See other cases
Extraintestinal manifestations in IBD
We present the case of a 35-year-old man, with a history of ulcerative proctosigmoiditis for almost 10 years, non-compliant with oral 5ASA and local suppository treatment, who presented with painful lesions on the right calf.
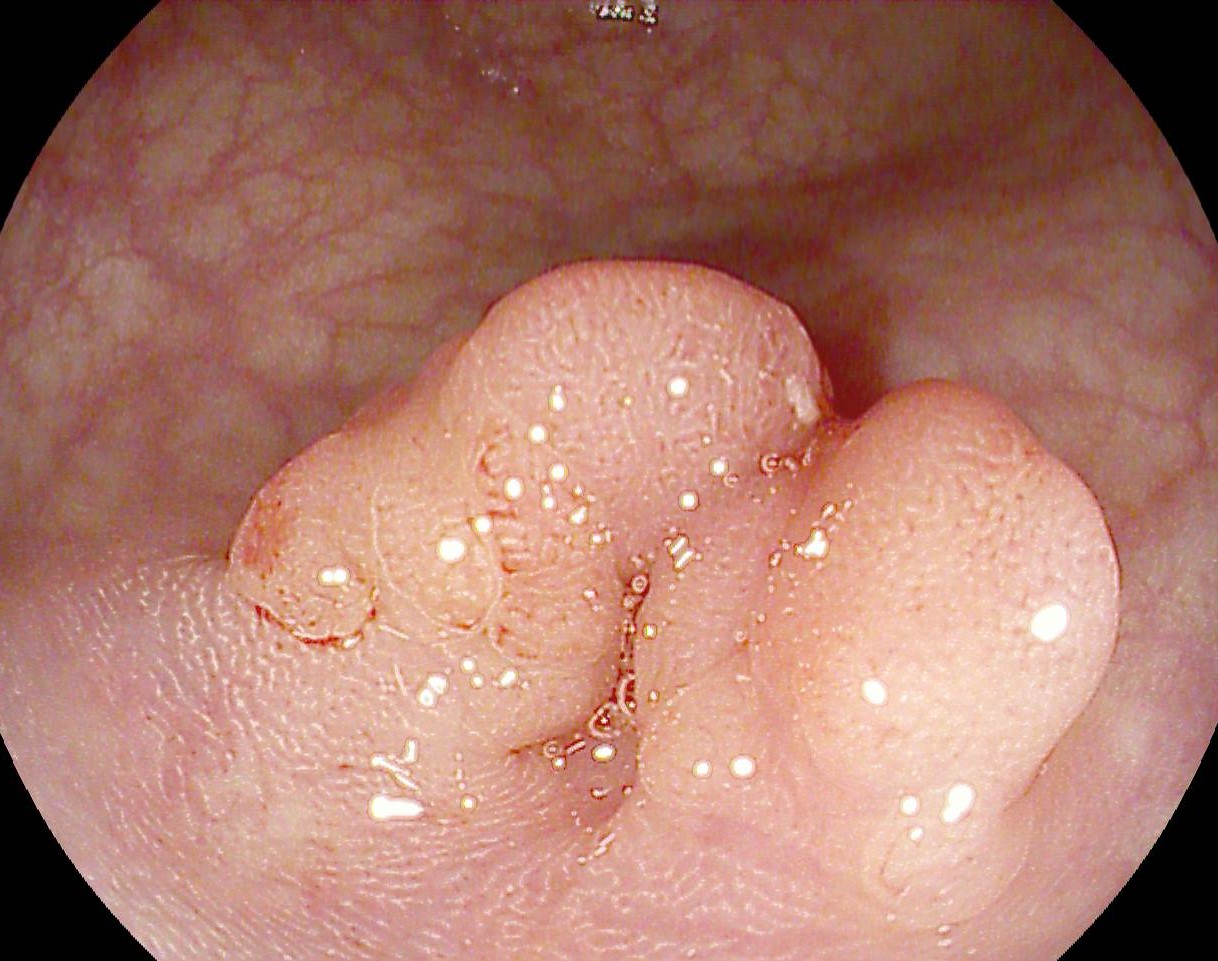
Clinical: two ulcers on the antero-medial surface of the right calf, with violet, irregular edges that rapidly progressed in size, with necrosis of the margins.
After sampling cultures and biopsies from the lesions, the wound was cleaned and local as well as intravenous corticotherapy was administered. Later, the corticotherapy was switched to oral administration with tapering of the doses with the gradual epithelization of the lesions. During the healing of the skin lesions, approximately 2 months after their appearance, the patient presented with intense dyspnea and chest pain.
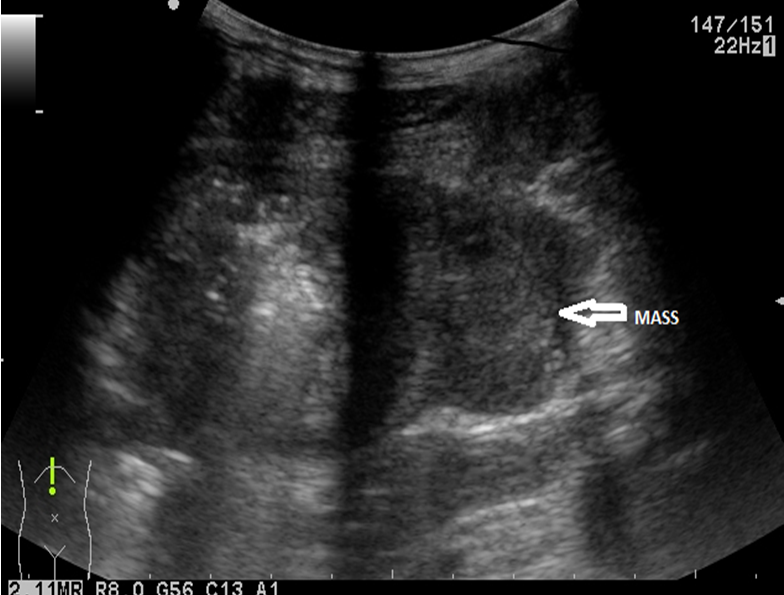
Biological: minimal inflammatory syndrome (CRP 11 mg/l, ESR 30 mm/h) and increased D-Dimers. Chest contrast enhanced computed tomography and Doppler ultrasound of the lower limbs were performed, which revealed the presence of bilateral pulmonary thromboembolism and a thrombus in the right popliteal vein of approximately 3 cm. Anticoagulant therapy was initiated initially subcutaneously, later orally with rapid tapering of corticotherapy with favorable evolution.
The patient refused biological therapy and remained in clinical and endoscopic remission under treatment with oral 5-ASA. Approximately 4 years after the resolution of the skin lesions, patient develop bilateral palmar plaques with erythema and scales, suggestive of palmar psoriasis.
Ulcerative proctosigmoiditis in clinical and endoscopic remission with extraintestinal manifestations.
Pyoderma gangrenosum is a neutrophilic dermatosis, frequently associated with autoimmune pathologies and solid or hematological neoplasms. In patients with inflammatory bowel disease (IBD), it is more common for ulcerative colitis, and may not be associated with exacerbation of intestinal manifestations. The characteristic lesions are initially erythematous nodules or macules, intensely painful, with rapid evolution towards ulcers and necrosis. There is no gold standard treatment for pyoderma, but management includes therapy of the underlying disease, systemic corticosteroid therapy and local immunosuppression (Tacrolimus ointment, Cyclosporine).
Patients with IBD also have a 3 fold increased risk of deep vein thrombosis and pulmonary thromboembolism, and during exacerbations and corticosteroid therapy this risk increases up to 8 fold compared to the general population.
Psoriasis and IBD can be associated in 2-10% of cases; at the same time, psoriasis-like lesions can be induced by the biological therapy recommended for IBD, not being the case of our patient.
Both palmar psoriasis and pyoderma gangrenosum are debilitating extraintestinal manifestations that considerably decrease the quality of life in patients with IBD. It is important to recognize this pathology from a clinical point of view, the diagnosis being one of exclusion, because the early administration of therapy can lead to the healing of these rapidly evolving lesions. Also, in patients not yet diagnosed with IBD, the identification of pyoderma gangrenosum leads to endoscopic investigations that can reveal intestinal lesions.
- Schmieder SJ, Krishnamurthy K. Pyoderma Gangrenosum. [Updated 2022 Aug 21]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-.
- Gerhard Rogler, Abha Singh, Arthur Kavanaugh, David T.Rubin. Extraintestinal Manfiestations of Inflammatory Bowel Disease: Current Concepts, Treatment, and Implications for Disease Management. Gastroenterology. (161):1118–32.