See other cases
MEN1 gastrinoma
A 43-year-old man with multiple stools/day (up to 20) and weight loss, with imaging studies within normal limits (upper and lower digestive endoscopy, CT scan and MRI, respectively!), with repeated treatments for irritable bowel syndrome in the last 2 years (Trimebutine, Rifaximin, MeteoSpasmyl, countless pre- and probiotics).
Upper abdominal pain, multiple stools/day (up to 20) and weight loss (> 20kg).
Biological investigations: high levels of chromogranin A (780 ng/mL – Jan 2020; 1140 ng/mL – Feb 2020; 1380 ng/mL – Mar 2020) and gastrin (1200 pg/L), respectively serotonin, elastase, 5HIIA normal.
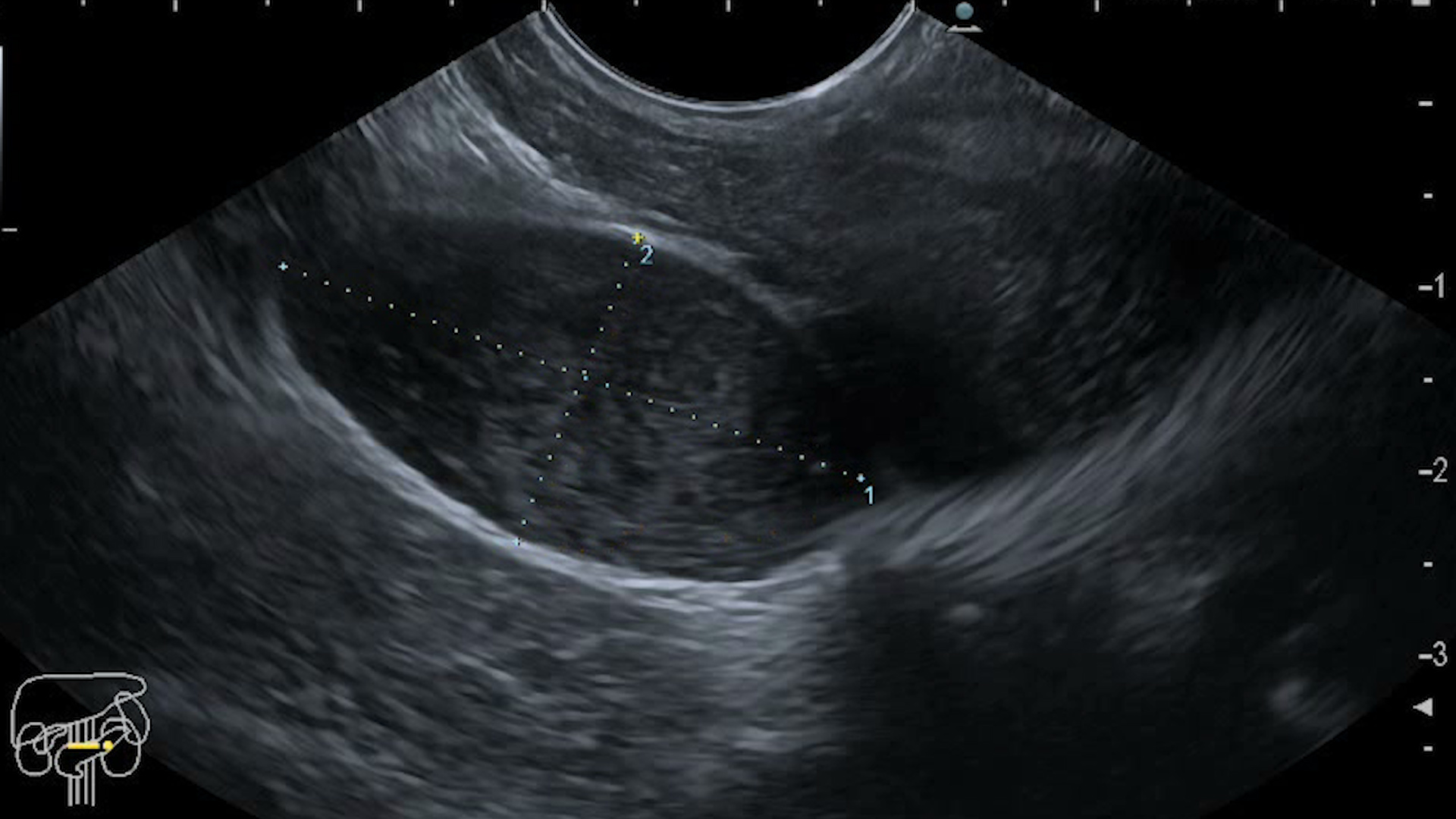
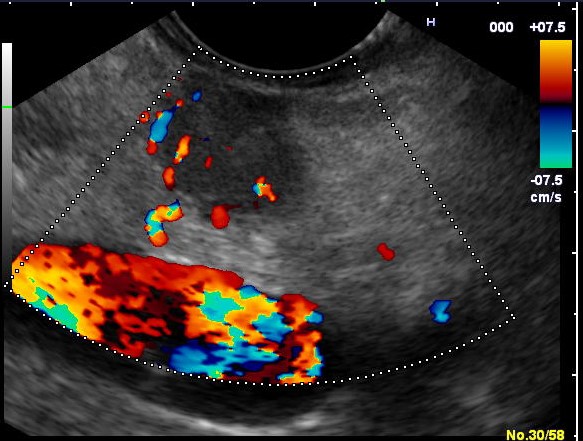
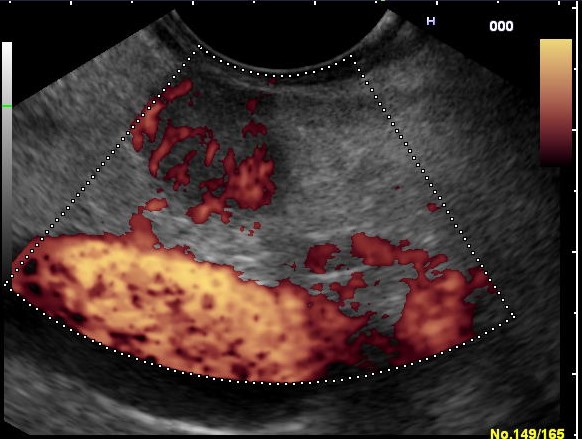
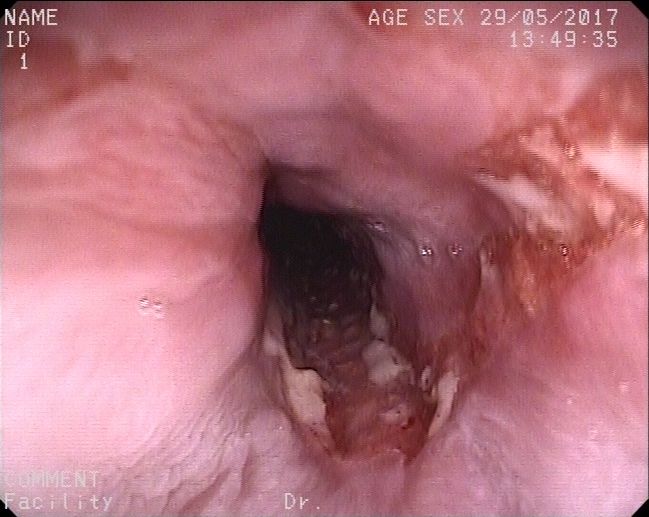
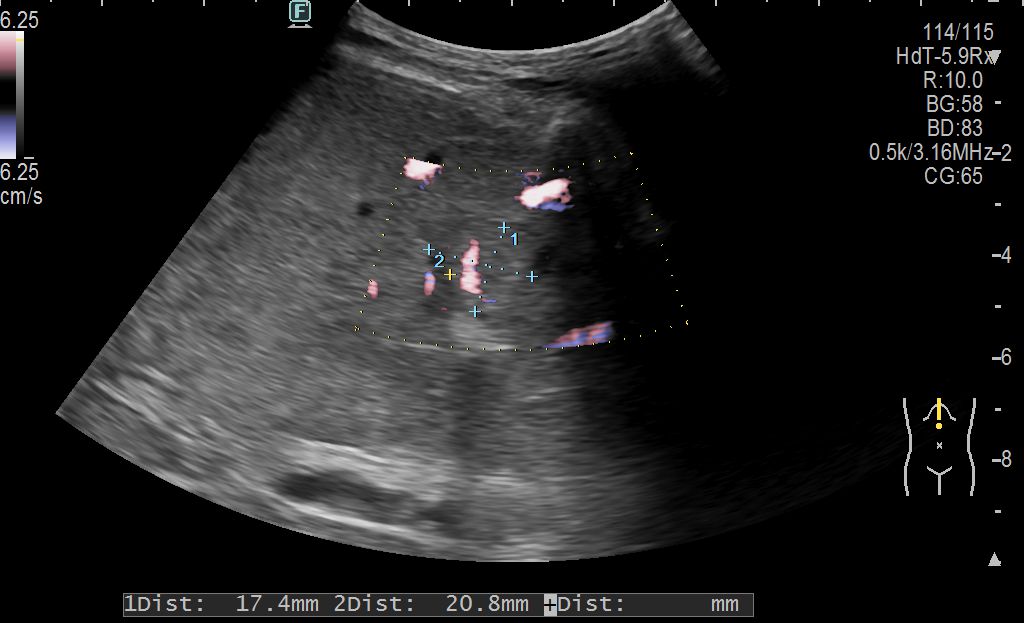
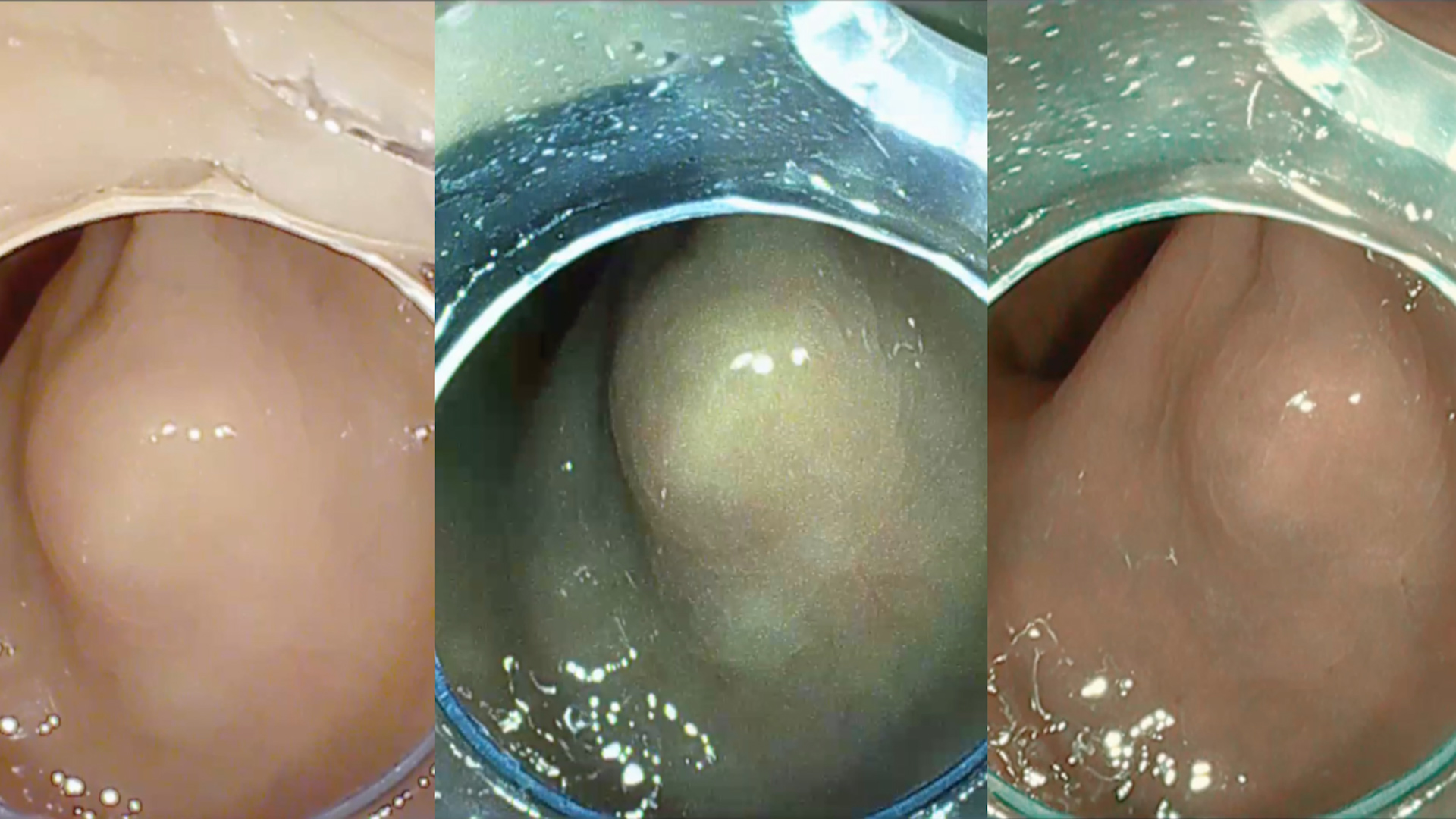
Endoscopic ultrasound indicated a dominant hypoechoic mass (well vascularized) at the pancreatic body, of approx. 20 mm diameter (Figure 1-2), from which a endoscopic ultrasound guided fine needle biopsy (EUS-FNB) was performed (Figure 3). Multiple other hypoechoic lesions (> 10) located in the head, body and tail of the pancreas, with variable sizes of 3-5-7 mm, were also visualised, from which a EUS-FNB was performed (Figure 4). SPECT-CT imaging with Tc99m Tektrotyd indicated positivity for the corporeal lesion.
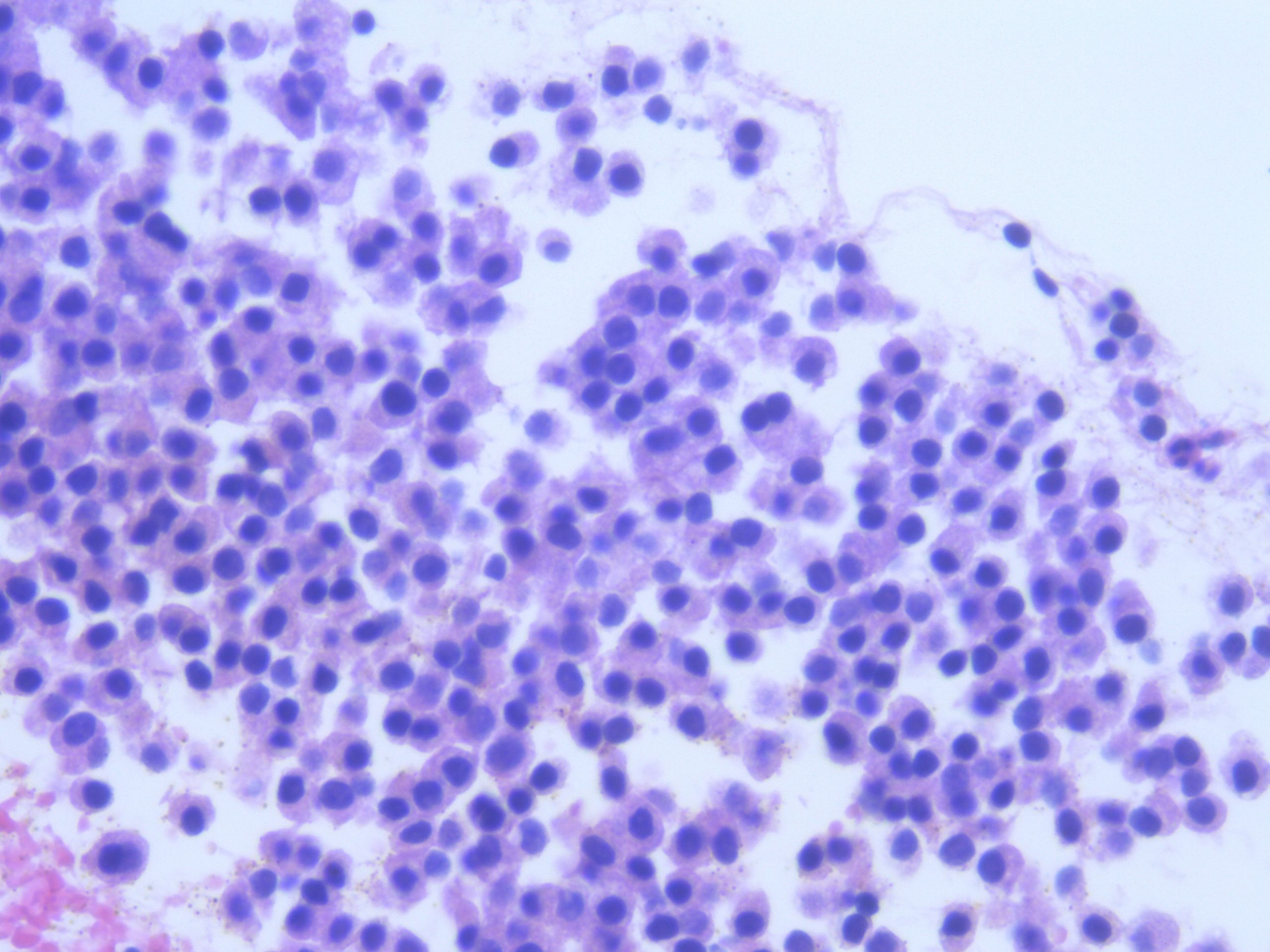
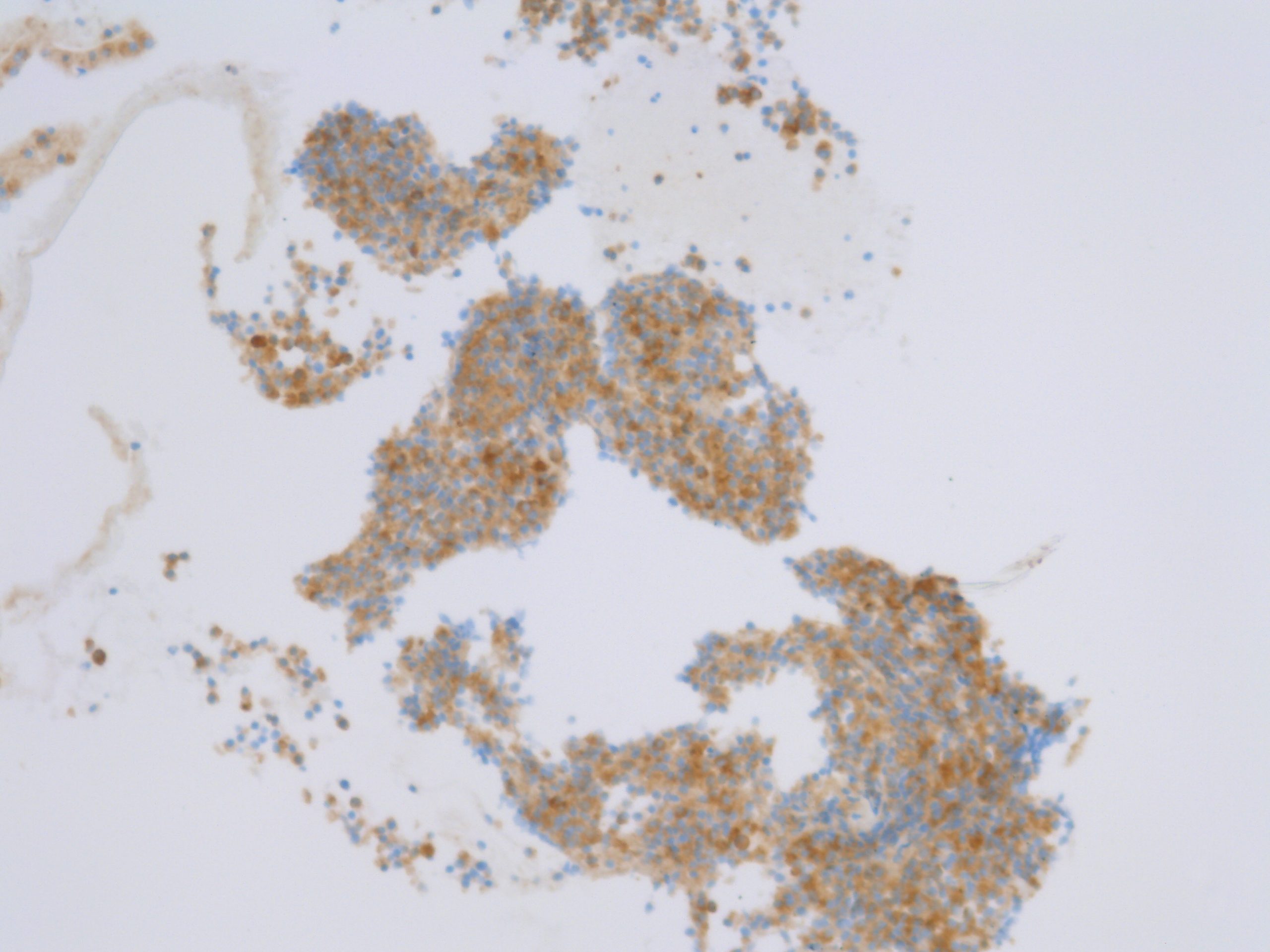
Fine needle aspiration biopsy with a “histological” fine needle was performed under endoscopic guidance (EUS-FNB) in the dominant corporeal mass and diminutive caudal lesions, confirming the diagnosis of well-differentiated neuroendocrine tumor (Pan-NEN G1). Cytological examination (on the slide) and microhistological examination (through paraffin processing of the cell block) was performed, with conventional hematoxylin-eosin staining (Figure 5) and respectively immunohistochemical, with positivity for CK AE1/AE3 (diffuse perinuclear), synaptophysin (diffuse) (Figure 6), chromogranin (focal) (Figure 7) and Ki67(2%). SMS receptors were also detected (SMS SSTR2 positivity > 66% of tumor cells).
The MEN1 gene was analyzed by PCR and bidirectional sequencing of the coding region + splicing for intron-exon junctions. MLPA was also applied to the identified deletions/duplications. The heterozygous deletion of 80 nucleotides from intron 6 to exon 7 of the MEN1 gene (c.928-33_963del) was identified – class 4 mutation (possibly pathogenic). The biological consequence is the loss of the splice site at intron 6, as well as 36 nucleotides at the 5′ end of exon 7, with an exon 7 missing from the final protein product. In conclusion, the patient is affected by MEN-1 as a consequence of the mentioned deletion, with a relatively good prognosis (1).
The patient is being treated with Pantoprazole (40 mg x 2/day), Sandostatin LAR (20 mg x 2/month) and Sutent (200 mg/day), being a candidate for PRRT (peptide receptor radionucleotide therapy) treatment with LUTATHERA (Lu 177 DOTATATE ) (2). Surgical treatment was delayed (3).
This case illustrates the role of endoscopic ultrasound for the evaluation of a rare pancreatic neuroendocrine tumor (SRS positive gastrinoma), with multiple secondary intrapancreatic tumors. Endoscopic ultrasound guided fine needle biopsy allowed a definite diagnosis to be established by histopathological examination with immunohistochemical staining.
1. van Beek DJ, Nell S, Pieterman CRC, et al . Prognostic factors and survival in MEN1 patients with gastrinomas: Results from the DutchMEN study group (DMSG). J Surg Oncol 2019; 120: 966-975.
2. Das S, Al-Toubah T, El-Haddad G, Strosberg J. 177Lu-DOTATATE for the treatment of gastroenteropancreatic neuroendocrine tumors. Expert Rev Gastroenterol Hepatol 2019; 13: 1023-1031.
3. Norton JA, Foster DS, Ito T, Jensen RT. Gastrinomas: Medical or Surgical Treatment. Endocrinol Metab Clin North Am 2018; 47: 577-601.
Scar Resection assisted by Band-Ligation for incomplete EMR