See other cases
Mucosal bridging
A 46 year old female patient diagnosed with pancolonic ulcerative colitis (UC) in January 2021 when she presented with a moderately-severe flare of disease, controlled with systemic steroids and 5-ASA maintenance treatment, presented without any increase in stool frequency or rectal bleeding, for endoscopic evaluation being diagnosed with moderate iron deficiency anemia in the context of metrorrhagia for 2 weeks. Her fecal calprotectin was elevated at 3650mcg/gr and all her infectious fecal tests were negative.
She had recently undergone a magnetic resonance examination of the pelvis for her gynecological symptoms showing rectal wall thickening with mesorectal fat stranding and doubtful fistula tract in the medium rectum.
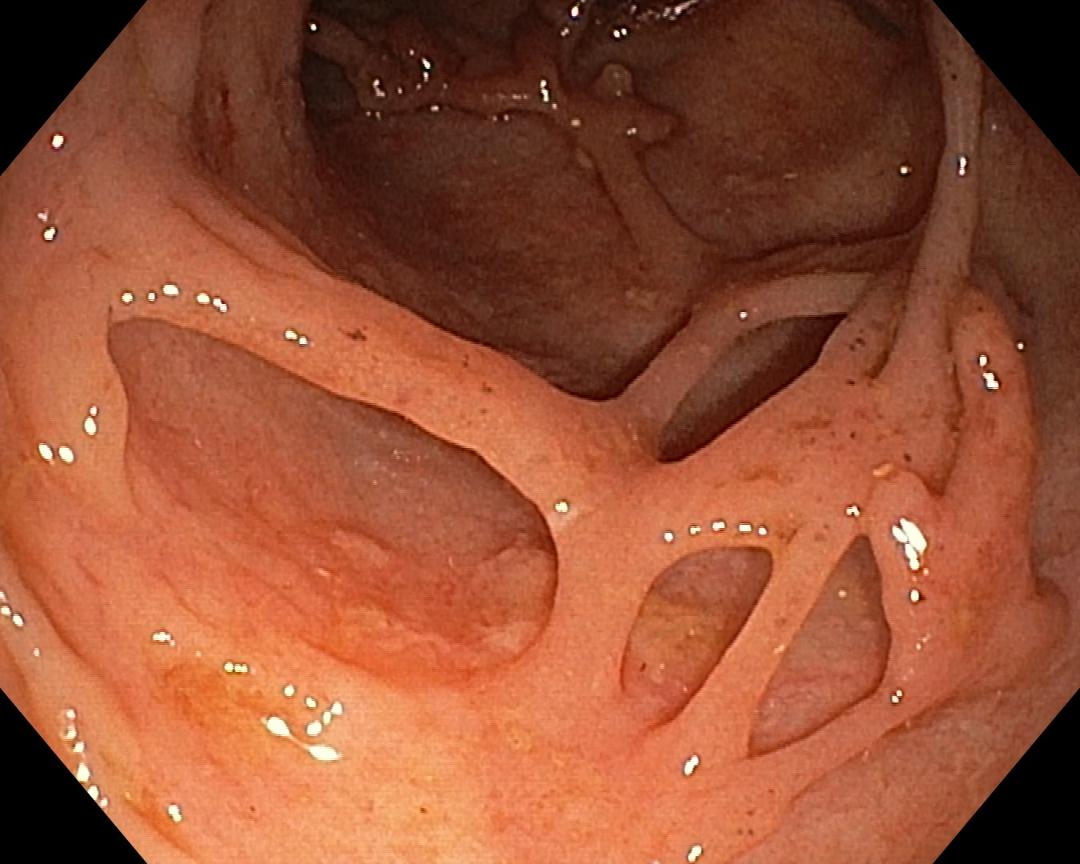
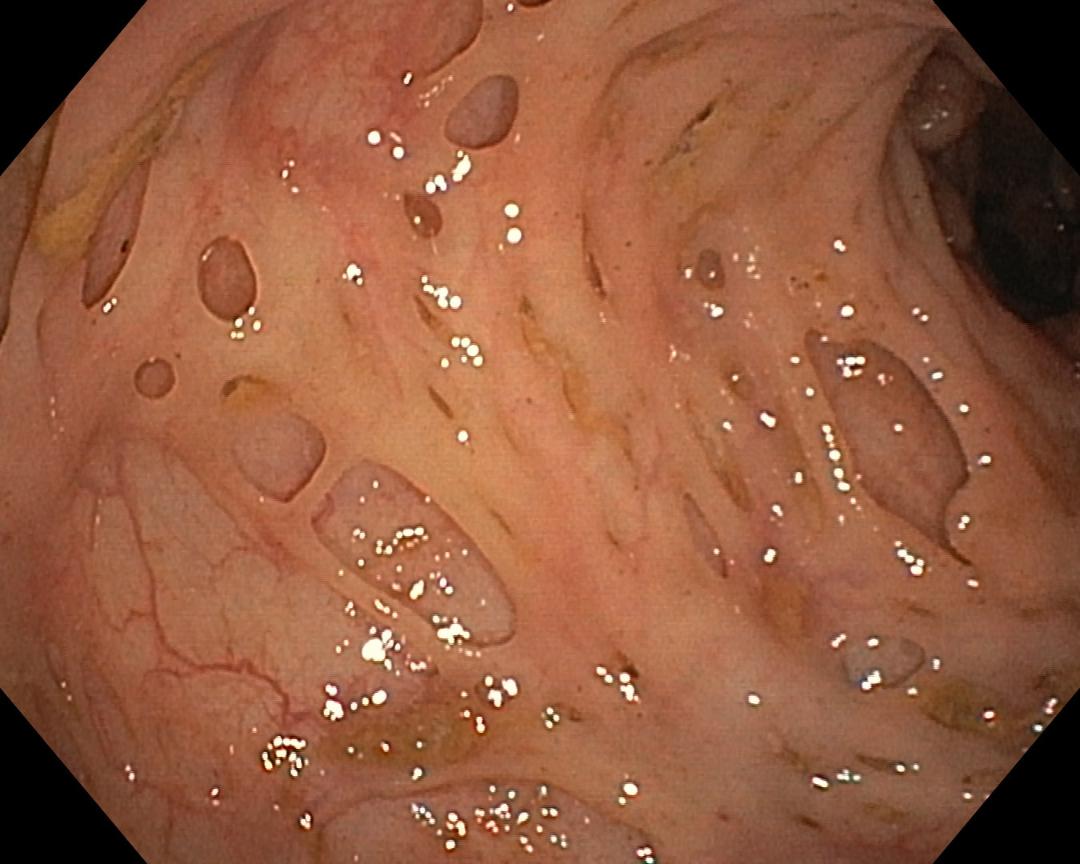
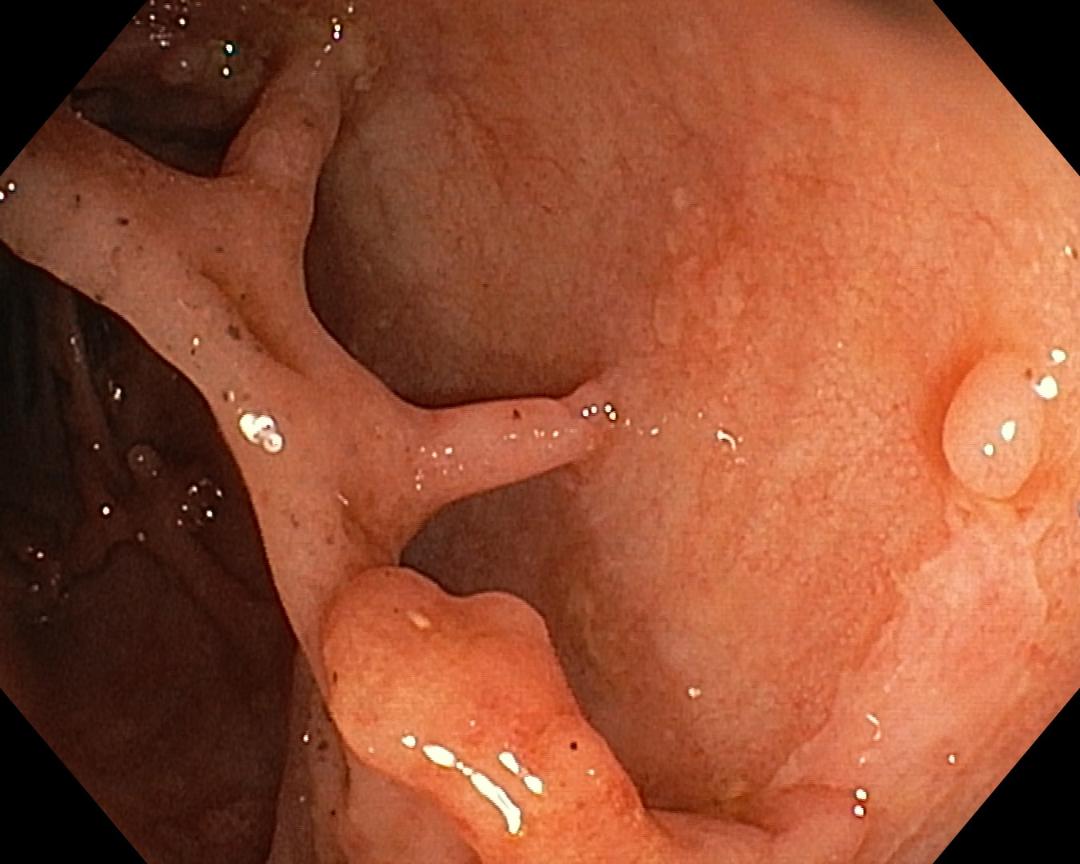
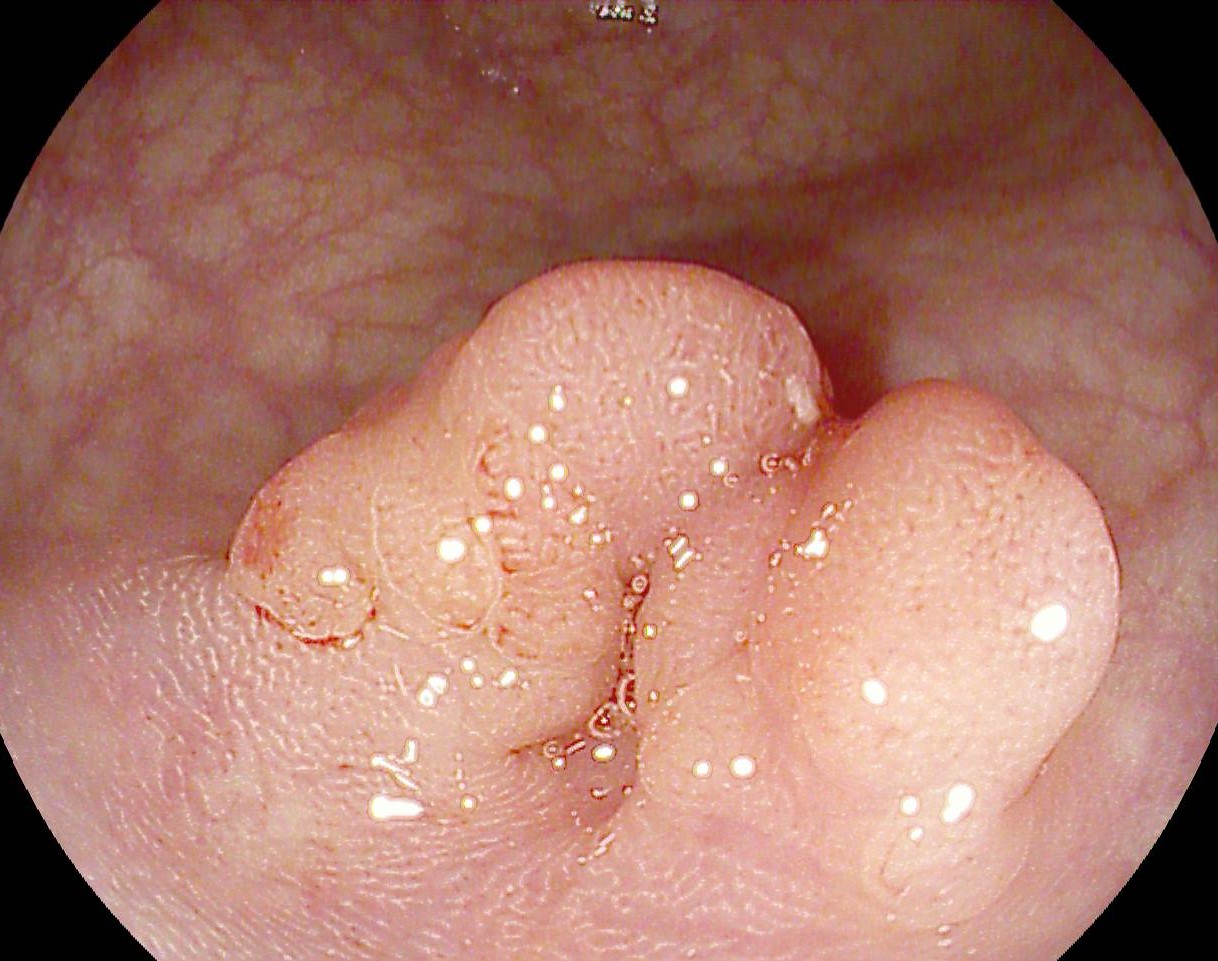
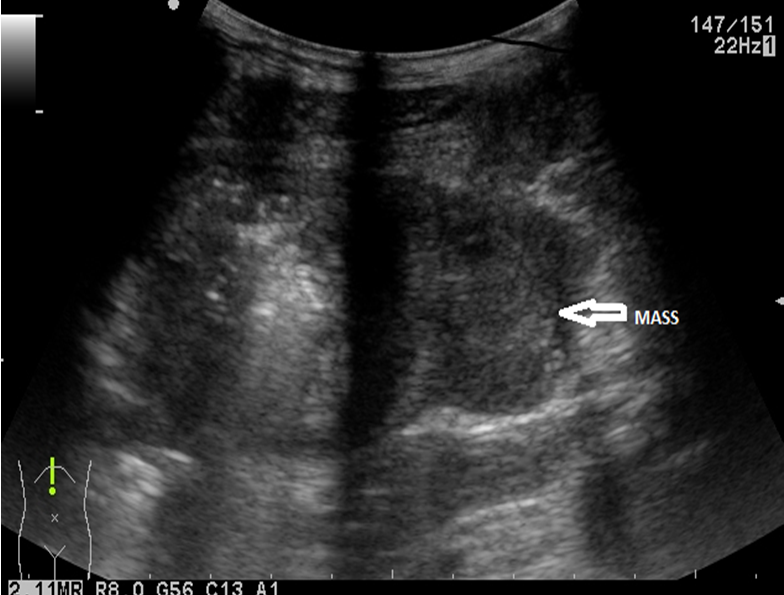
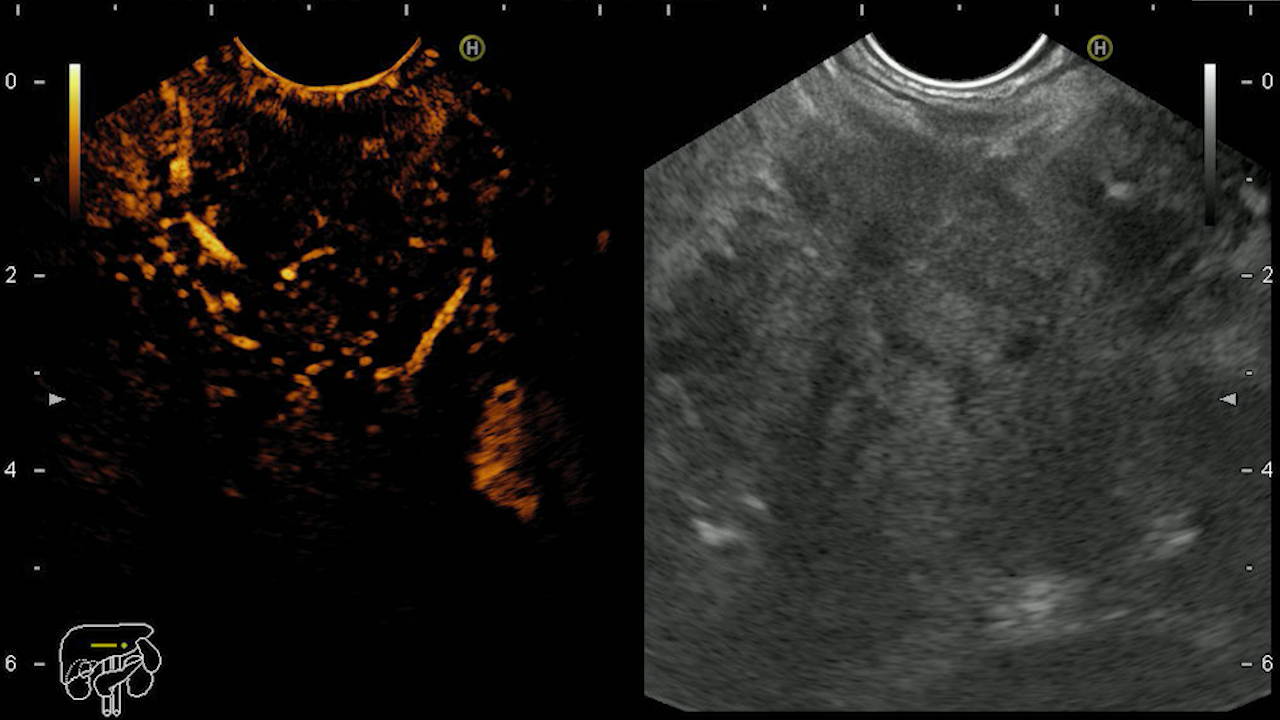
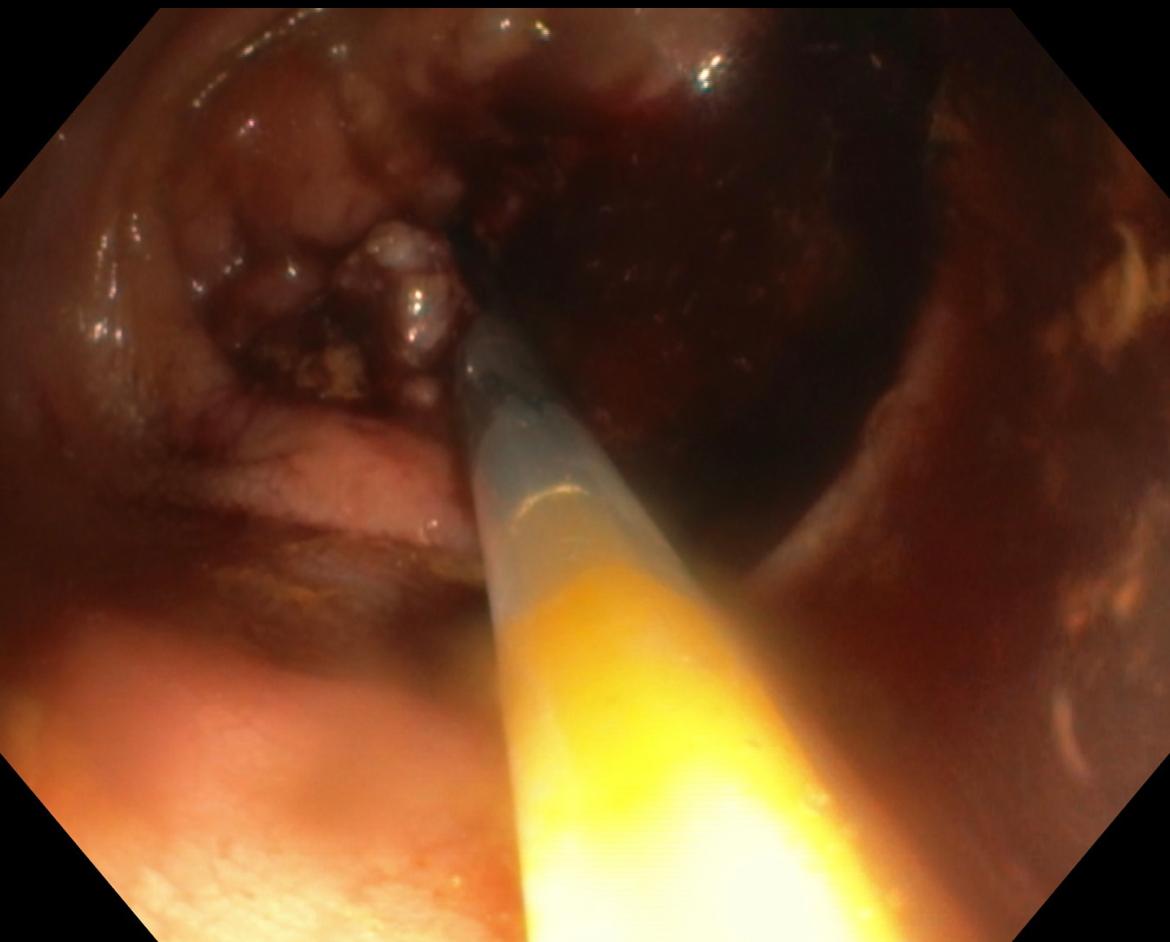
Multiple inflammatory polyps and mucosal bridges localized throughout the entire colon, with normal appearing underlying mucosa. Several erythematous areas without other endoscopic features of disease activity were identified in the sigmoid segment Fig. 1, Fig. 2, Fig. 3.
Pancolonic ulcerative colitis in endoscopic remission (Mayo 1, UCEIS 1).
Mucosal bridging (MB) in inflammatory bowel diseases has been described as early as 1980s, being associated with both ulcerative colitis and Crohn’s disease, but more frequently with UC.
These bridges represent regenerative consequences of severe ulcerative lesions, their pathogenesis being related to the healing process of the undermining mucosa on the site of previous profound ulcers, and the attachment sites for these bridges lay on previously non-ulcerated mucosa generating an endoscopic appearance of Swiss cheese/ dissection pockets1. Pathological examination of these bridges shows chronic inflammation but they carry no malignant potential2.
They can persist long after the resolution of the acute flare, but do not represent endoscopic activity of the disease, as they are not taken into consideration in the Mayo, UCEIS or other endoscopic severity scores of the disease.
MB can appear also in other severe inflammatory disease of the colon such as ischemic colitis or tuberculosis, or other digestive sites such as the esophagus, stomach, etc.1
The problem posed by this case is the false wall thickening and doubtful fistula tract on MR examination generated by this endoscopic aspect, along with the elevated fecal calprotectin in otherwise clinical remission setting that could have been generated by the inflammation in these mucosal bridges.
1. Butcher GP. Lower Gastrointestinal Bleeding: Gastroenterology: An Illustrated Colored Text. London, Churchill Livingstone, 2003; pp. 70–71.
2. Gupta G, Nijhawan S, Chander S, Mathur A, Nepalia S. Colonic mucosal bridging in ulcerative colitis. Indian J Gastroenterol 2012; 31: 39.