See other cases
Flat elevated LST-NG of the descending colon
A 74-year-old woman presented for follow-up colonoscopy 7 years after resection of pedunculated colonic polyps.
Normal.
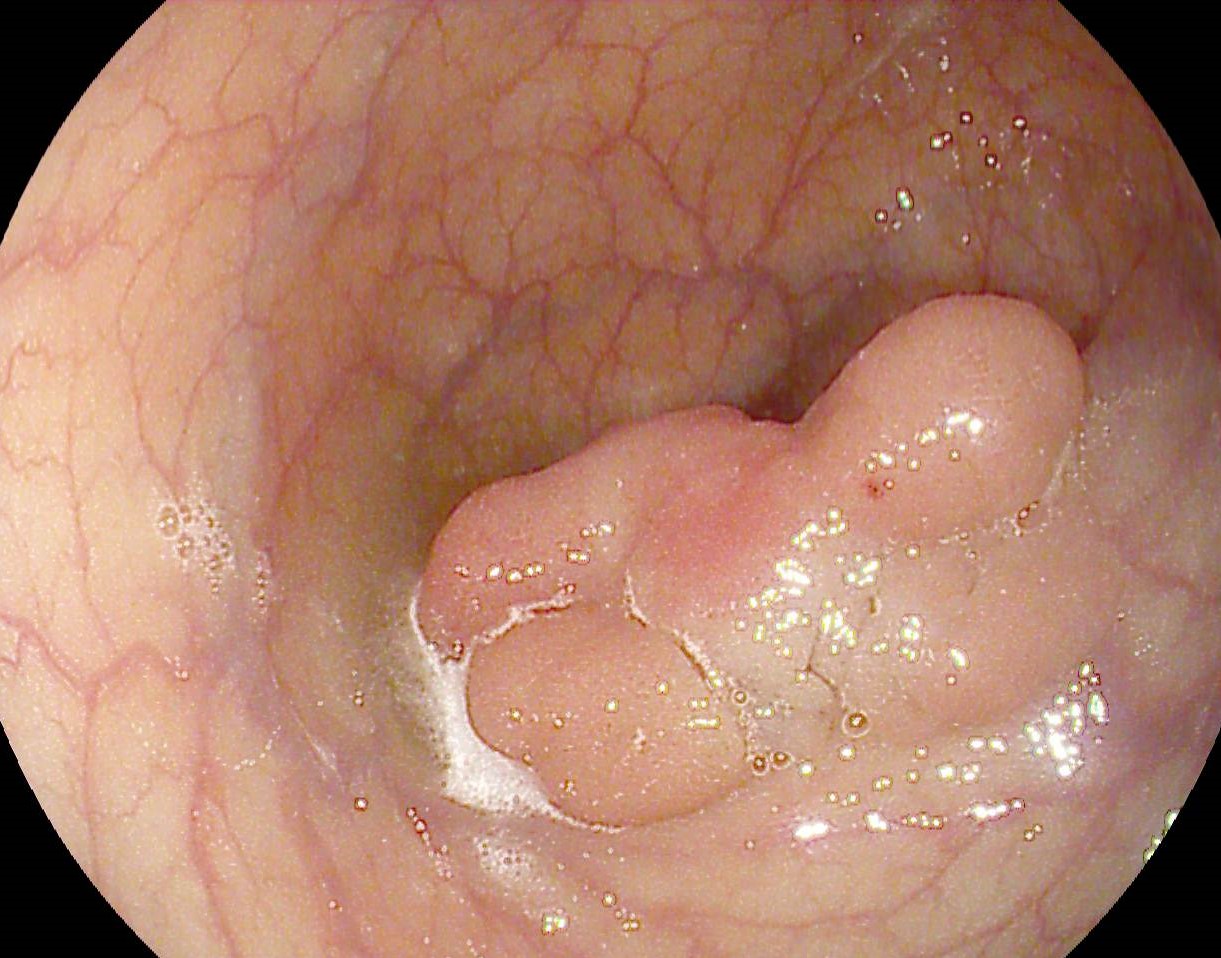
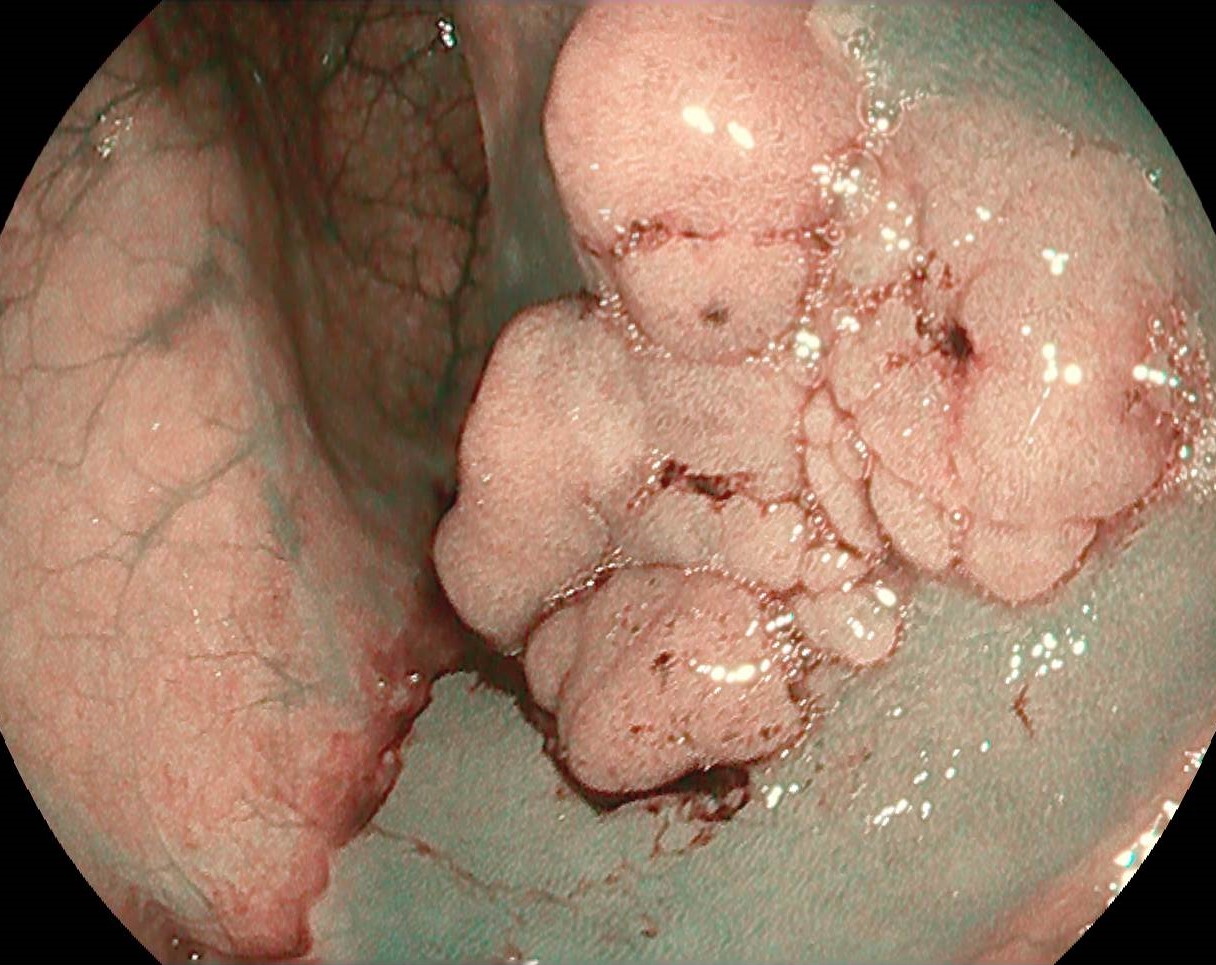
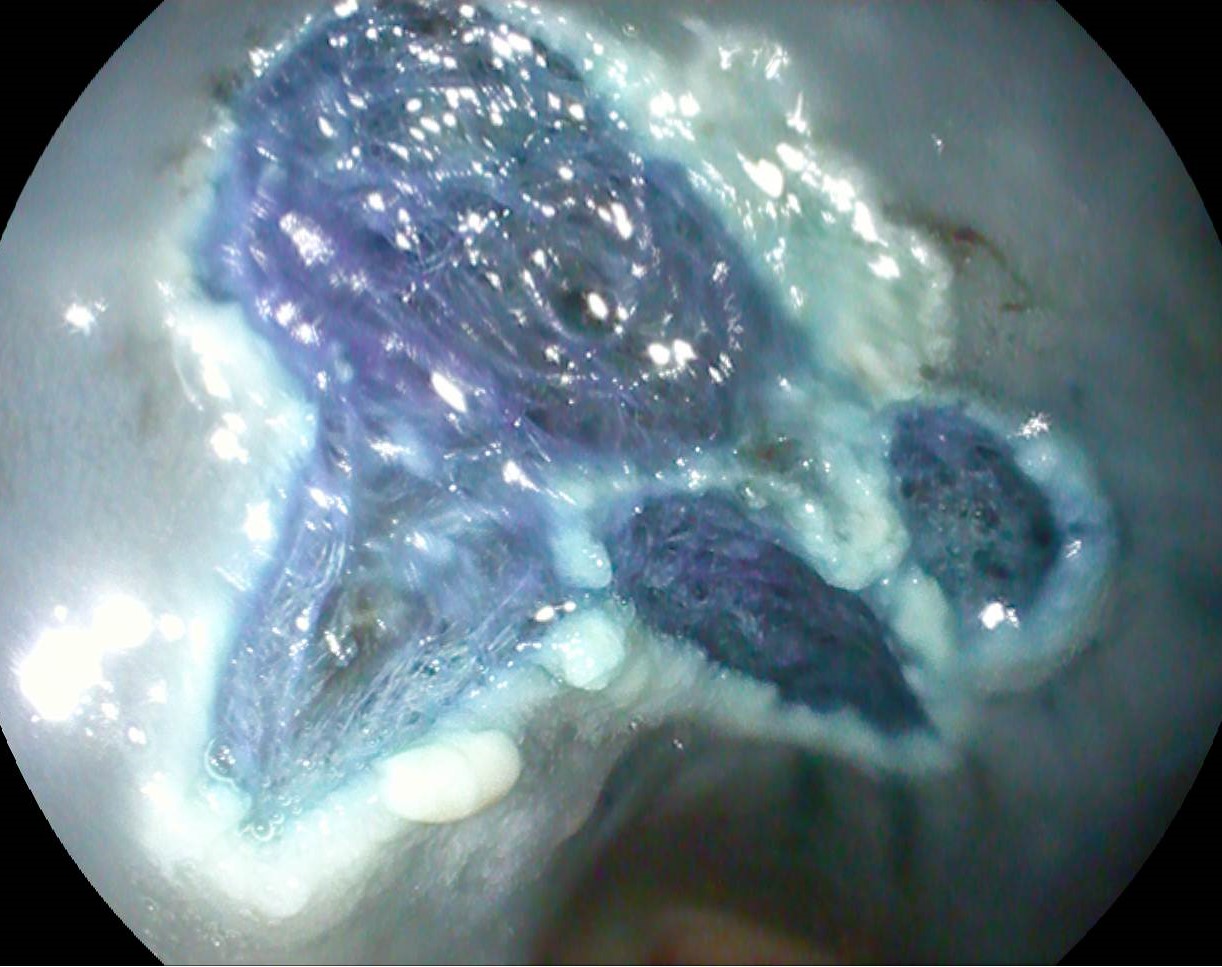
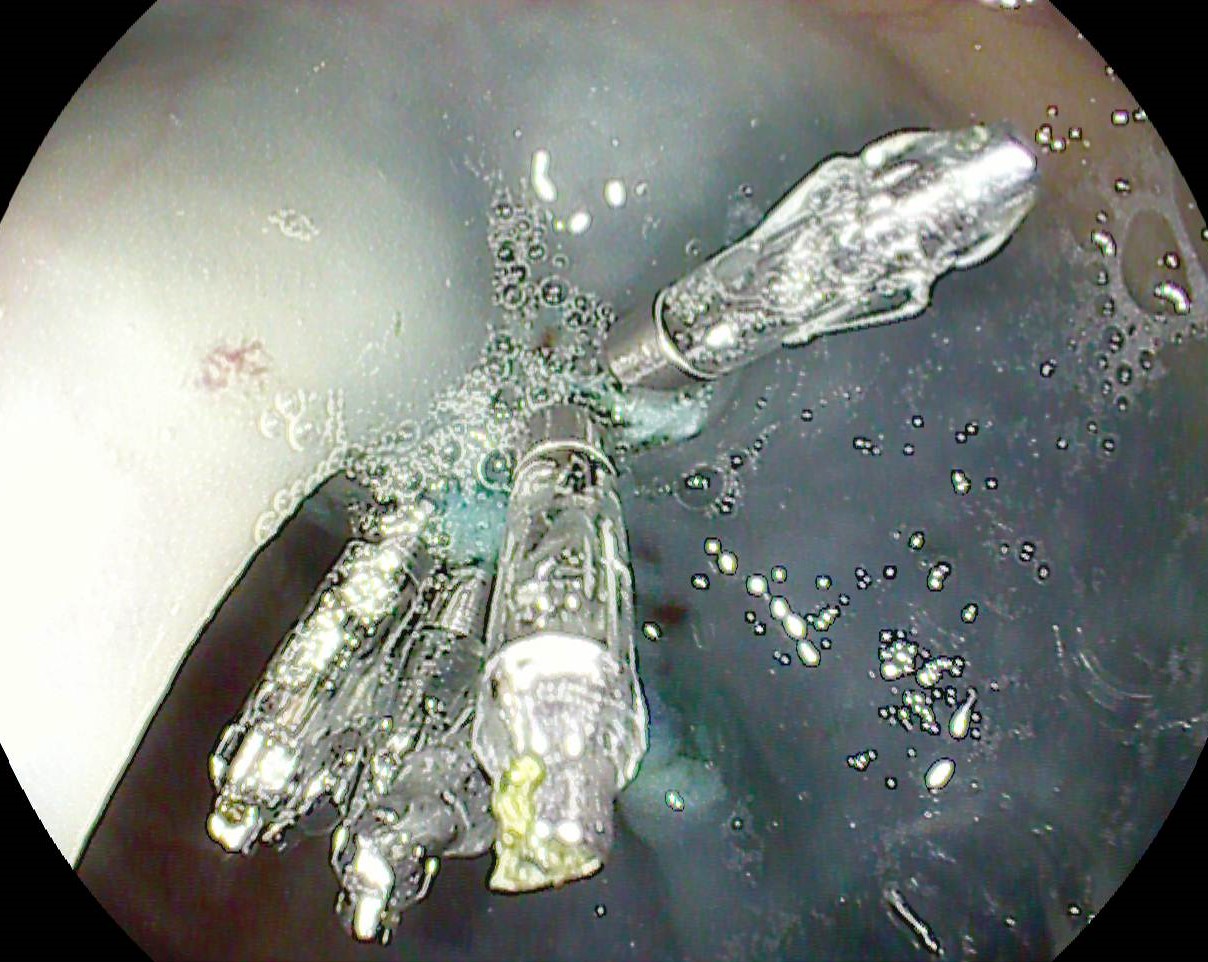
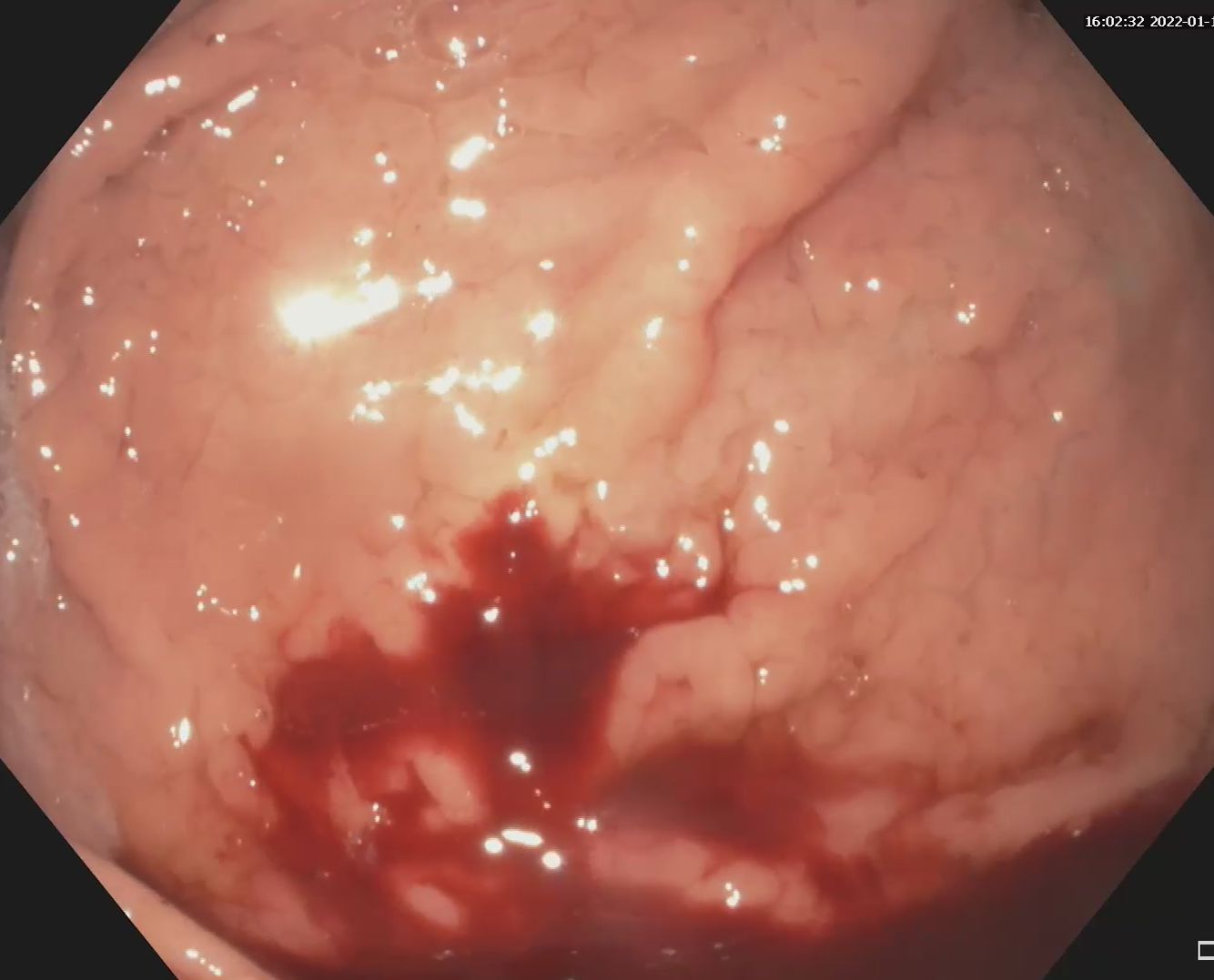
Lower gastrointestinal endoscopy visualized a flat-elevated polyp with lateral spreading in the descending colon, non-granular, irregular, with size of approximately 25/20 mm (Fig. 1). The lesion was classified as Paris 0-IIa, KUDO IIIs, NICE 2 (JNET 2A) (Fig. 2). Piece-meal endoscopic mucosal resection (piece-meal endoscopic mucosal resection – pEMR) was performed, with subsequent recovery of the fragments for histopathological examination (Fig. 3, Film 1). Finally, the edges of the resulting defect were coagulated with argon plasma (APC), and the defect was closed with 6 hemostatic clips (Fig. 4).
The diagnosis based on the histopathological examination revealed a tubulo-villous adenoma with low and high degree focal dysplasia.
Lesions with lateral extension (lateral spreading tumors – LST) of the non-granular type are associated with a relatively higher risk of submucosal invasion (approx. 5%), whilst resection is more difficult due to fibrosis and possible invasion into the submucosa [1-3 ]. Elevation of the flat lesion after submucosal injection (generally succinylated gelatin and/or adrenaline 1:10,000, with methylene blue) is a critical factor for endoscopic resection which can be difficult or even impossible. Compared to LST-G type lesions, LST-NG type lesions appear to be different from a histological point of view, with a flat disposition of the muscularis mucosae, as well as a better vascularized submucosa, but with similar fibrosis (except for cases in which cold biopsies were taken) [4].
The resection is difficult to perform in a single fragment (“en bloc”), when the dimensions of the lesion allow it (generally below 20 mm), or in multiple fragments, through the piece-meal technique (pEMR). pEMR is characterized by a good safety profile but is associated with a recurrence risk of approximately 15%. Although less accessible, the endoscopic submucosal dissection (ESD) technique is superior to EMR in terms of complete and en bloc resection rates, while being associated with a lower recurrence rate.
Endoscopic mucosal piece-meal resection (pEMR) remains the preferred method for resection of LST lesions, especially in the absence of ESD availability.
- Kaltenbach T, Anderson JC, Burke CA, Dominitz JA, Gupta S, Lieberman D, Robertson DJ, Shaukat A, Syngal S, Rex DK. Endoscopic Removal of Colorectal Lesions: Recommendations by the US Multi-Society Task Force on Colorectal Cancer. Am J Gastroenterol 2020; 115: 435-464.
- Ferlitsch M, Moss A, Hassan C, Bhandari P, Dumonceau JM, Paspatis G, Jover R, Langner C, Bronzwaer M, Nalankilli K, Fockens P, Hazzan R, Gralnek IM, Gschwantler M, Waldmann E, Jeschek P, Penz D, Heresbach D, Moons L, Lemmers A, Paraskeva K, Pohl J, Ponchon T, Regula J, Repici A, Rutter MD, Burgess NG, Bourke MJ. Colorectal polypectomy and endoscopic mucosal resection (EMR): European Society of Gastrointestinal Endoscopy (ESGE) Clinical Guideline. Endoscopy 2017; 49: 270-297.
- Russo P, Barbeiro S, Awadie H, Libânio D, Dinis-Ribeiro M, Bourke M. Management of colorectal laterally spreading tumors: a systematic review and meta-analysis. Endosc Int Open 2019; 7: E239-E259.
- Goto SP, Sakamoto N, Mitomi H et al. Histological Distinction between the Granular and Nongranular Types of Laterally Spreading Tumors of the Colorectum. Gastroenterol Res Practice 2014; 153935.