See other cases
Focal Nodular Hyperplasia-like Lesions in a Patient with Budd Chiari Syndrome: A Case Report
A 22-year-old female patient with a history of infantile spastic tetraparesis and primary Budd Chiari syndrome (diagnosed in 2010) presented with diffuse abdominal pain and constipation.
Clinical examination revealed a conscious but hardly cooperative patient with pallor and signs of gingival bleeding. Abdominal inspection showed mild abdominal distension with visible collateral circulation, diffuse abdominal tenderness on palpation, and hepatosplenomegaly.
Biological analysis indicated moderate anemia, mild thrombocytopenia, mild hypoalbuminemia, hypocholesterolemia, elevated GGT levels, therapeutic INR, and normal AFP levels.
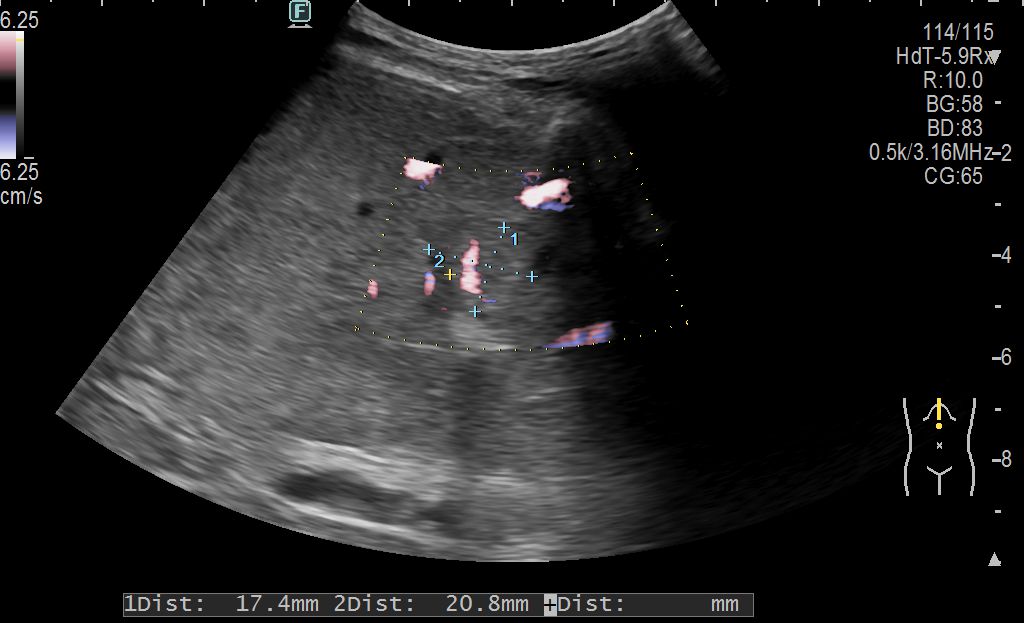
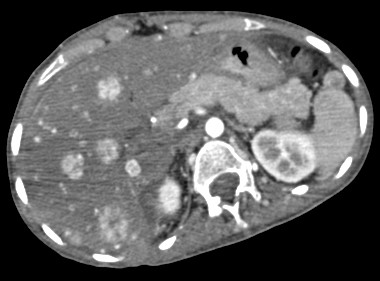
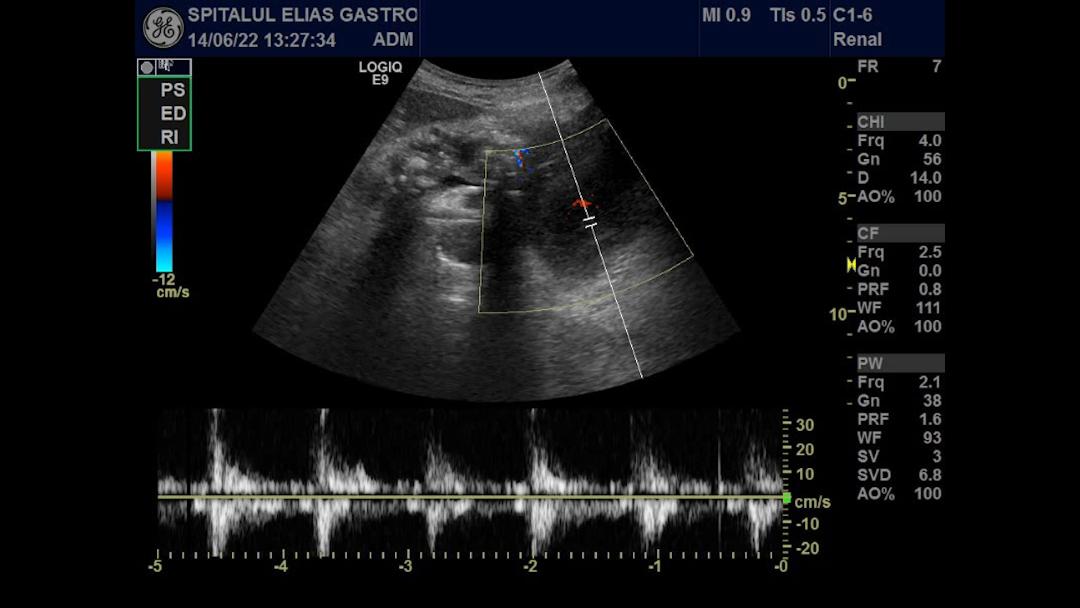
Abdominal ultrasound revealed non-homogeneous hepatomegaly with multiple hypoechoic nodules (Figure 1), moderate splenomegaly, enlarged hepatic veins with incomplete filling, and multiple collateral subcapsular vessels.
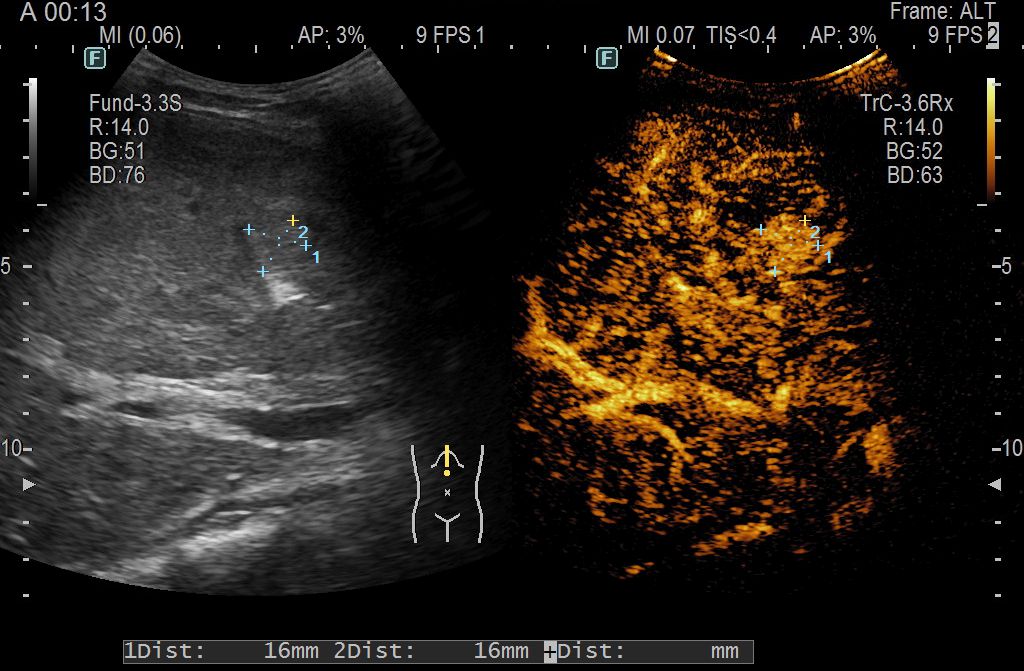
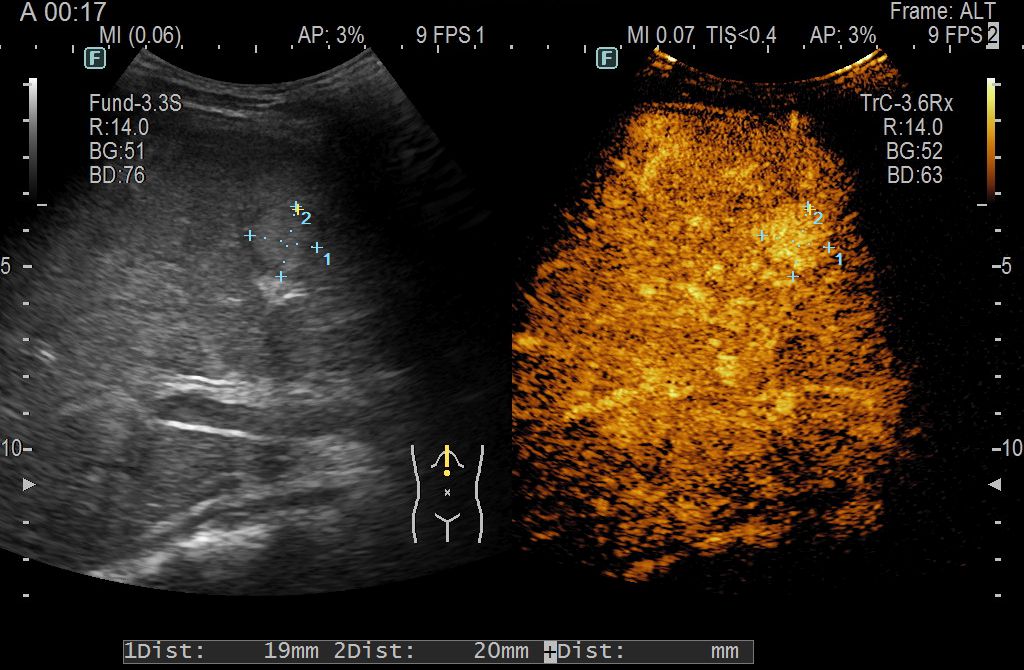
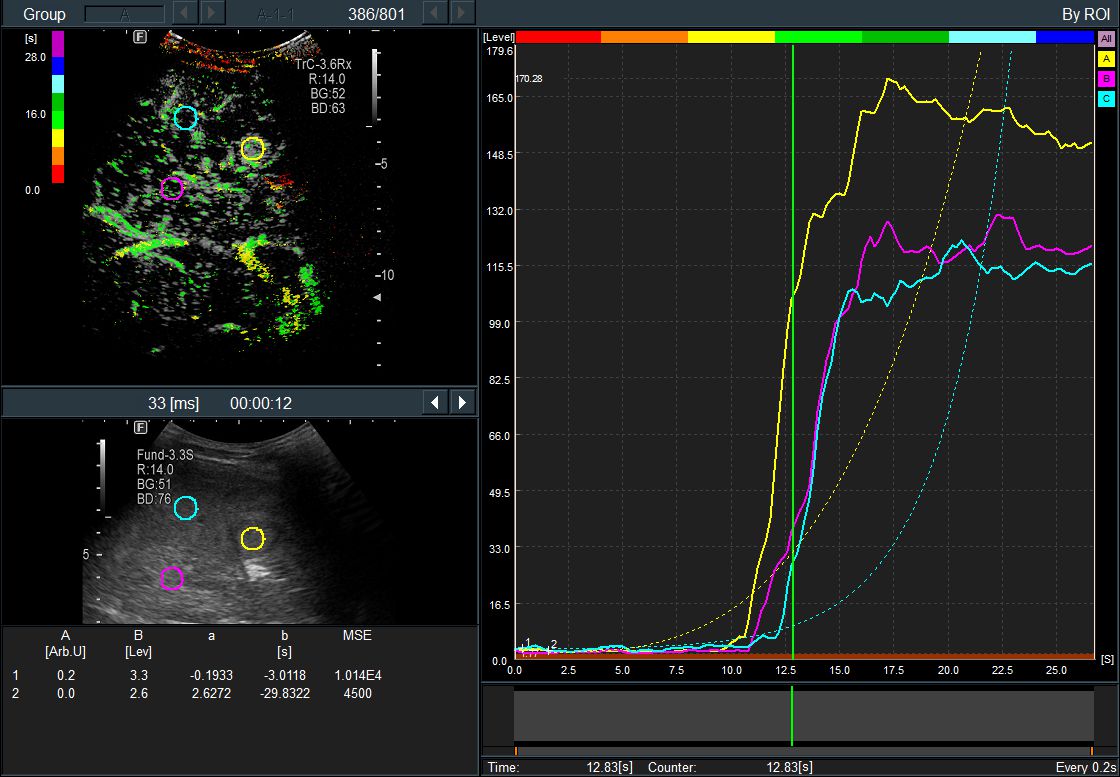
Contrast-enhanced ultrasound (CEUS) demonstrated nodules with rapid homogeneous centrifugal hyperenhancement in the arterial phase (Figure 2), followed by isoenhancement in the portal-venous (Figure 3) and delayed phases, consistent with focal nodular hyperplasia (FNH). Time intensity curve (TIC) analysis show the same hyperenhanced appearance as compared to the surrounding liver parenchyma (Figura 4).
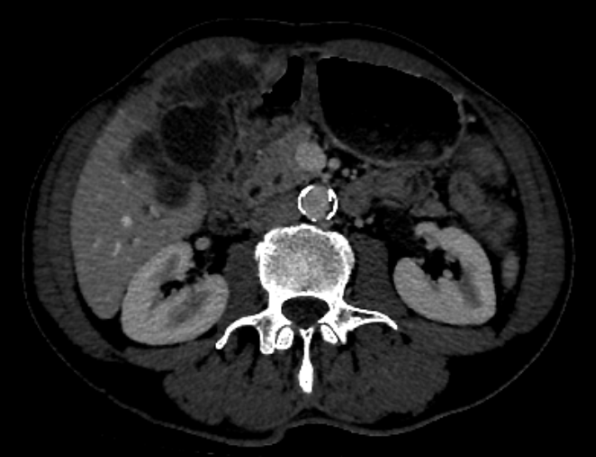
Contrast-enhanced computed tomography (CE-CT) revealed similar findings as CEUS (Figure 5), along with intrahepatic inferior vena cava (IVC) hypoplasia, abnormal perfusion, and intra- and extrahepatic collaterals.
The patient was diagnosed with Budd Chiari Syndrome accompanied by large regenerative nodules resembling focal nodular hyperplasia (FNH-like lesions).
Budd-Chiari syndrome is a relatively rare vascular complication in liver diseases, characterized by obstruction of the suprahepatic veins, leading to hepatic congestion. Chronic liver congestion can eventually lead to liver fibrosis, cirrhosis, and hepatocellular carcinoma (HCC). Focal hepatic nodules are a common finding in patients with chronic Budd-Chiari syndrome. They occur as a result of a chronic decrease in portal blood flow, followed by a compensatory increase in arterial blood supply to the liver parenchyma.
Most of these nodules are benign and correspond to regenerative lesions called focal nodular hyperplasia-like (HNF-like) lesions. Because of their predominant arterial supply, these nodules show significant arterial uptake that persists in the portal-venous and late phases on CE-CT, CE-MRI, and CEUS. It is important to note that, in addition to its simplicity and accessibility, CEUS also allows for “real-time” evaluation of liver nodules. Therefore, the centrifugal capture pattern (spoke-wheel-like filling) or the presence of non-capture areas (central scar) can be seen more easily.
The incidence of HCC in patients with Budd-Chiari syndrome is similar to that found in patients with other chronic liver diseases (4-17%). Recent studies have confirmed that routine screening for HCC is only necessary in the presence of cirrhosis. Hypoenhancement in the portal-venous and late phases (wash-out phenomenon) is a well-known characteristic of malignant nodules, differentiating them from most similar FNH-like nodules encountered in Budd-Chiari syndrome. In cases of atypical regenerative nodules (isolated/solitary) with wash-out phenomenon, the use of contrast agents with hepatic MRI may help the diagnosis, the iso- or hyperintense appearance in the hepatobiliary phase supporting the benign character.
a) Liver nodules are frequently observed in patients with Budd Chiari syndrome and should be assessed by integrating imaging, laboratory, and clinical data. b) CEUS is a simpler and faster technique that accurately characterizes FLLs in Budd Chiari syndrome, reducing the need for follow-up CT/MRI scans, particularly in patients without cirrhosis. c) Besides assessing FLLs, attention should also be given to other vascular and parenchymal changes associated with Budd Chiari syndrome, as they hold diagnostic and prognostic significance.
[1] Bansal V, Gupta P, Sinha S, et al. Budd-Chiari syndrome: imaging review. Br J Radiol 2018 Dec; 91(1092): 20180441. doi: 10.1259/bjr.20180441.
[2] Brancatelli G, Vilgrain V, et al. Budd-Chiari Syndrome: Spectrum of Imaging Findings. American Journal of Roentgenology, Volume 188, Issue 2, 2007, https://doi.org/10.2214/AJR.05.0168.
[3] Gaillard F, Šedivý O, Knipe H, et al. Focal nodular hyperplasia. Reference article, Radiopaedia.org, 2009. https://doi.org/10.53347/rID-6749
[4] Wester A, Aberg F, Rajani R, Hagstrom H, Minimal Risk of Hepatocelullar Carcinoma in Noncirrhotic Budd-Chiari Syndrome: A Three-Decade Population-Based Study. Clin Gastroenterol Hepatol 2022 Sep 8; S1542-3565(22)00838-2. doi: 10.1016/j.cgh.2022.08.042.