See other cases
Hilar cholangiocarcinoma – endoscopic prosthesis by ERCP
A 62-year-old patient, underwent surgery in 2016 for colon cancer (moderately differentiated adenocarcinoma), with a CT scan performed in 2020 that highlighted secondary peritoneal determinations, presents for yellow pigmentation of the skin with the onset of a few weeks.
Moderate general condition, intensely icteric skin, painless distended abdomen.
AST – 488 U/l, ALT – 302 U/l, total bilirubin – 37,40 mg/dl, conjugated bilirubin – 29,73 mg/dl.
Cholangio-MRI showed significant bilateral intrahepatic bile ducts dilatations and the presence of an intraluminal tumor formation located at the level of the biliary crossroads that extended to the level of the left hepatic duct, with an appearance suggestive of hilar Bismuth IIIB cholangiocarcinoma (Klatskin tumor). Perihepatic, perisplenic, and inter-bowel ascites associated with peritoneal nodules and thickening up to 38/24 mm in the context of peritoneal carcinomatosis has also been visualized.
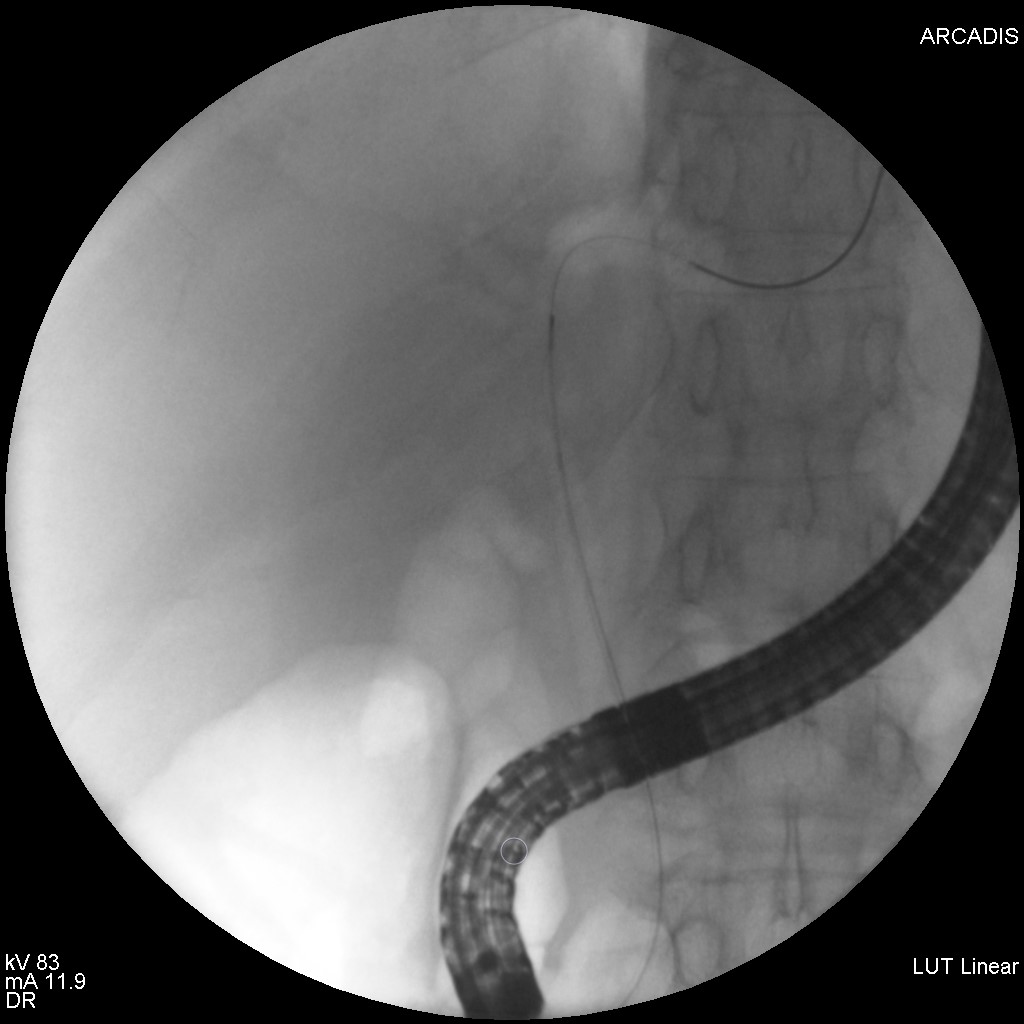
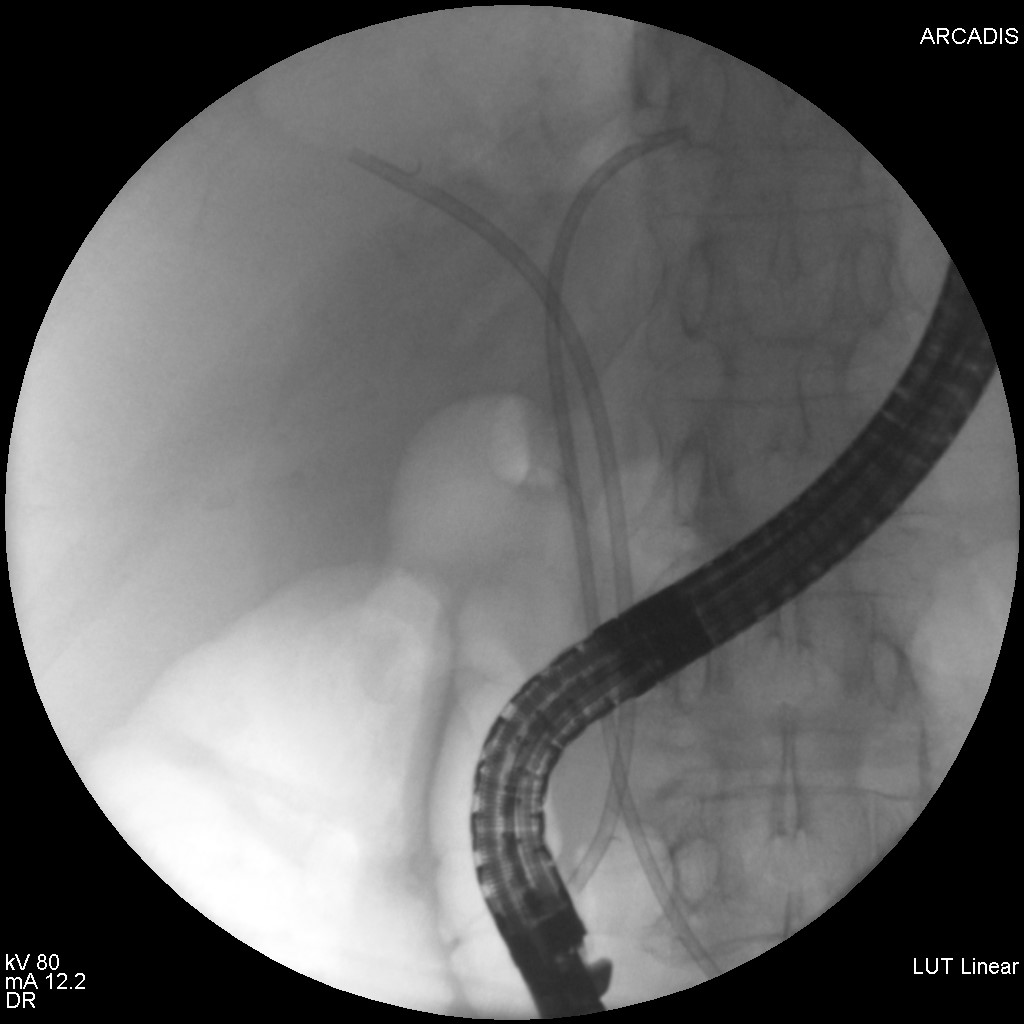
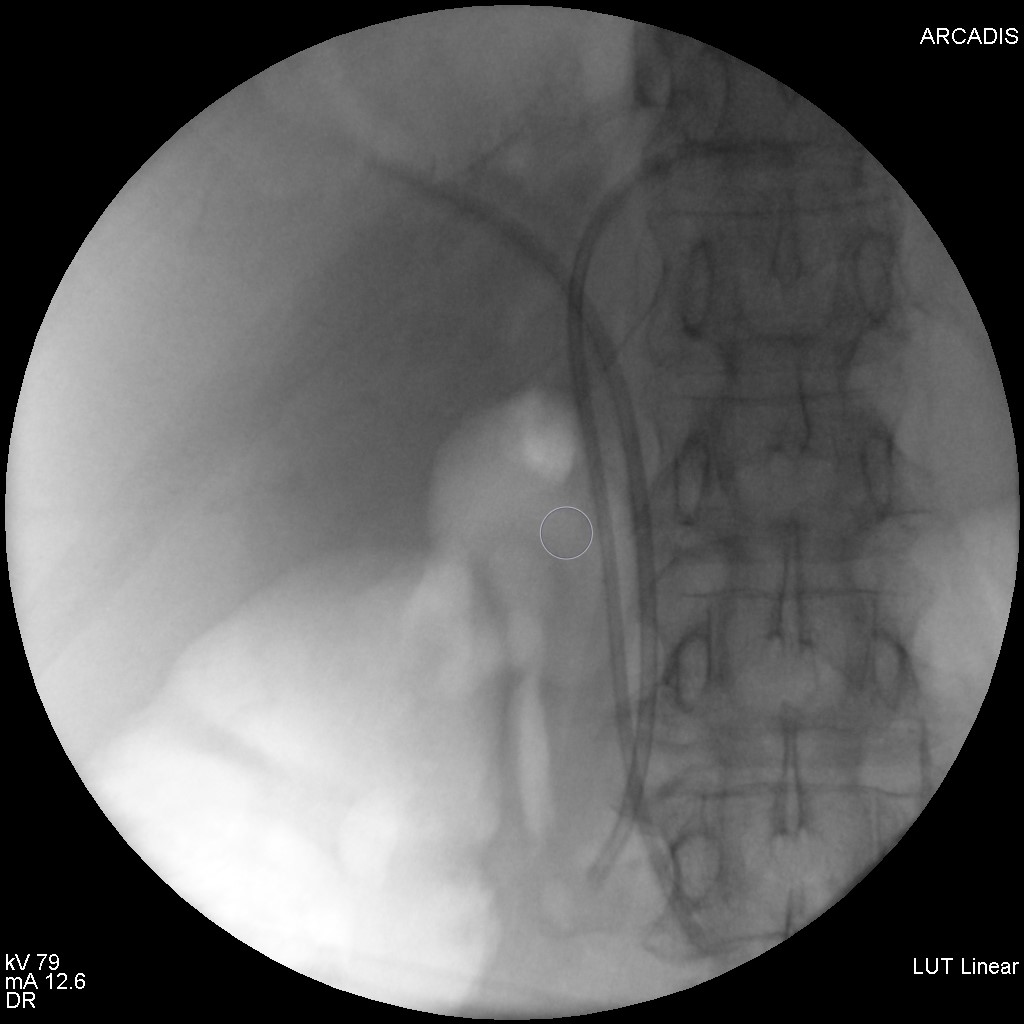
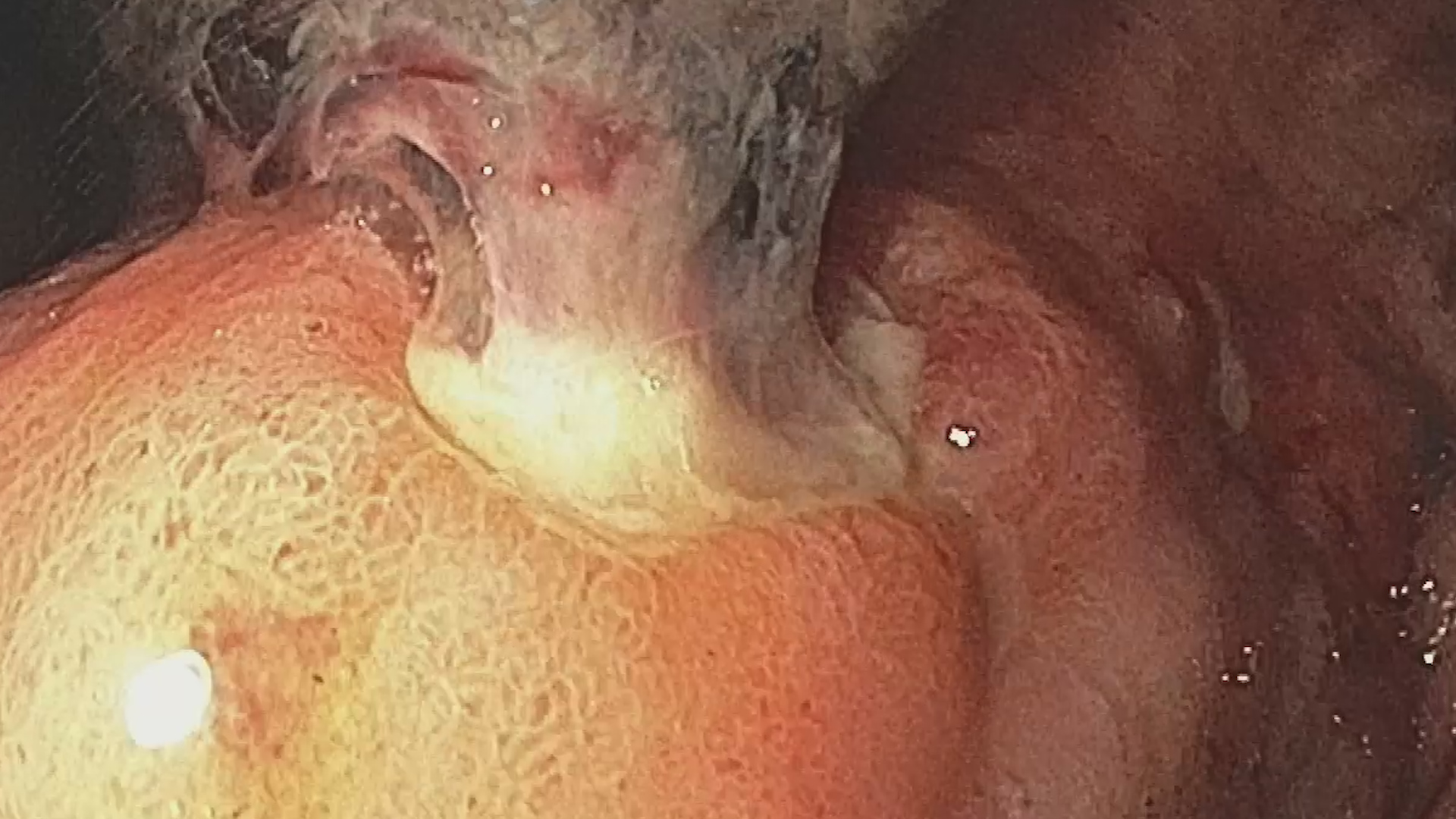
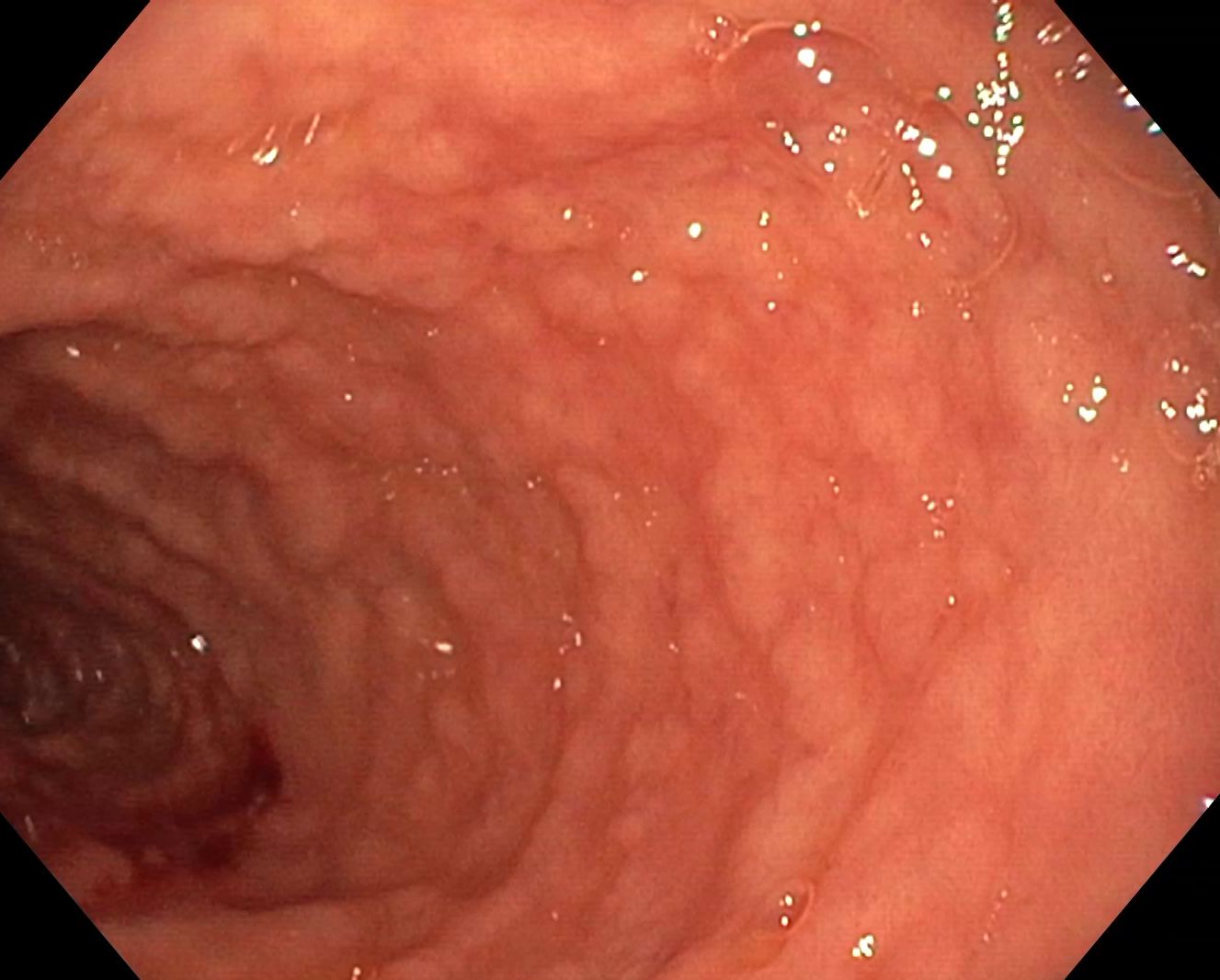
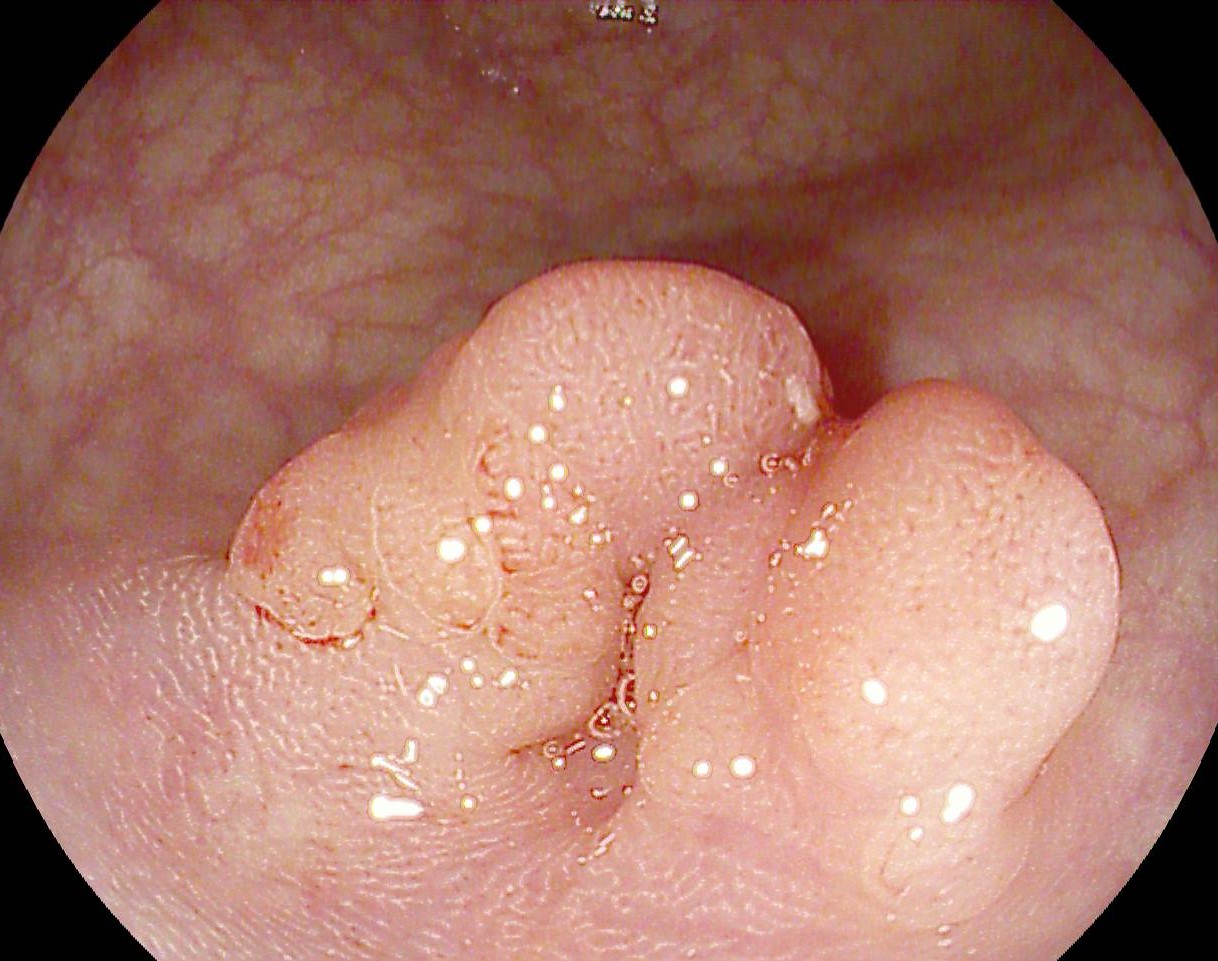
ERCP was performed – the main bile duct was cannulated and an air cholangiogram (Fig. 1) was initially performed, which revealed a centrohilar stenosis with marked dilatation of the left hepatic duct and bilateral intrahepatic bile ducts. A minimal amount of radiopaque contrast material was subsequently injected. Irregular, tight stenosis was revealed, located at the level of the biliary carrefour at a distance of approximately 20 mm, extended to the left hepatic duct, dilated upstream (Fig.2). Retrograde sphincterotomy was performed and the left intrahepatic bile duct was deeply selectively cannulated, placing a 7.5 Fr/15 cm plastic stent (Fig. 3). Next, a branch of the right intrahepatic bile duct was cannulated and an 8 Fr/12 cm plastic stent was also placed (Fig. 4).
The subsequent evolution was favorable, with total bilirubin decreasing to 20 mg/dl within a few days post-procedure.
Six weeks later, the patient returned for chills and pain in the right hypochondrium of 3 days’ onset. Biological at that time – total bilirubin – 8 mg/dl, conjugated bilirubin – 6.28 mg/dl.
ERCP was performed – endoscopically, both biliary stents were found to be occluded. The stent placed in the left intrahepatic bile duct was extracted with alligator forceps, the left intrahepatic bile duct was selectively deeply cannulated, and a 10 Fr/14 cm plastic stent was placed. The other stent was subsequently retrieved and the right intrahepatic bile ducts were deeply cannulated with placement of a 10 Fr/12 cm plastic stent. At the end of the procedure, effective drainage of stasis bile was observed on both stents.
The evolution was favorable, with remission of symptoms and halving of bilirubin values at 48h.
Bismuth III B hilar cholangiocarcinoma. Peritoneal secondary determinations. History of colon cancer.
Hilar cholangiocarcinomas affect a complex anatomic region, so stenting is difficult and carries a significant risk of developing angiocolitis if drainage of contrast material injected for cholangiogram is unsuccessful. Thus, although ductal changes are usually less obvious, air entrainment can be used to perform the cholangiogram in order to avoid contrast injection. In this context, pre-procedural assessment by cholangio-MRI is mandatory for prosthetic planning.
Stent placement is guided by the intraductal extent of the lesion and is based on the Bismuth-Corlette classification. In bismuth type I cholangiocarcinomas, a single stent placement is usually sufficient, while in bismuth type II-IV multiple stents are required.
There are two techniques for prosthetics of the left and right hepatic ducts. The first technique involves the initial placement of one guide wire in each hepatic duct and the subsequent placing of stents on each of them. The second technique, the one used in the present case, consists of deep cannulation and initial stenting of the left hepatic duct which is technically easier, followed by cannulation and insertion of a second stent in the right hepatic duct.
Two types of prostheses can be used – expandable uncovered plastic or metal stents. The patency of plastic stents is up to 3 months, so they must be changed at this interval because of the risk of clogging and cholangitis. They are used both for palliative purposes and for decompression of the bile ducts until curative surgical intervention. Expandable metal stents are used in patients with a longer life expectancy, but for palliative purposes. Uncovered stents are used, due to the risk of obstruction of the bile ducts associated with the installation of covered metal prostheses.
Endoscopic ERCP prosthesis of malignant centrohilar stenoses is technically difficult. This can be associated with the occurrence of angiocolitis and subsequently liver abscesses, if the contrast substance injected for performing the cholangiogram is not subsequently drained. Stent placement is guided by the Bismuth-Corlette classification and usually involves the insertion of a single stent in Bismuth I lesions and multiple stents in Bismuth II-IV lesions.
- Bilal M, Freeman ML. Endoscopic Retrograde CholangiopancreatographyStenting for Hilar Cholangiocarcinoma. TechniquesandInnovations in Gastrointestinal Endoscopy. 2022; 24(2):190-199
- Uppal DS, Wang AY. Advances in endoscopic retrograde cholangiopancreatography for the treatment of cholangiocarcinoma. World J GastrointestEndosc. 2015 Jun 25;7(7):675-87
- Dumonceau JM, Tringali A, Papanikolaou IS. et al. Endoscopic biliary stenting: Indications, choice of stents, and results: European Society of Gastrointestinal Endoscopy (ESGE) Clinical Guideline – Updated October 2017. Endoscopy 2018;50:(910-930)