See other cases
Cyst vs pseudocyst
We present the case of a 43-year-old woman with emergency surgery for a hemorrhagic ovarian cyst, with intraoperative biopsy of a pancreatic cystic formation, followed by 2 episodes of acute pancreatitis, with the formation in 3 months of a pseudocyst of approx. 7 cm, in the vicinity of the pancreatic corporeal cyst formation (IPMN – intrapapillary mucinous neoplasm) (Figure 1).
Pain in the upper abdominal floor, nausea, vomiting.
Leukocytes count 10 000/mm3, serum amylase 138 IU/mL, serum lipase 1267 IU/mL.
Abdominal CT scan + MRI: 2 adjacent cystic formations (suggestive of IPMN and pseudocyst, both communicating with the duct of Wirsung which was dilated towards the tail of the pancreas!).
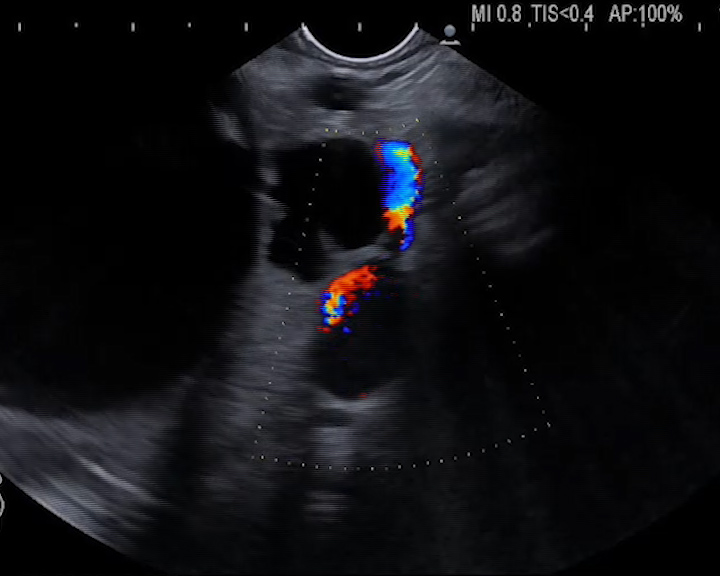
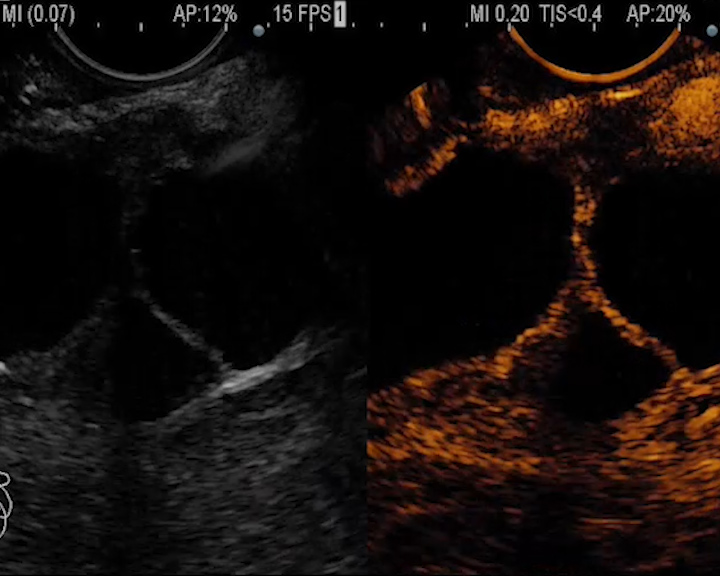
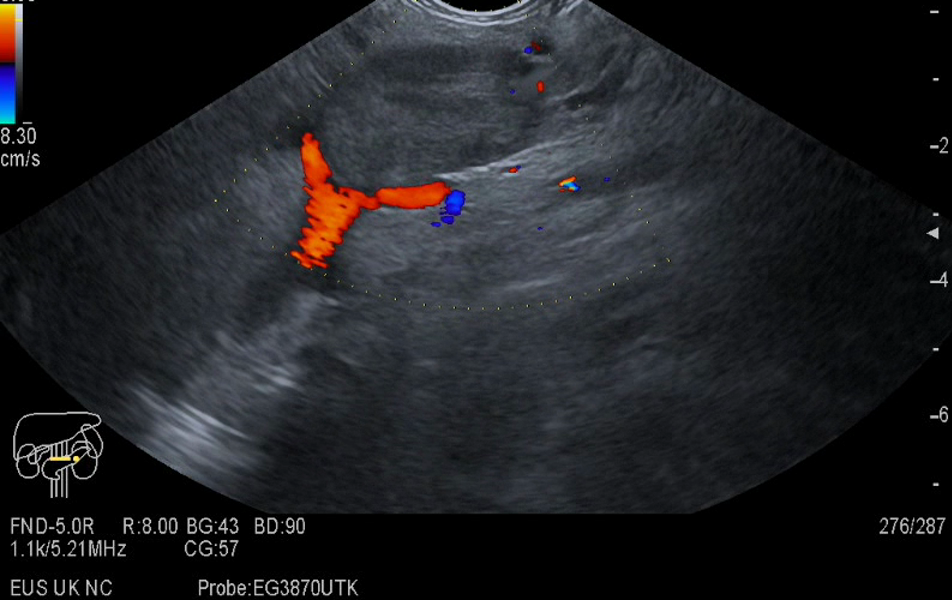
The patient was referred for contrast-enhanced endoscopic ultrasound (CE-EUS), followed by endoscopically guided drainage of the pseudocyst (Movie 1). CE-EUS (Sonovue 4.8 mL) revealed a cystic, multi-loculated pancreatic body tumor of approx. 3 x 2.5 cm, with septa inside, which captured the contrast substance suggestive of mucinous neoplasm (IPMN), thus allowing clear differentiation from pseudocyst (Figure 2). The cystic tumor was in contact with the splenic artery and vein.
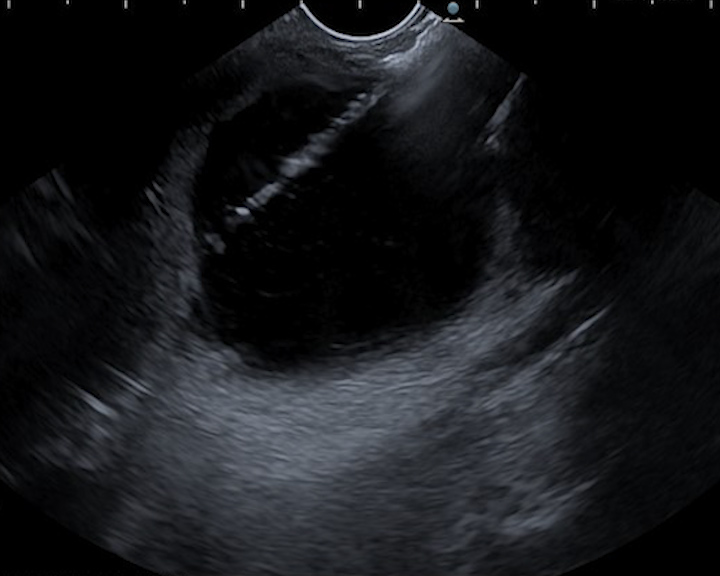
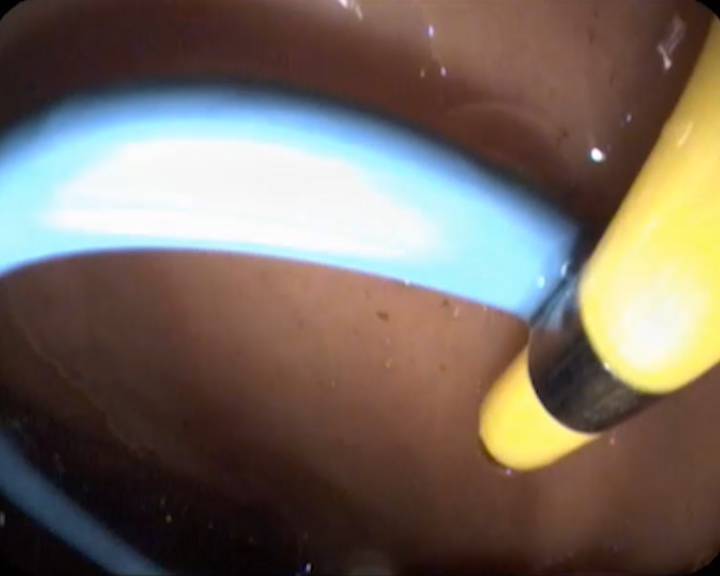
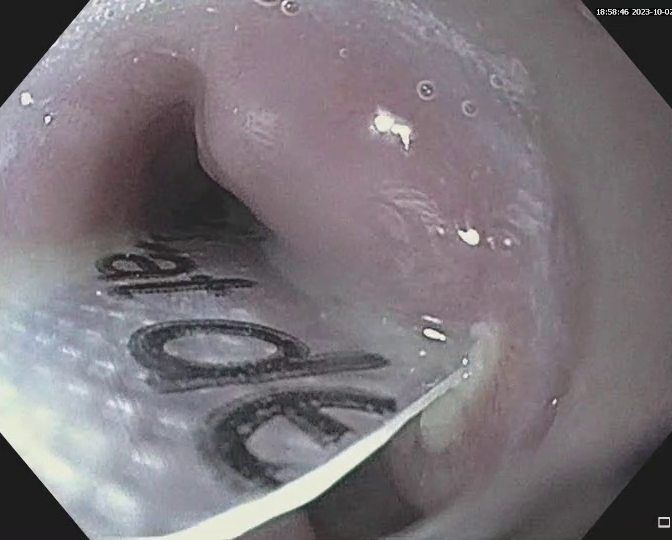
The pseudocyst was initially punctured transgastrically, under endoscopic ultrasound guidance, avoiding the intervening vessels, with a 19G needle through which a guide wire was placed (Figure 3). A 10 Fr cystotome was then inserted followed by placement of the second guide wire (Figure 4). Two plastic “pigtail” stents of 7 and 8.5 Fr were then placed, with effective drainage of the pseudocyst contents in the stomach (Figure 5).
Contrast-enhanced endoscopic ultrasound allowed the differentiation of the pancreatic corporeal cystic tumor from the pseudocyst, respectively the drainage of the pseudocyst under safe conditions, under direct endoscopic ultrasound guidance.
Pancreatic pseudocyst is one of the complications of acute pancreatitis, with endoscopic ultrasound drainage being a minimally invasive treatment of choice in symptomatic patients (1,2). The technical and clinical success rate is 95% and 90% respectively. Complications are significantly lower compared to surgery and consist of perforation, bleeding or recurrence in less than 5% of patients.
The particularity of the case is represented by the presence of an IPMN that triggered an episode of acute pancreatitis with the formation of a pancreatic pseudocyst, drained minimally invasively under endoscopic ultrasound guidance. The presence of an IPMN of approx. 3 cm, even in the absence of intramural nodules or thickened wall, requires surgical re-evaluation with a view to performing a distal pancreatectomy with curative intent.
1. Ng PY, Rasmussen DN, Vilmann P, Hassan H, Gheorman V, Burtea D, Surlin V, Săftoiu A. Endoscopic Ultrasound-guided Drainage of Pancreatic Pseudocysts: Medium-Term Assessment of Outcomes and Complications. Endosc Ultrasound 2013; 2: 199-203.
2. Săftoiu A, Vilmann A, Vilmann P. Endoscopic ultrasound-guided drainage of pancreatic pseudocysts. Endosc Ultrasound 2015; 4: 319-23.