See other cases
Giant pancreatic pseudocyst drainage
A 51-year-old woman, which in 2022 presented an episode of acute pancreatitis complicated by an asymptomatic giant pseudocyst that was monitored by imaging is hospitalized for fever and abdominal pain that started a few days prior.
Clincal: altered general condition, stable, fever 37.3 C, painful abdomen particularly in the left part, without signs of peritoneal irritation.
Biological: inflammatory syndrome: CRP 211 mg/l; fibrinogen 708 mg/dl without leucocitosis.
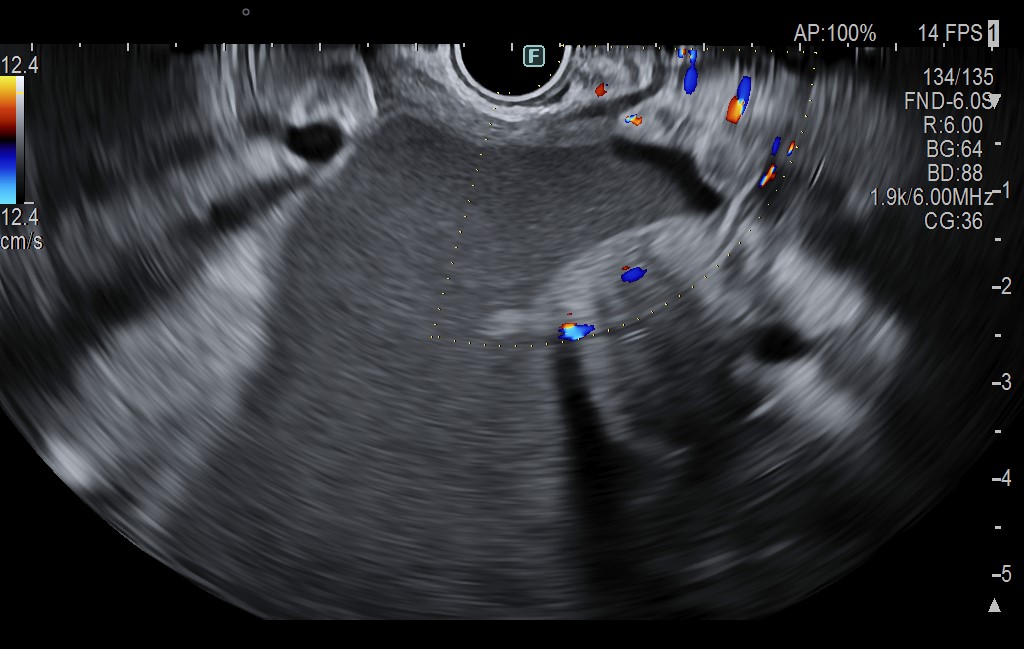
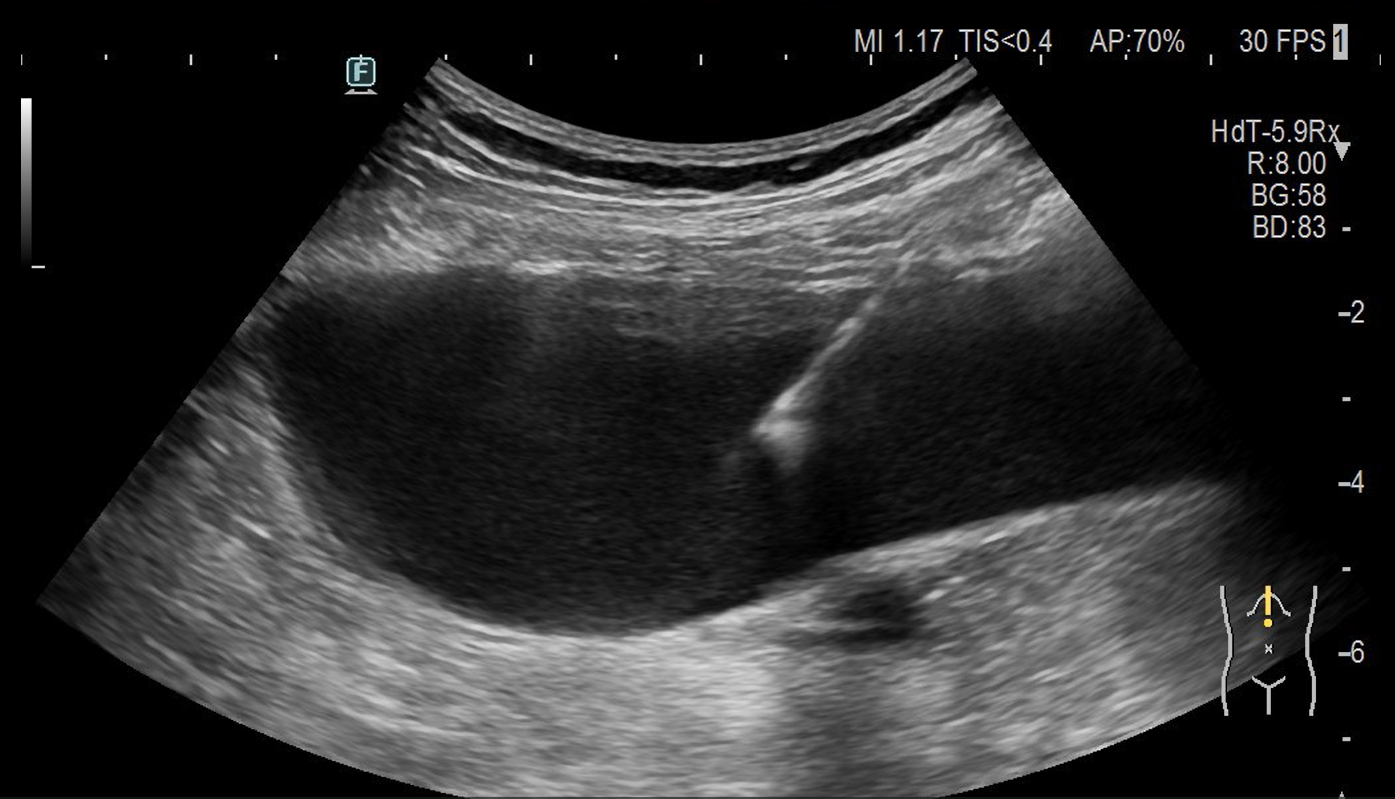
Ultrasound revealed a massive transonic mass starting from pancreas and extending to the left iliac crest, in contact with the left kidney, which presents hydronephrosis due to external compression.
The contrast enhanced CT scan confirmed the ultrasound diagnostic. This imaging technique showed that the pseudocyst had an anatomical contact with the posterior gastric wall and with the left lumbar abdominal wall.
Drainage
The procedure was performed in the OR with deep sedation under the surveillance of the anesthesiology team.
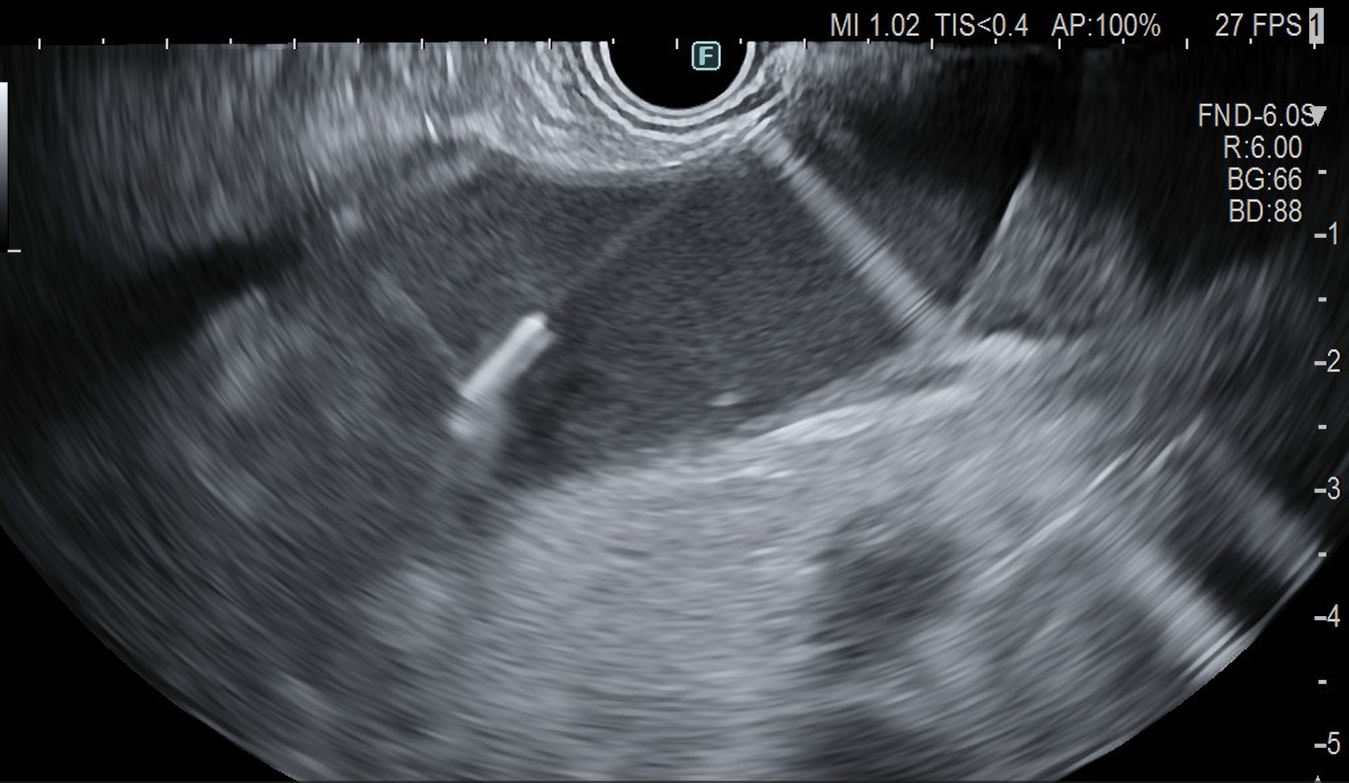
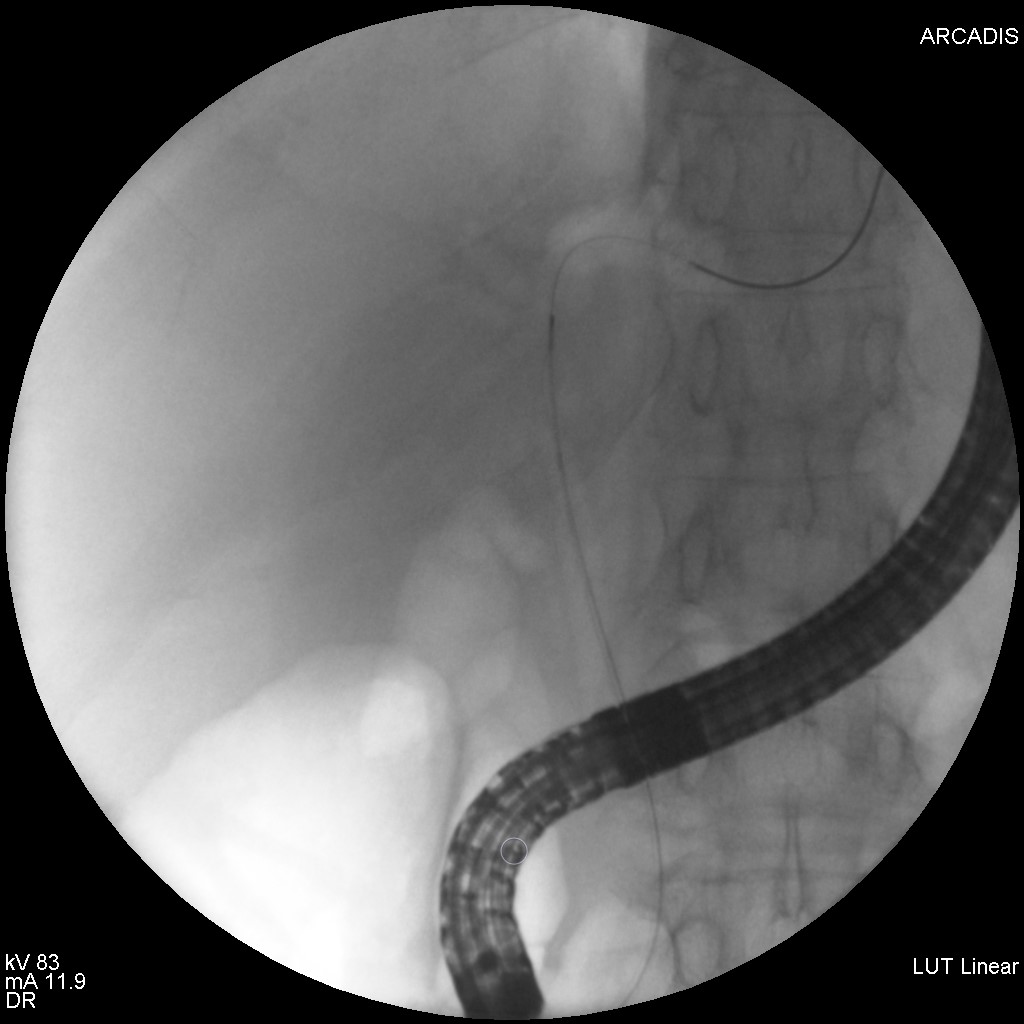
In the firs stage, the endoscopic ultrasound drainage was performed. A 19G FNB needle was used to puncture the pseudocyst through the posterior gastric wall, and after that, a 0.035 Jagwire guidewire was inserted into the pseudocystic cavity. The needle was removed and using the guidewire a cystotome was used to create the fistulous tract. A double pigtail 7 Fr stent was positioned with efficient drainage of the pseudocyst.
In the second part of the procedure, under ultrasound guidance, the pseudocyst was punctured transcutaneously at the level of the contact area with the abdominal wall in the left lumbar region and a guidewire was placed into the cavity. The puncture channel was progressively dilated with tissue dilators and then a 10 Fr monopigtail stent was placed into the caviy with efficient drainage.
The drained liquid had a brown color. Through the percutaneous drainage stent 500 ml of liquid was evacuated. A sample was sent to the laboratory for bacterial and fungal analysis.
Evolution
The procedure had no immediate or late complications. After drainage, the patient’s condition quickly improved without any subsequent pain or fever. Two days after the procedure, the inflammatory syndrome had regressed. A control CT scan was conducted prior to discharge. With the two stents in place and no signs of complications, it demonstrated significant regression of the pseudocyst. Three days after the drainage, the patient was discharged. The percutaneous drain was removed one week later.
Giant pancreatic pseudocyst.
Acute pancreatitis can lead to many complications. The pseudocyst is a frequent complication represented by a liquid collection that is well separated from the surrounding structures by a fibrotic wall. They occur up to four weeks after an episode of acute pancreatitis. In evolution, a small pseudocyst can disappear all by itself in a process of resorption, can stay at the same dimensions or it can enlarge.
In the past, the management of a pseudocyst was essentially surgergy, associated with high morbidity and mortality. Nowadays, with the rise of new endoscopic therapeutic techniques, we can approach this pathology in a new manner.
The endoscopic drainage of a pseudocyst is a procedure with low percentage of complications and a high grade of success. The endoscopic technique evolved quickly, and it became a standard procedure in guidelines. It consists of creating a connection between the pseudocyst and the stomach lumen to drain the liquid content into the gastric cavity.
Minimally invasive pseudocyst drainage is a very good alternative to surgical drainage with a low complication rate and excellent results regarding the drainage efficiency and the short hospitalisation.
- Yamada, T., Alpers, D. H., Kalloo, A. N., Kaplowitz, N., Owyang, C., & Powell, D. W. (2009). Textbook of Gastroenterology, Fifth Edition. Blackwell Publishing Ltd. https://doi.org/10.1002/9781444303254
- S. Habashi and P. V Draganov, “Pancreatic pseudocyst,” World J Gastroenterol, vol. 15, no. 1, p. 38, 2009, doi: 10.3748/wjg.15.38.
- Oh, C. H., Lee, J. K., Song, T. J., Park, J.-S., Lee, J. M., Son, J. H., Jang, D. K., Choi, M., Byeon, J.-S., Lee, I. S., Lee, S. T., Choi, H. S., Kim, H. G., Chun, H. J., Park, C. G., & Cho, J. Y. (2021). Clinical Practice Guidelines for the Endoscopic Management of Peripancreatic Fluid Collections. Clinical Endoscopy, 54(4), 505–521. https://doi.org/10.5946/ce.2021.185