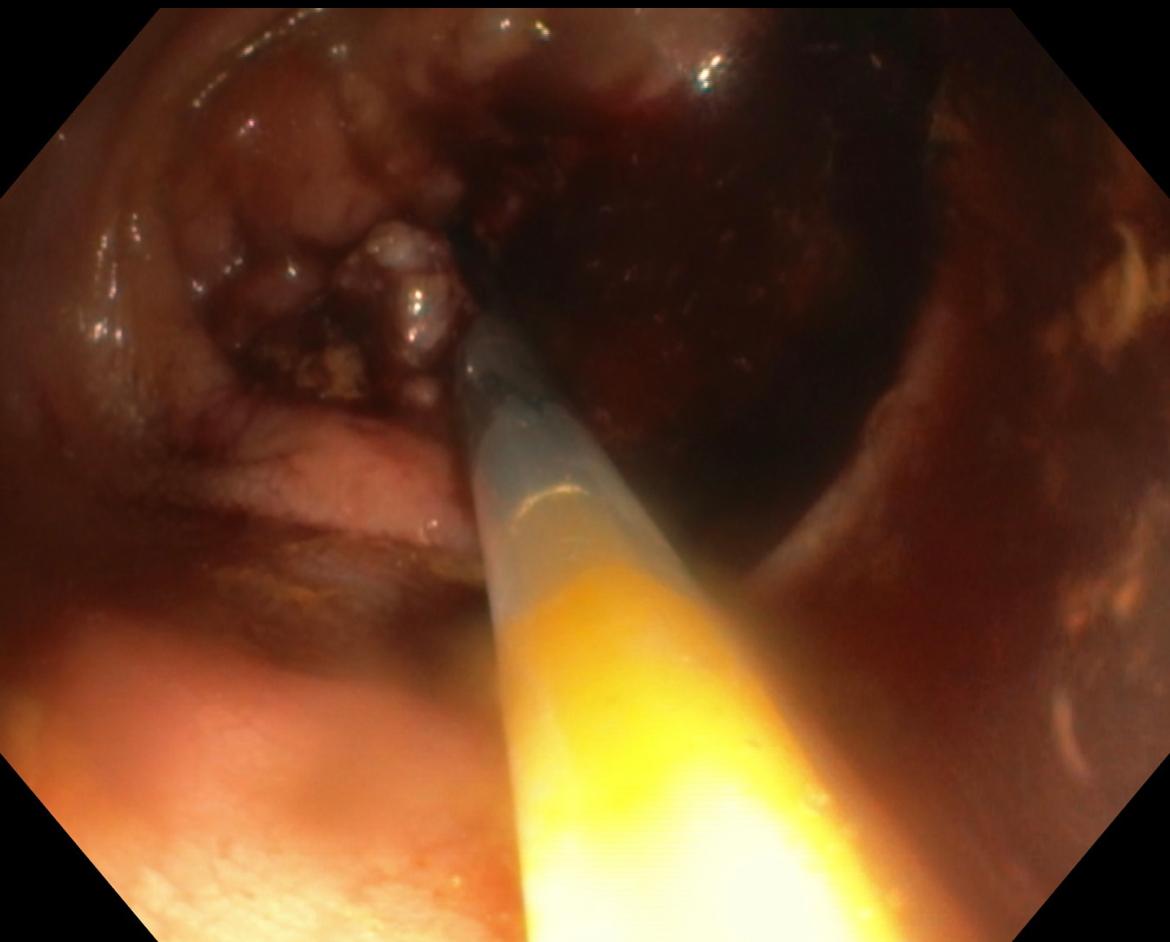
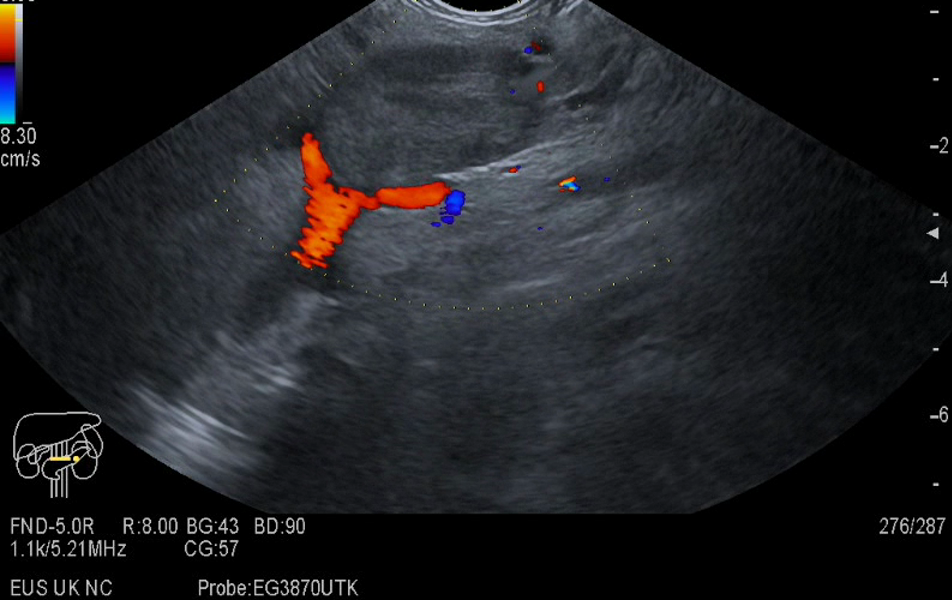
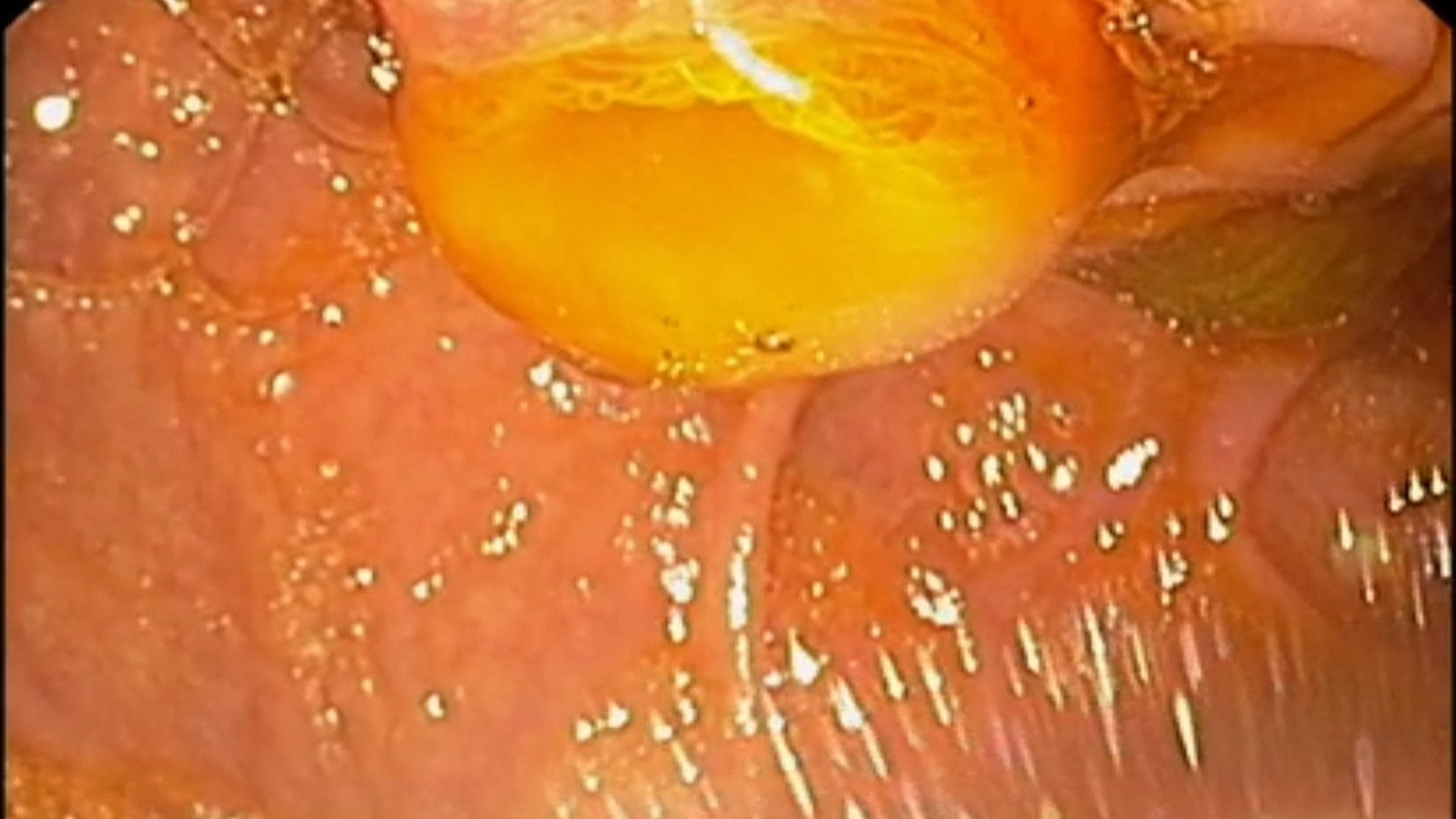
B-mode ultrasound (EUS) was repeated (Figure 1), including color Doppler (Figure 2) and power Doppler (Figure 3) examinations. Endoscopic ultrasound examination with contrast material indicated hyperenhancing appearance in the early arterial phase with areas of necrosis (Figure 4), followed by wash-out in the late venous phase (Figure 5). Subsequent EUS-guided fine needle biopsy (EUS-FNB) was performed, revealing the following immunohistochemical profile: AE1/AE3 positive, synaptophysin positive, chromogranin positive, NSE positive, SSTR2 positive, Ki67 4-5%, Congo Red negative.
Pancreatic neuroendocrine tumor (NET) G1/G2.
Pancreatic neuroendocrine tumors (NETs) are a rare subset of pancreatic neoplasms that arise from the hormone-producing cells of the pancreas. They can present as incidental findings during imaging for unrelated reasons. While most pancreatic NETs are slow-growing and have a favorable prognosis, some may exhibit malignant potential, especially if they are larger in size or have a higher Ki67 index.
The lesion in this case was initially suggested to be a serous cystadenoma based on imaging and EUS-FNA findings, but the eventual immunohistochemistry profile strongly indicated a pancreatic NET. The Ki67 index (4-5%) suggests a tumor of intermediate grade (G1/G2), and positive staining for synaptophysin, chromogranin, and SSTR2 further confirmed the neuroendocrine origin.
Management of pancreatic NETs depends on tumor size, location, grade, and functional status. In this case, surgical resection is recommended due to the lesion’s size, hypervascularity, and the patient’s history of acute pancreatitis, which may suggest a risk of future complications.
Recommended Management Plan:
• Immediate Surgical Referral
Surgical resection is recommended for both definitive diagnosis and treatment. Given the lesion’s size, characteristics, and immunohistochemistry profile, there is a concern for potential malignancy, making surgery the most appropriate option.
• Multidisciplinary Discussion
In cases where there is hesitancy regarding surgical intervention due to the patient’s condition or other risk factors, a multidisciplinary discussion involving gastroenterology, surgery, and oncology teams is crucial. This could help weigh the benefits of surgery versus other therapeutic options, such as radiofrequency ablation (RFA) or re-biopsy. However, given the current findings, surgical resection remains the most likely recommendation.
• Follow-up and Monitoring
Post-surgery, regular follow-ups with monitoring of tumor markers, imaging, and possibly serial Ki67 assessment will be necessary to ensure there is no recurrence or progression. For pancreatic NETs, ongoing surveillance is critical, particularly for those with intermediate-grade tumors (G1/G2).
Pancreatic neuroendocrine tumors are rare but carry a risk of malignancy depending on the grade and size. This case highlights the importance of thorough immunohistochemical evaluation following inconclusive FNA results. Surgical resection is the preferred treatment option in this case, offering both diagnostic clarity and therapeutic benefit. Regular follow-up is essential to monitor for recurrence or progression.
- Kos-Kudła B, Castaño JP, Denecke T, Grande E, Kjaer A, Koumarianou A, de Mestier L, Partelli S, Perren A, Stättner S, Valle JW, Fazio N. European Neuroendocrine Tumour Society (ENETS) 2023 guidance paper for nonfunctioning pancreatic neuroendocrine tumours. J Neuroendocrinol 2023; 35(12): e13343. doi: 10.1111/jne.13343. PMID: 37877341 DOI: 10.1111/jne.13343
- Ravi Nk, Gabeur V, Hu YT, Hu R, Ryali C, Ma T, et al. SAM 2: Segment Anything in Images and Videos. 2024: arXiv preprint arXiv:2408.00714 (https://arxiv.org/abs/2408.00714)