See other cases
Gastric ESD
We present the case of a 70-year-old male patient with cardiovascular comorbidities: hypertension, chronic heart failure class III NYHA, mild biliary pancreatitis in the past, type II diabetes on oral antidiabetic medication, hepatic hemangiomas, and chronic kidney disease undergoing staging. The patient was evaluated endoscopically, revealing a nodular gastritis with an elevated lesion located in the antrum on the greater curvature, from which biopsies were taken. The histopathological result was compatible with complete intestinal metaplasia with mild epithelial dysplasia, Helicobacter Pylori negative.
Clinical: intermittent abdominal pain localized in the epigastrium.
Biologically: nitrogen retention with eGFR mL/min/1.73 m2, hyperglycemia, hyperuricemia, no anemia, negative tumor markers.
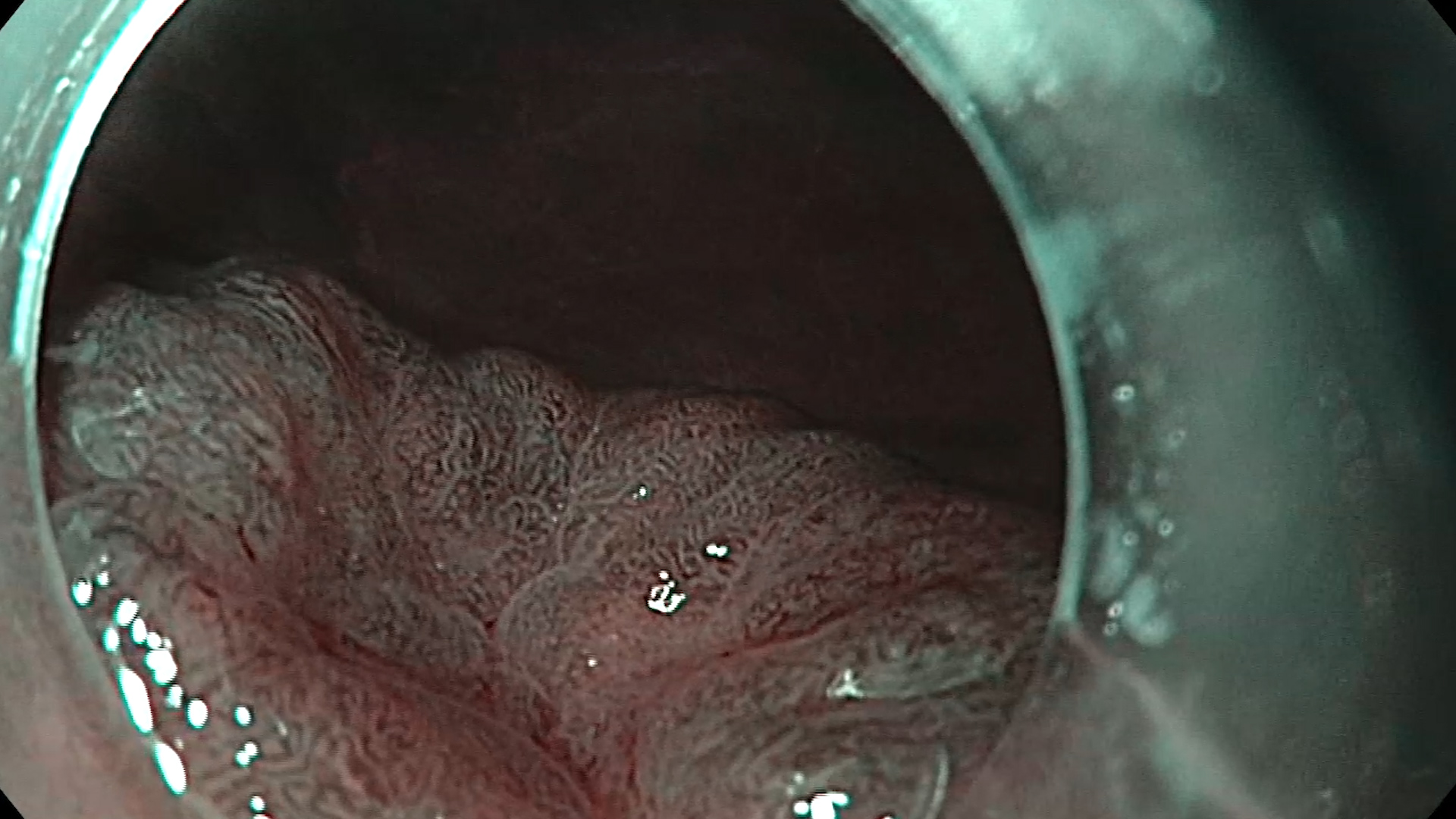
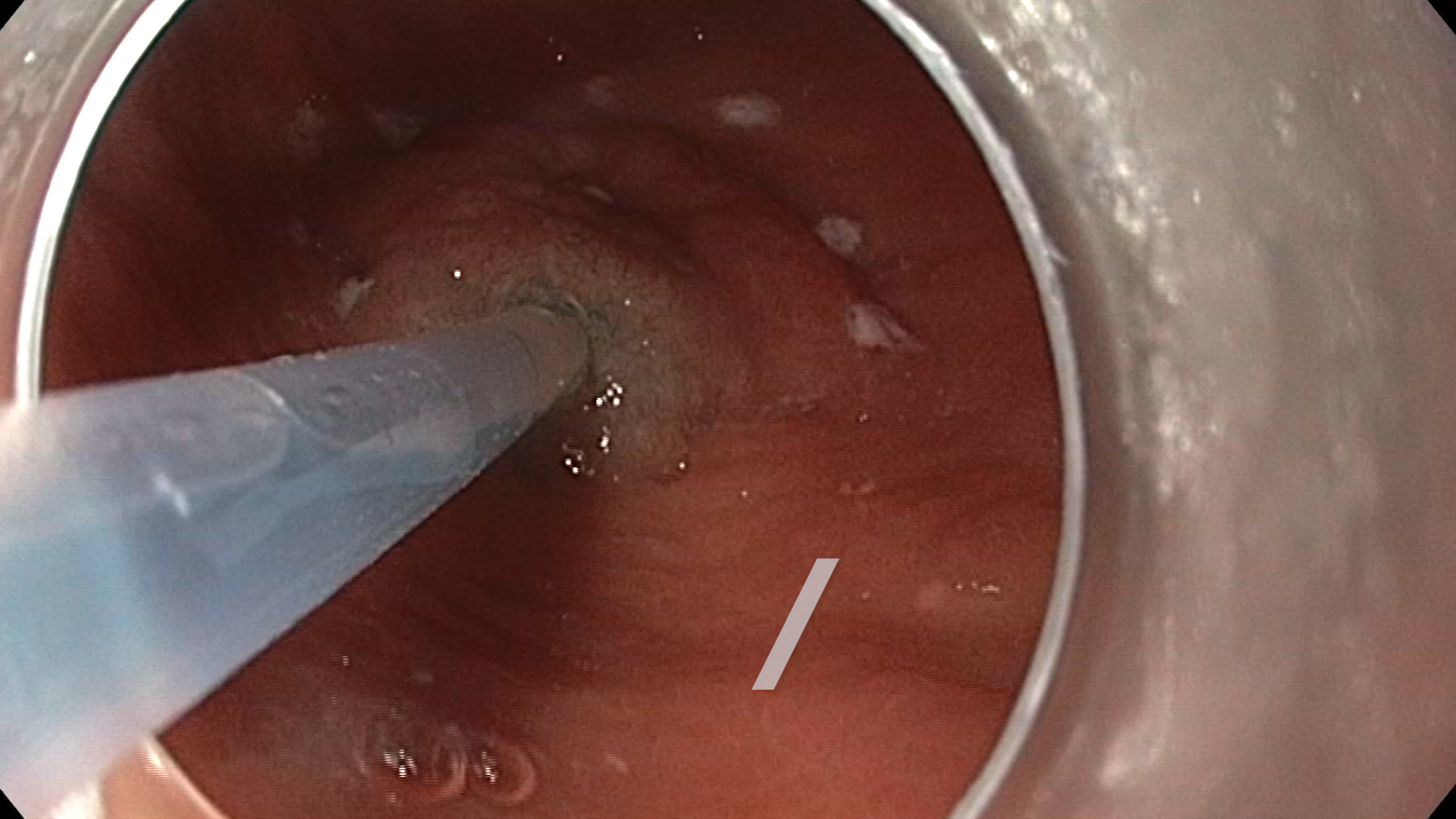
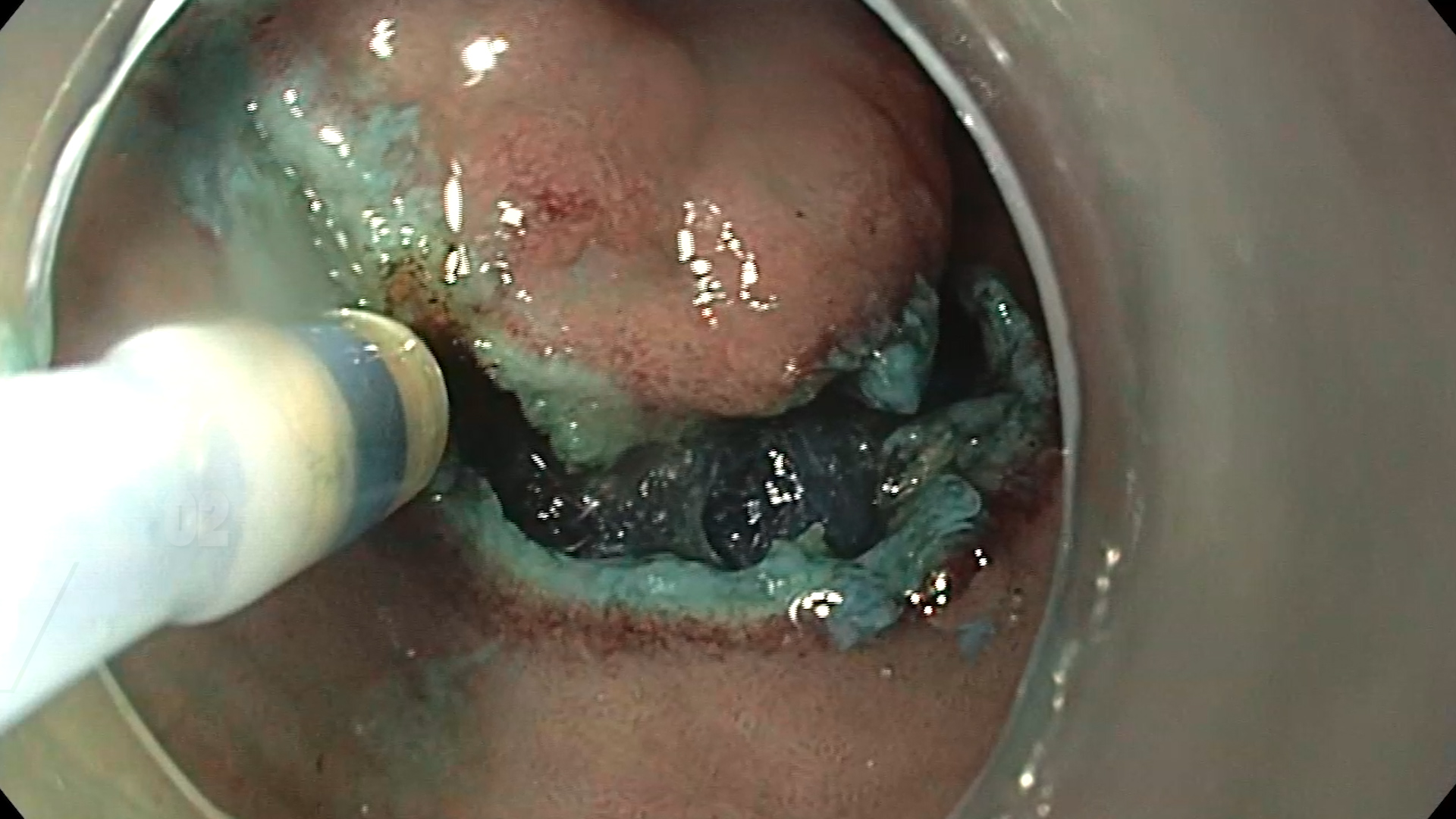
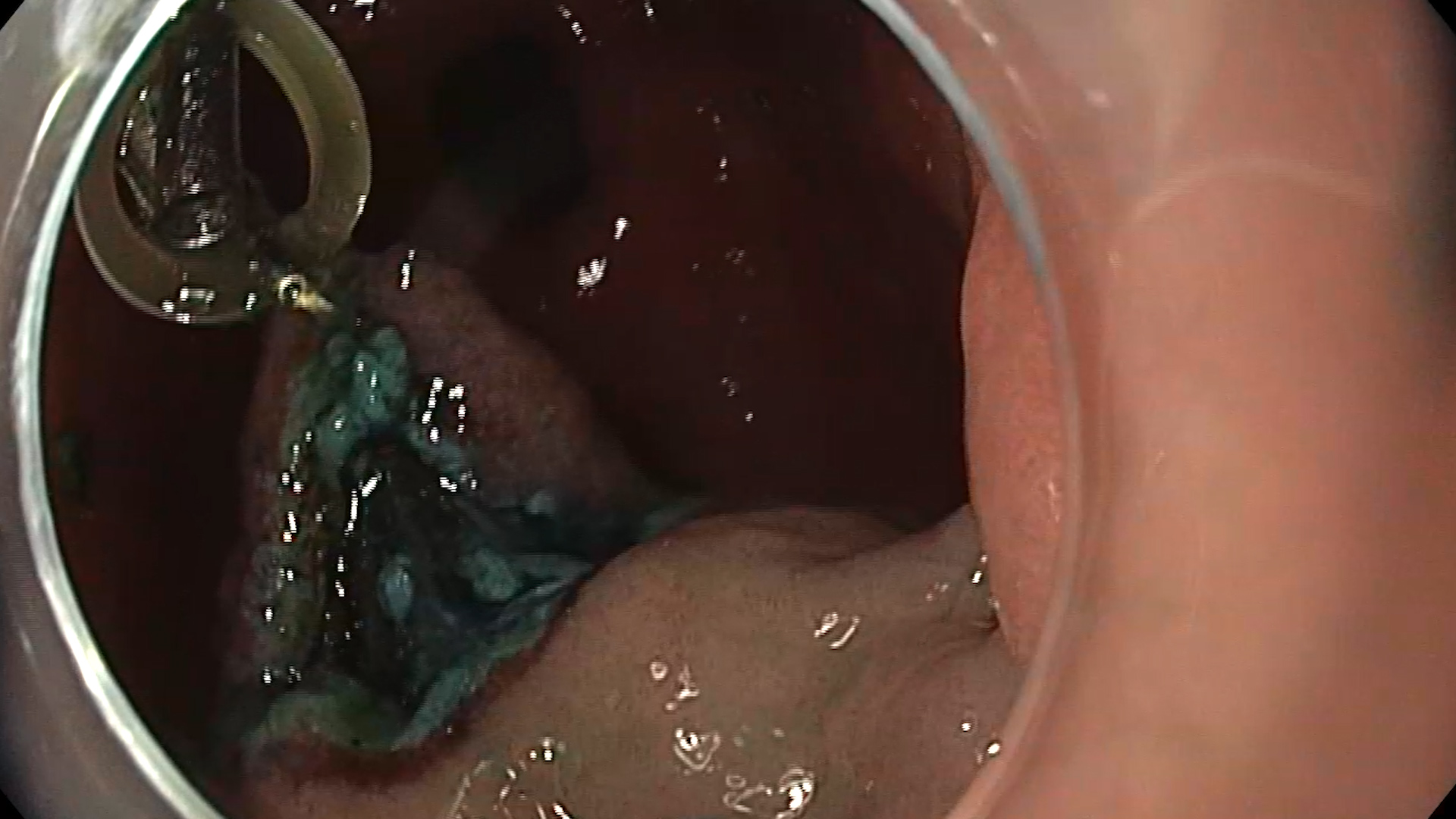
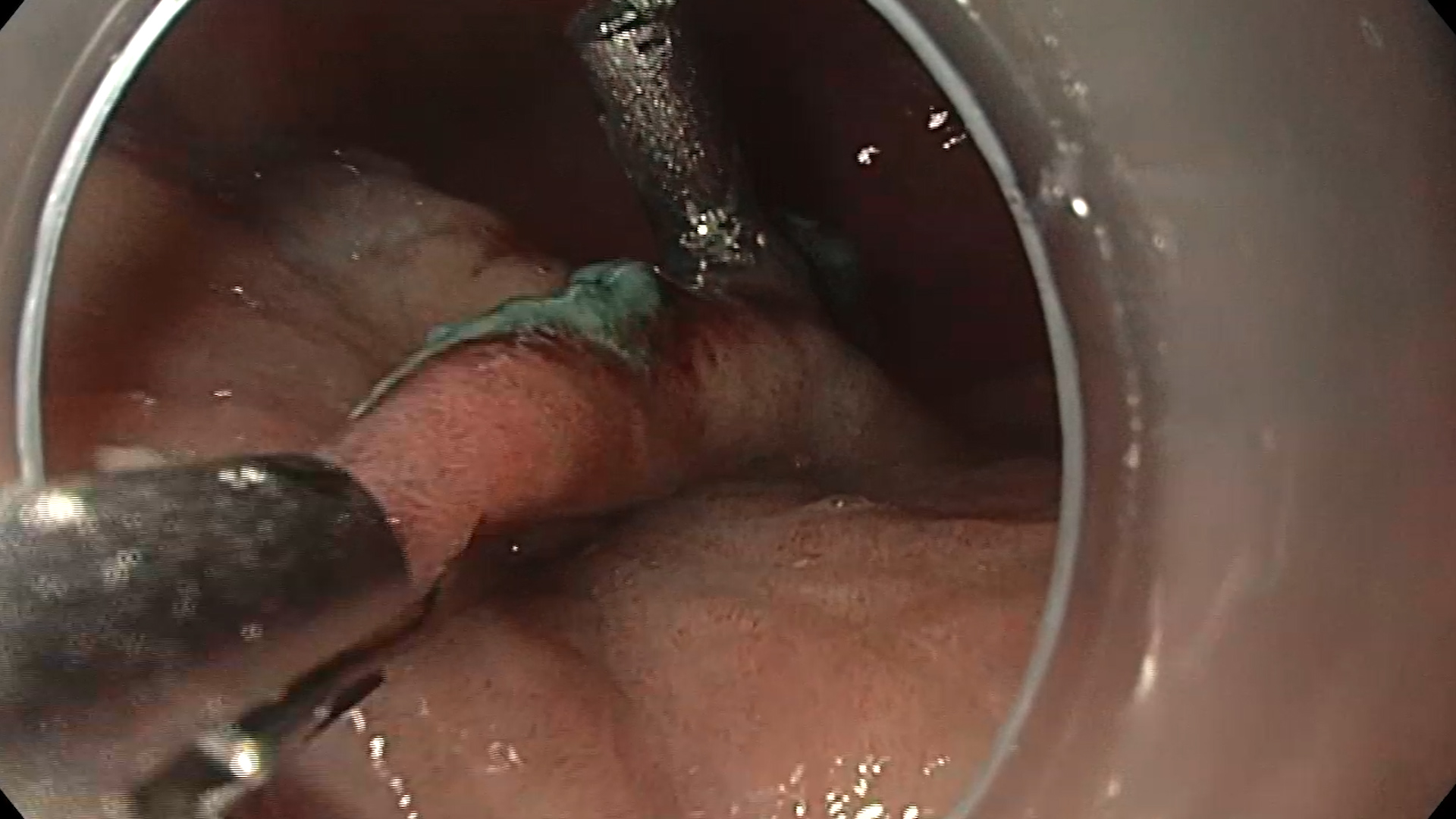
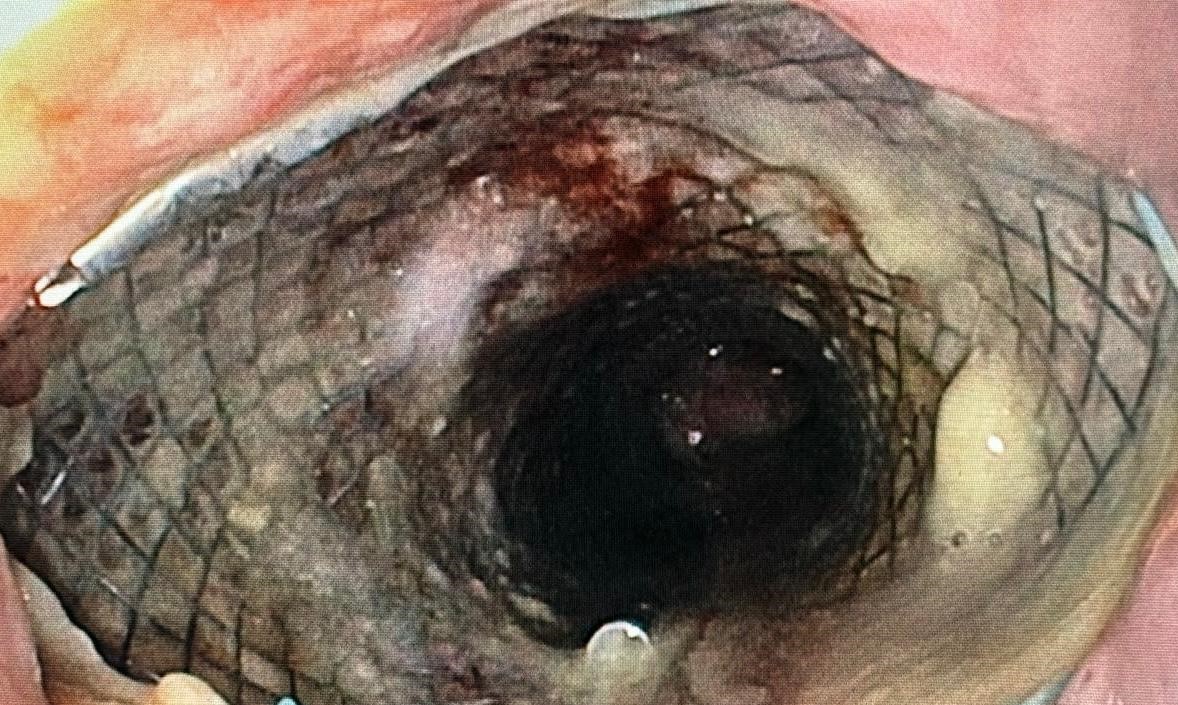
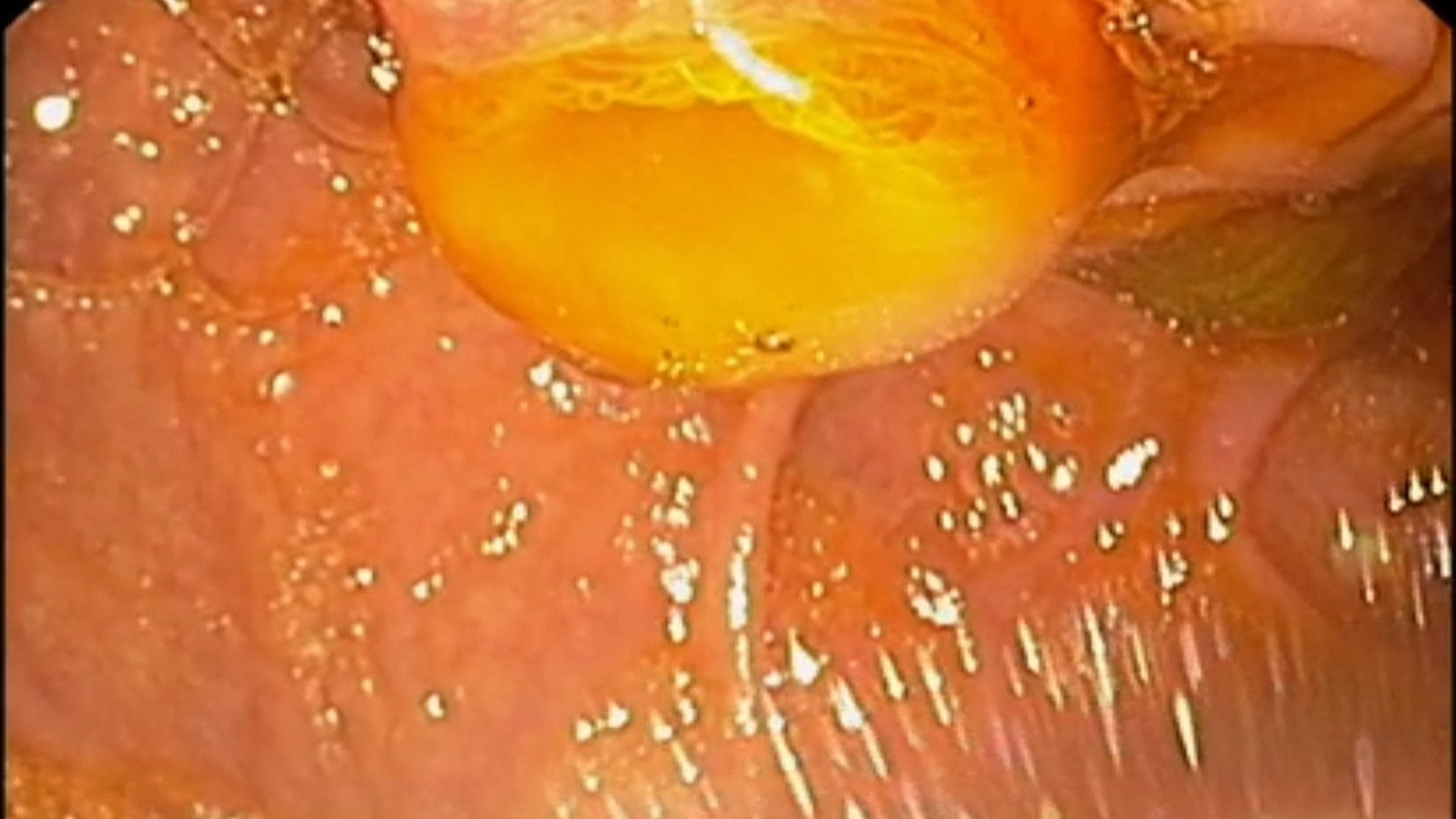
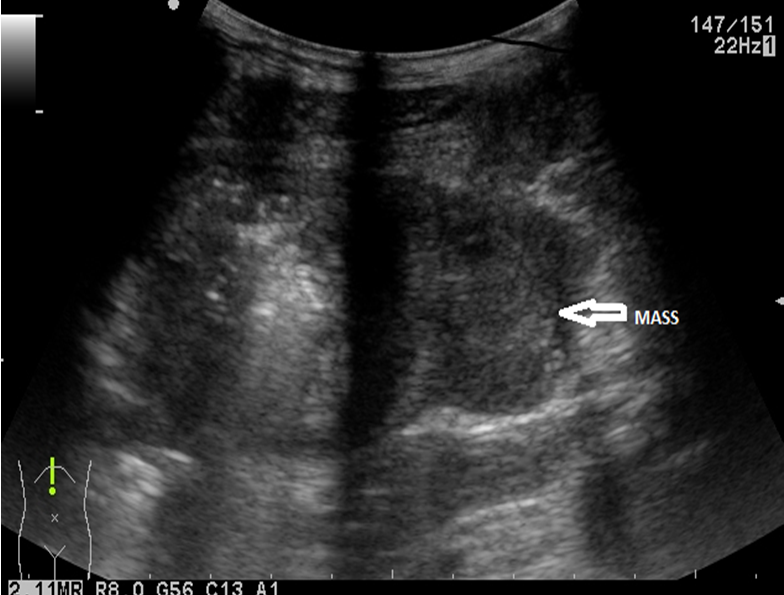
Endoscopic examination revealed an elevated antral lesion with a prior biopsy. The lesion was carefully examined in white light (Figure 1) and NBI (Figure 2) to detail the characteristics, being an elevated gastric lesion with central depression, Paris 0-IIa+IIc, approximately 10 mm in diameter, with an adenomatous appearance. Given the patient’s comorbidities, endoscopic resection of the gastric lesion was decided through submucosal dissection, after the patient was informed of the alternatives and procedural risks. The lesion outline was initially marked using the tip of a DualKnife (Olympus) and ForcedCoag current (Figure 3). A mixed solution of methylene blue was injected submucosally to elevate the lesion appropriately. The proximal incision was made using PulseCut Fast, and entry into the submucosal space was achieved; dissection continued with the knife and ForcedCoag current in the submucosa, periodically verifying the dissection trajectory (Figure 4). Traction was applied to continue dissection by mobilizing the lesion with Lockado 16mm metal clips and elastic bands (Figure 5). Dissection continued until the distal end of the lesion, after which the traction system was removed. The lesion was fully dissected and completely retrieved. The vessels at the resection base were coagulated using a CoagGrasper with ForcedCoag current, and the defect was closed with 3 MicroTech Lockado 20mm clips (Figure 6). No post-procedural complications were encountered.
Elevated antral gastric lesion Paris 0-IIa+IIc with mild dysplasia on the background of complete intestinal metaplasia.
Intestinal metaplasia is considered a precancerous lesion, most often asymptomatic, and is therefore usually diagnosed during endoscopic evaluations or after histopathological examinations1. Depending on the extent, it can be localized or diffuse, and depending on the degree of differentiation, it can be complete (with cells similar to those of the small intestine), considered the first stage of intestinal metaplasia, or incomplete (with cells resembling those of the large intestine), considered a more advanced stage with a higher risk of dysplasia. The main causes of metaplasia include: Helicobacter Pylori infection, autoimmune gastritis, certain rheumatological diseases, bile reflux, smoking, alcohol, etc. To accurately detect gastric intestinal metaplasia, the Modified Sydney System (MSS) is used, implemented since 1994, which involves obtaining biopsies from suspected endoscopic areas, as well as random biopsies from the antrum (both the lesser and greater curvatures), gastric angle, and body (lesser and greater curvatures)2.
Monitoring of patients with intestinal metaplasia is performed based on the degree of dysplasia. For patients with low-grade dysplasia, annual endoscopic evaluation with biopsies is recommended, while for patients with high-grade dysplasia without an endoscopic lesion formation, endoscopic evaluation every 6 months to 1 year is recommended. For patients with lesion formations grafted onto areas of metaplasia, proper staging and resection are recommended3.
Histopathological examination: area of complete intestinal metaplasia with low-grade dysplasia changes, resection margins of the specimen show no dysplastic features. Helicobacter Pylori was not observed in Giemsa staining.
- Costa D, Ramai D, Tringali A. Novel classification of gastric polyps: The good, the bad and the ugly. World J Gastroenterol 2024 Aug 21; 30(31): 3640-3653. PMID: 39192997
- https://my.clevelandclinic.org/health/diseases/22215-intestinal-metaplasia
- Jencks DS, Adam JD, Borum ML, Koh JM, Stephen S, Doman DB. Overview of Current Concepts in Gastric Intestinal Metaplasia and Gastric Cancer. Gastroenterol Hepatol (N Y) 2018 Feb; 14(2): 92-101. PMID: 29606921