See other cases
A 56-year-old male patient, known with left renal cell carcinoma (pT3) with radical nephrectomy in 2005, diabetes type 2 and hypertension is referred for endoscopic ultrasound (EUS) evaluation with the suspicion of autoimmune pancreatitis raised in a previously performed magnetic resonance cholangiopancreatography (MRCP). The patient has been experiencing epigastric pain and steatorrhea for about 2 months.
Clinic: pallor.
Biologic: mild normochromic, normocytic anemia, hyperglycemia, hypercholesterolemia, CA 19.9 = 63.2 U/ml
MRCP: cephalic pancreatitis with subsequent body and tail atrophy suggestive of an autoimmune condition or pancreas divisum. The recommendation was to check the levels of IgG4 in the blood and in the biopsy specimen.
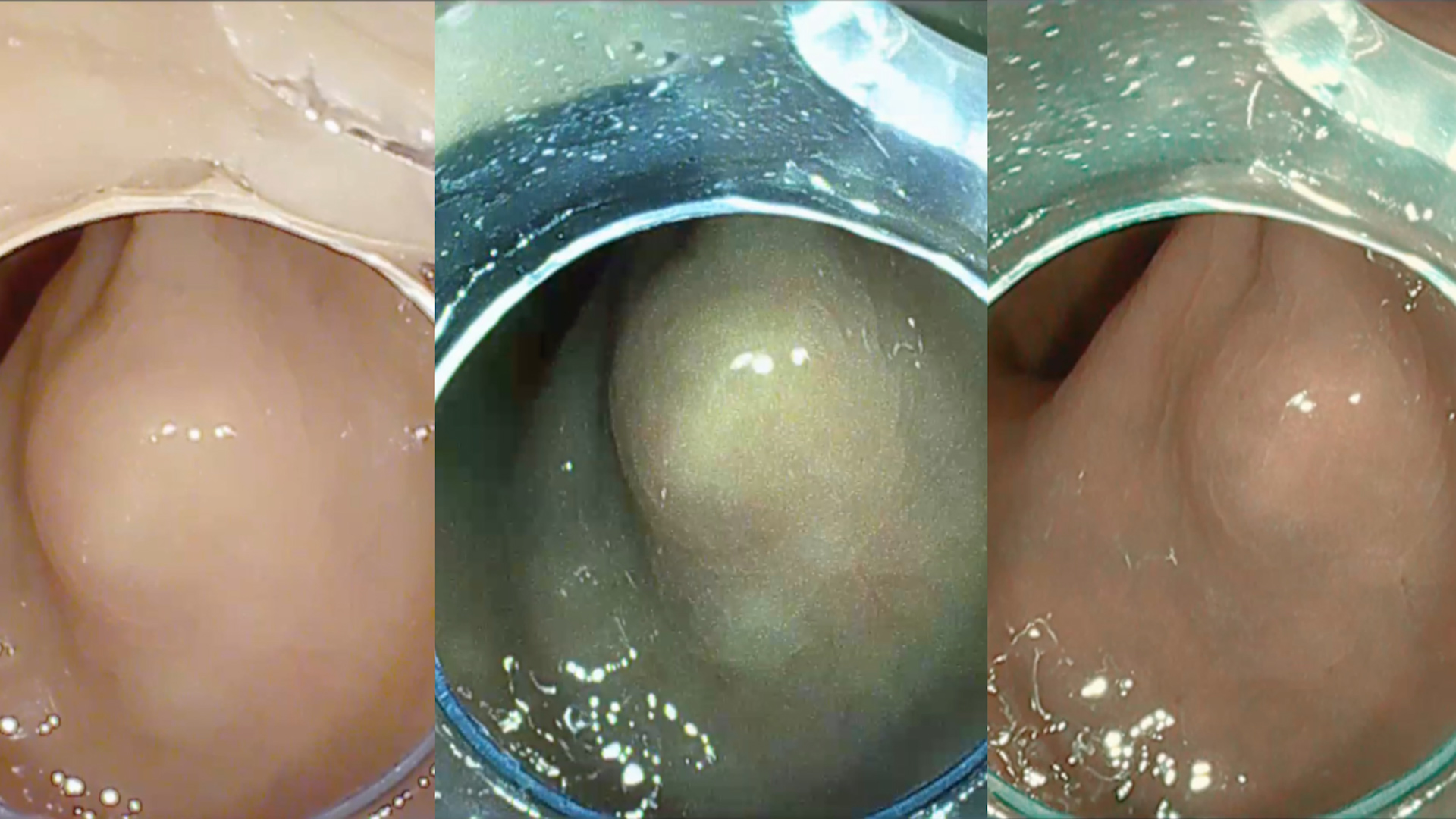
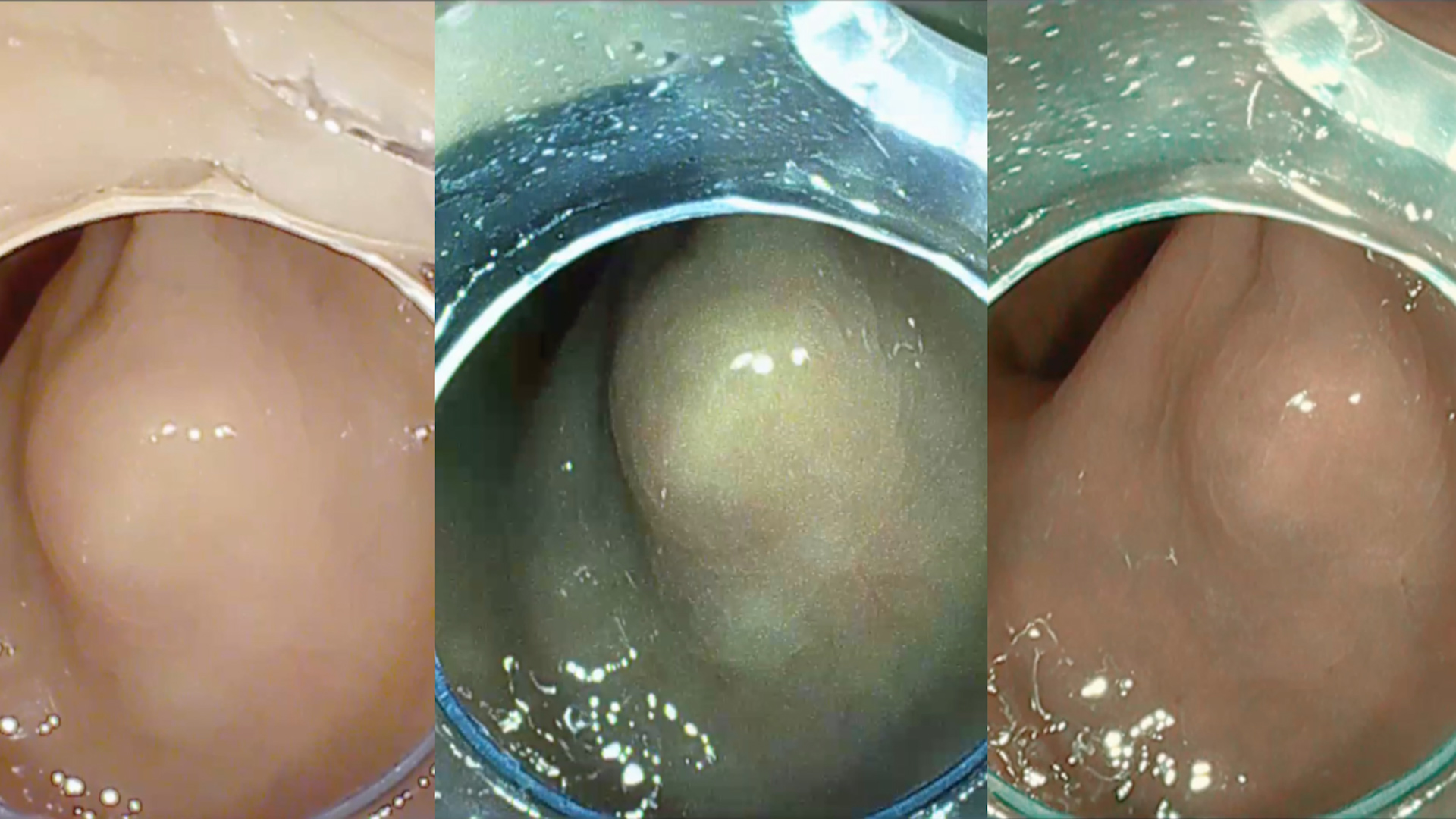
EUS-FNB: 2 pancreatic nodules (2 cm and 3 respectively) in the ampullary and cephalic region. EUS elastography revealed that the lesions were stiff and during contrast-enhanced EUS (CE-EUS) they became hyper-enhanced in the arterial phase with wash-out in the venous phase. Endoscopic biopsies have been taken from the papillary tumor. Fine needle biopsies (FNB) were obtained from cephalic pancreatic nodule. Histopathological examination and immunohistochemistry (IHC) analysis: pancreatic nodules proved to be metastases from renal carcinoma.
ERCP 1: the patient presented at the emergency room (5 days after EUS) for fever, jaundice, right upper quadrant pain. An emergency ERCP was indicated. Due to difficult biliary cannulation (malignant appearance of the papilla) a needle-knife fistulotomy was performed. After biliary cannulation using guidewire-assisted technique, two plastic stents (9 and 7 cm 10 Fr, respectively) were inserted with efficient biliary drainage at the end of the procedure.
ERCP 2: one day after ERCP the patient presented hematemesis, melena, with sudden drop of hemoglobin. Through ERCP, diffuse bleeding of the ampullary tumor was identified. The hemostasis was obtained by inserting a biliary fully covered self-expandable metal stent.
Upper gastrointestinal bleeding from the ampullary tumor. Acute cholangitis. Pancreatic and ampullary metastasis from renal carcinoma.
Regarding solid pancreatic masses, EUS-FNB combined with EUS elastography and CE-EUS proved high accuracy in establishing a precise diagnosis. Furthermore, other imaging techniques such as MRCP or computer-tomography (CT) proved to have a complementary role in establishing a precise diagnosis.
Last but not least, European Society of Gastrointestinal Endoscopy (ESGE) has recommended temporary placement of a biliary metal stent for post-sphincterotomy bleeding in cases where standard hemostasis techniques were not effective.
EUS-FNB combined with elastography-EUS and CE-EUS proved high accuracy in establishing a precise diagnosis, in the management of rare solid pancreatic masses. In the management of post-sphincterotomy bleeding refractory to standard hemostatic modalities the placement of a biliary fully covered self-expandable metal stent was recommended.
See other cases