See other cases
EUS-guided RFA of an insulinoma
A 49-year-old female, with no significant past medical history, who was initially evaluated because of rapid weight gain and increase in appetite due to episodes of hunger, dizziness and sweating.
Clinic: obesity (BMI = 35,2)
Biologic: hypoglycemia (47 mg/dL), hyperinsulinemia (15,3 µU/mL). The remaining work-up was within normal limits.
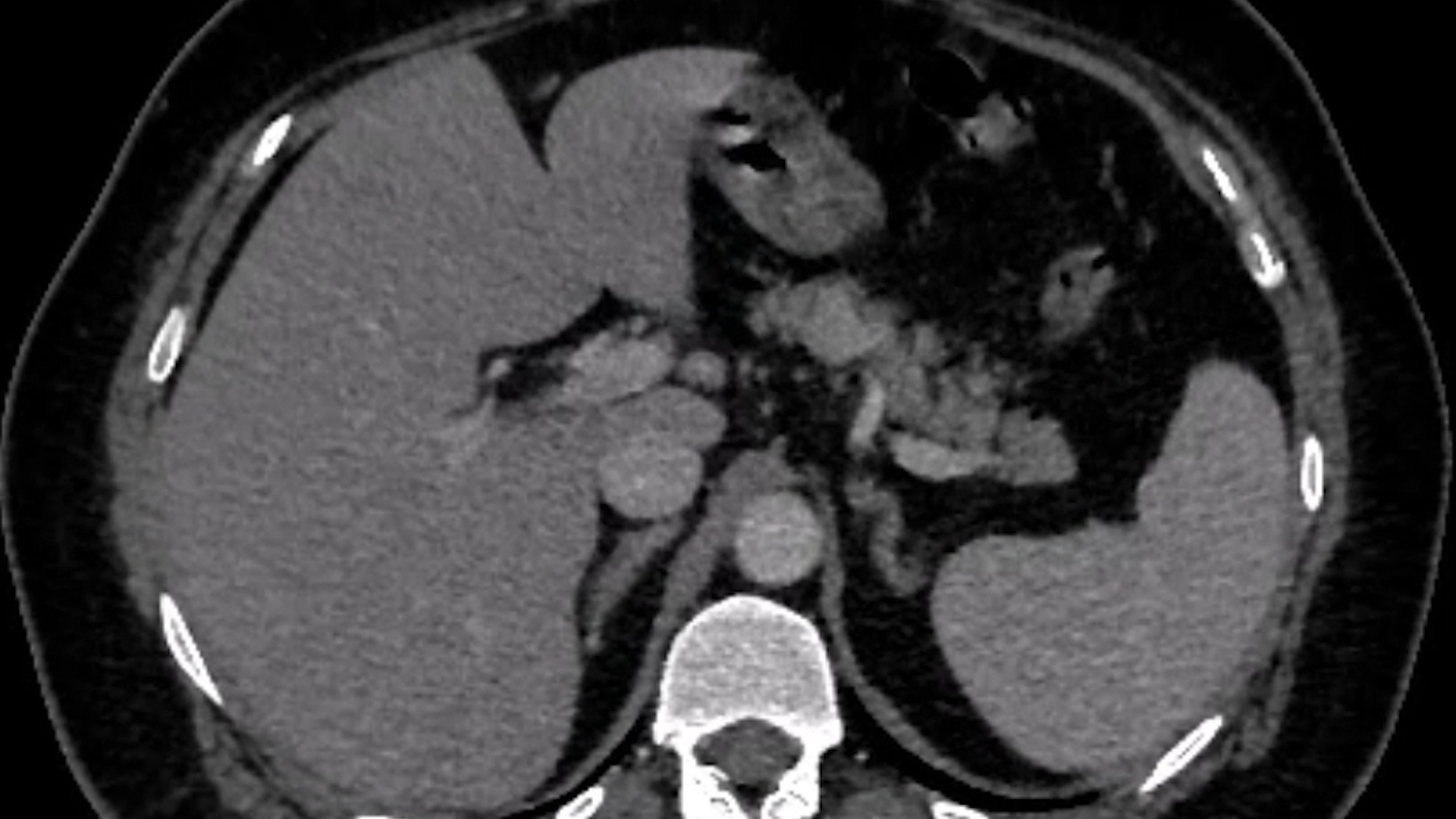
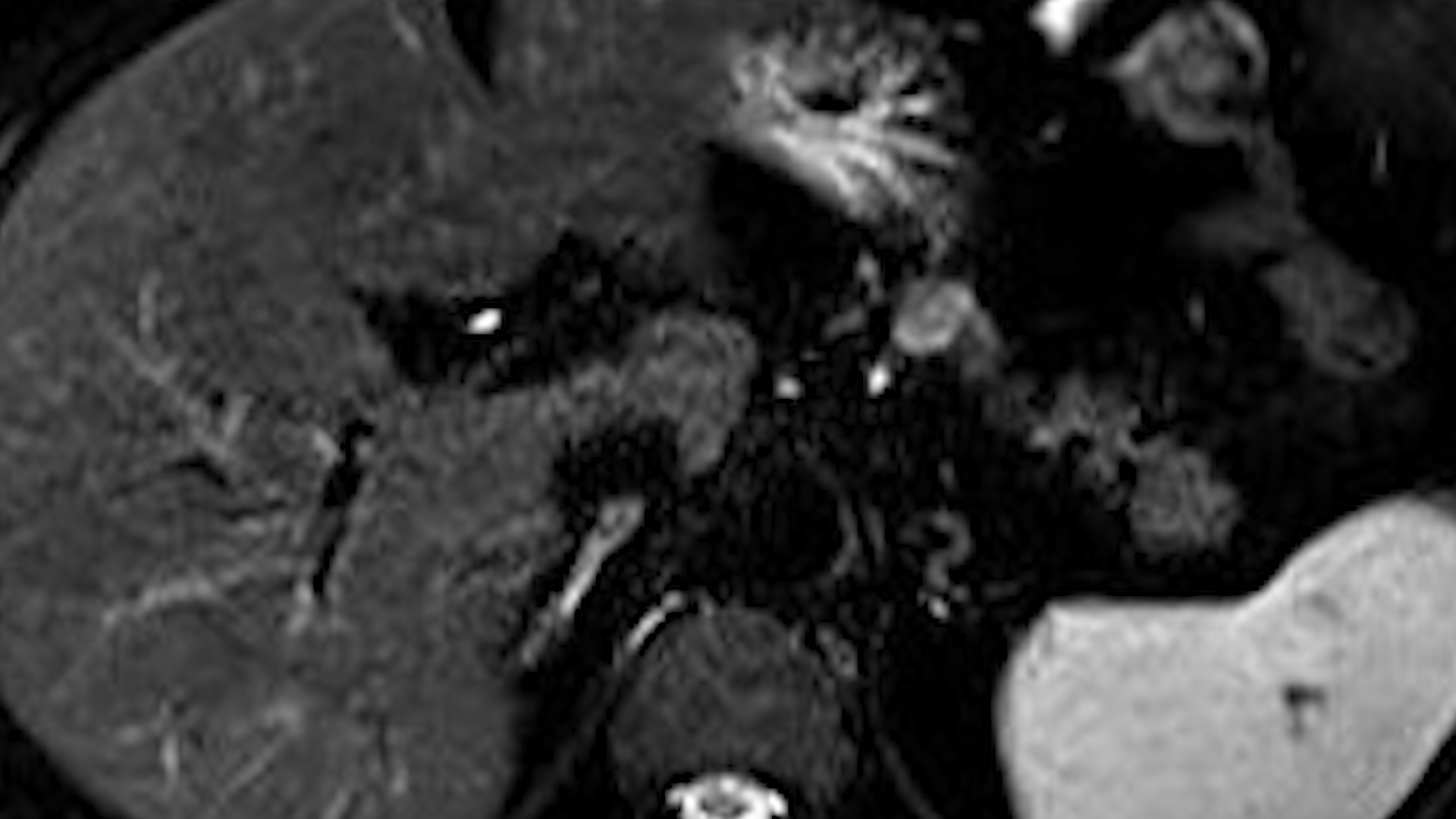
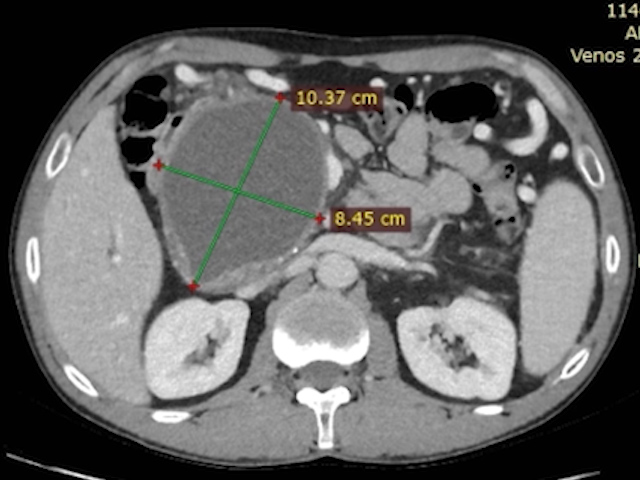
A contrast-enhanced CT scan was ordered (Fig. 1), which showed a 16/22 mm arterial hyperenhanced pancreatic body tumor, in proximity with the splenic artery and vein. MRI with gadolinium revealed the same hyper-enhancing pattern of the pancreatic body tumor on T2-weighted images, with slight restriction on DWI/ADC (Fig. 2).
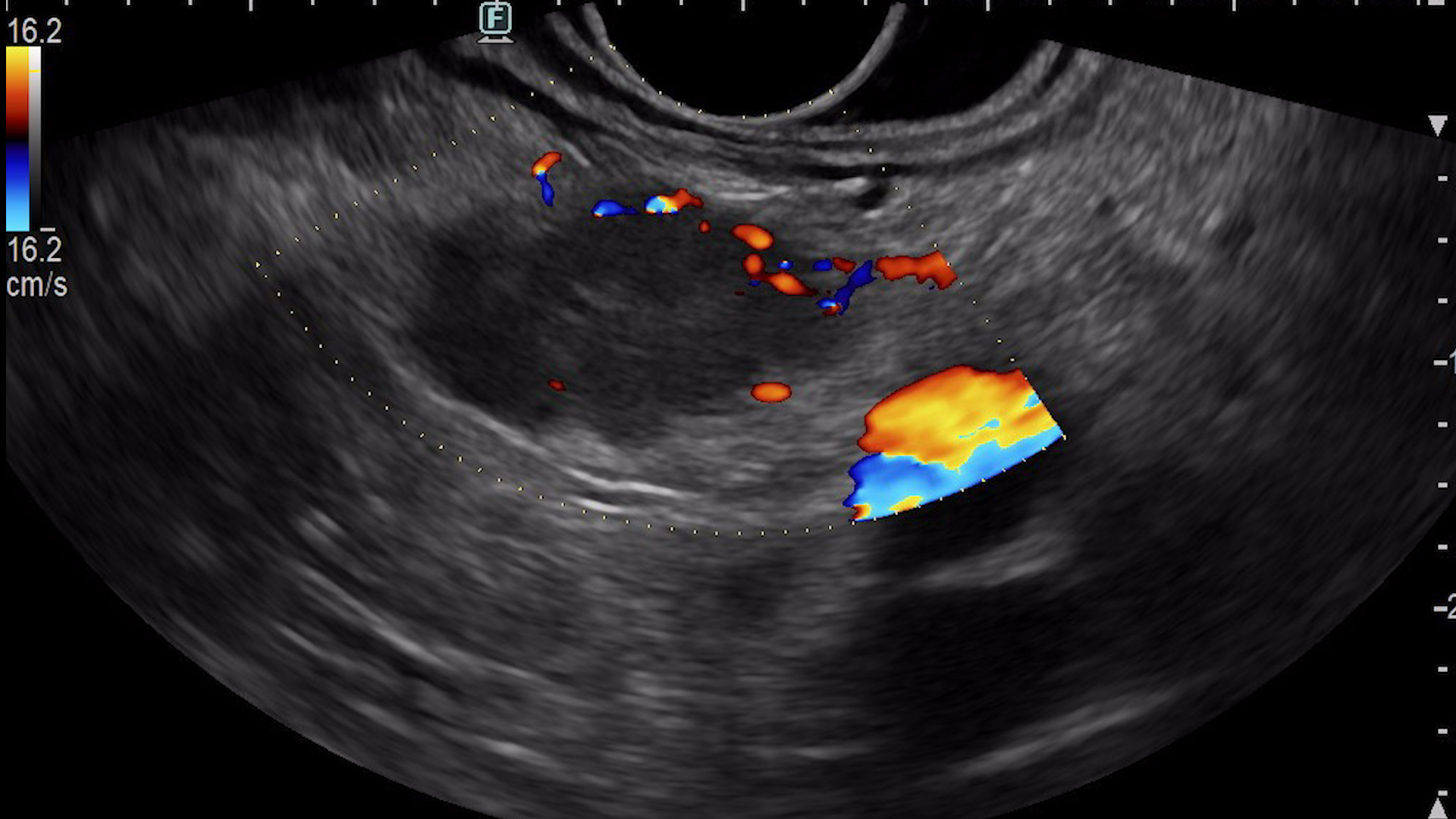
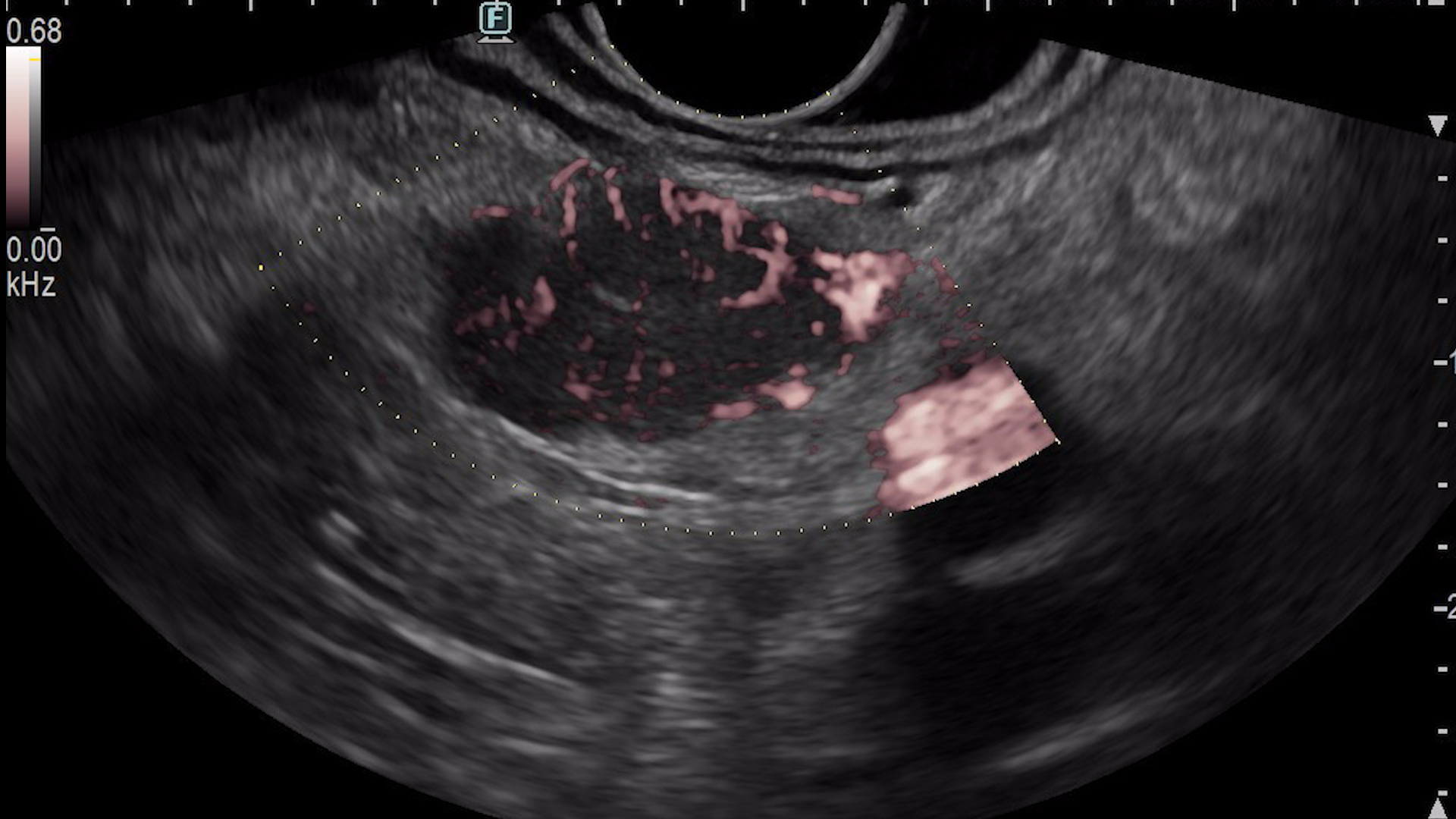
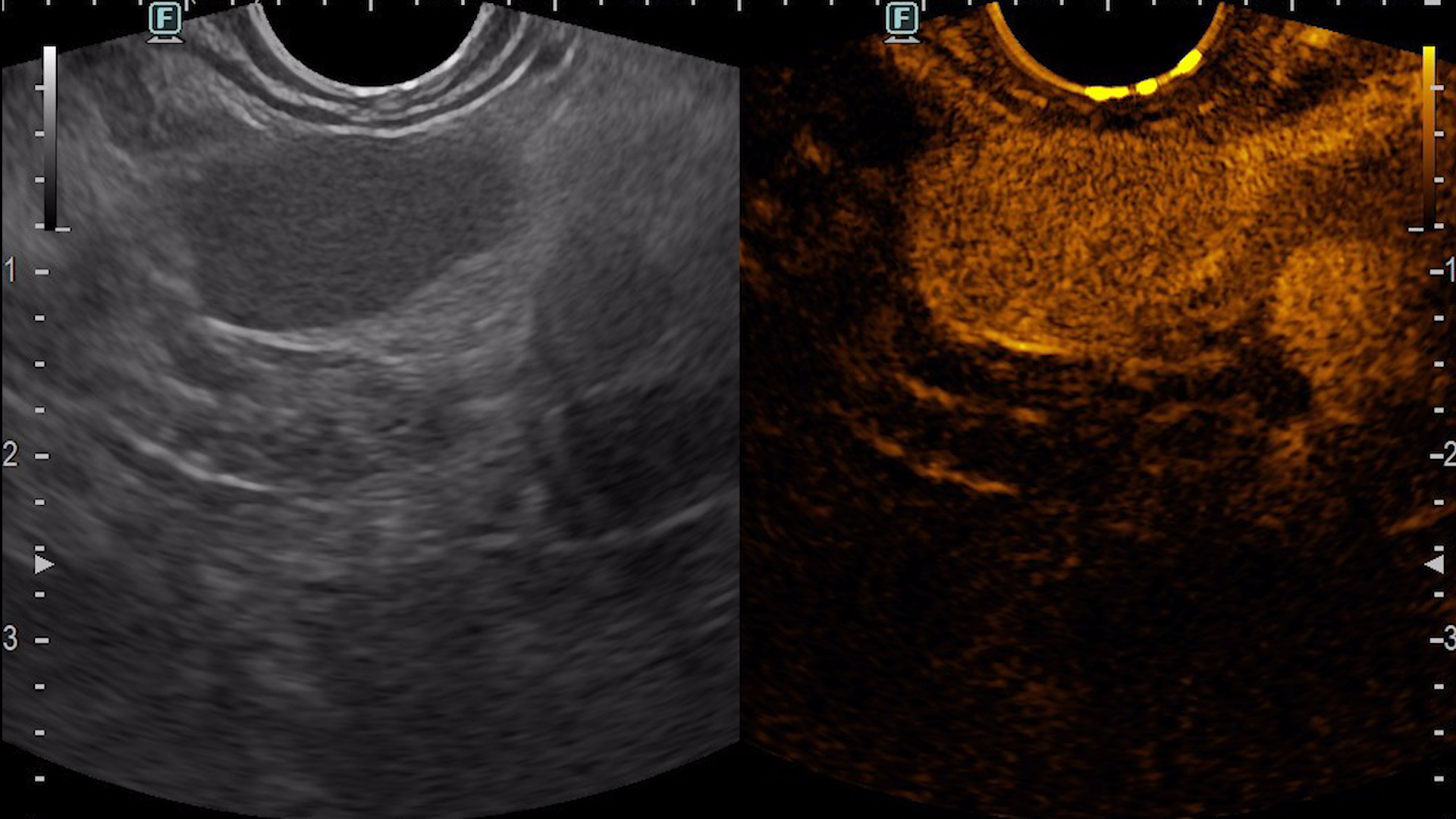
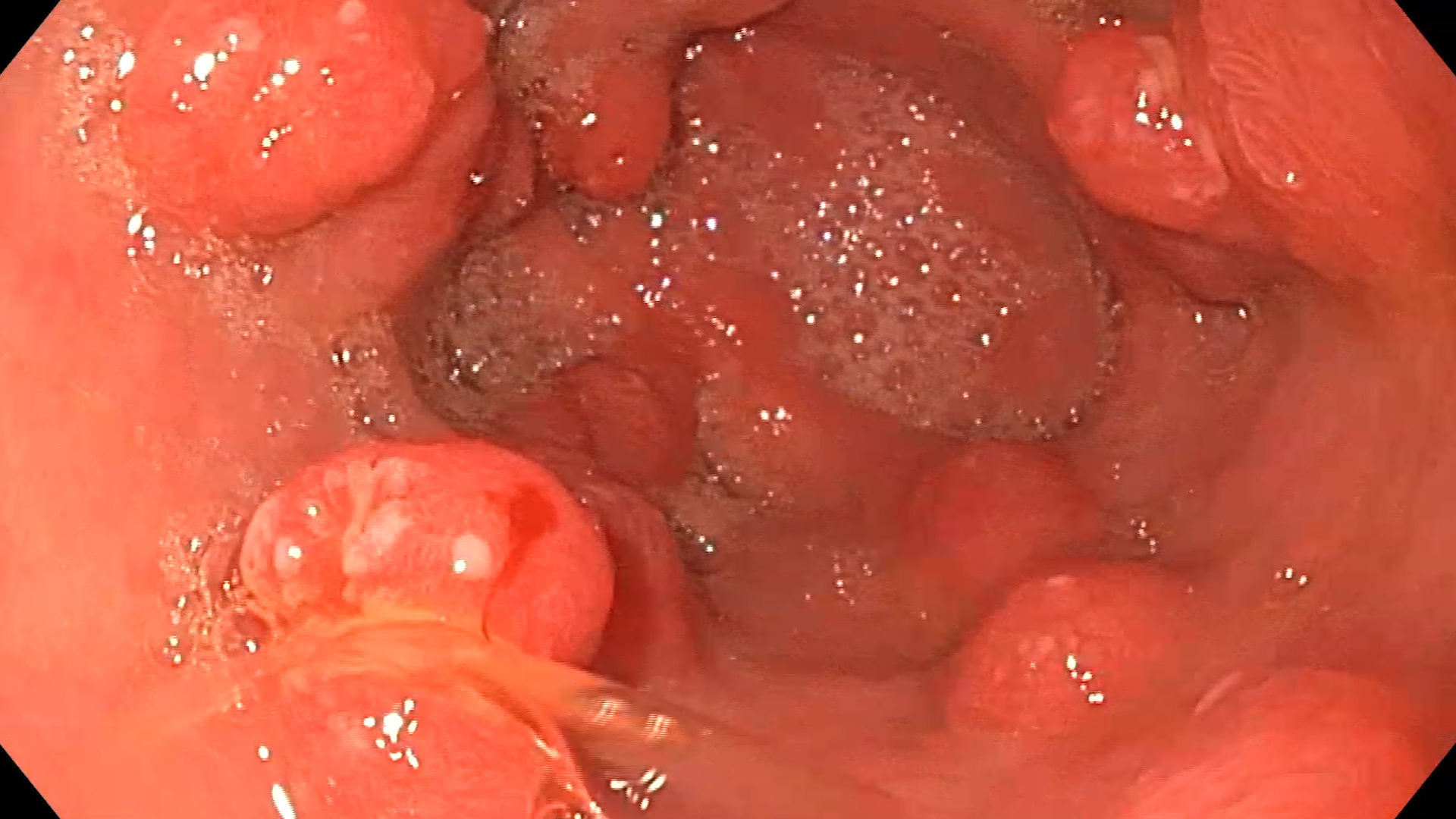
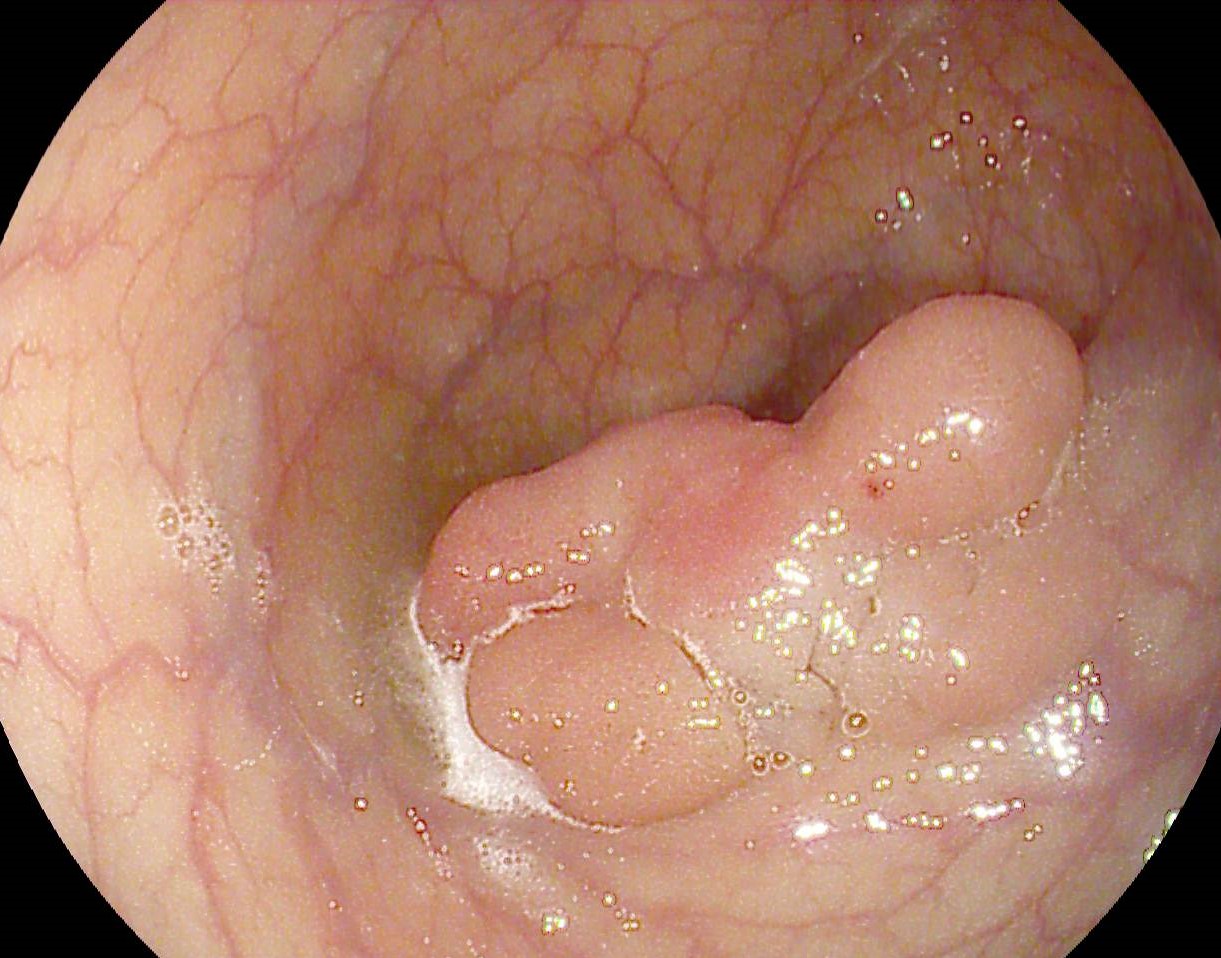
Consequently, an endoscopic ultrasound examination was carried out with tissue acquisition from the mass using a 22G Franssen-type needle (Acquire, Boston Scientific). The tumor was hypervascular on both color Doppler (Fig. 3a), detective flow imaging (Fig. 3b) and contrast-enhanced harmonic imaging (CHI) endoscopic ultrasound (Fig. 4). Histopathology was conclusive for a well-differentiated G1 neuroendocrine tumor, while immunohistochemistry confirmed the diagnosis, showing a Ki 67 index of 1%.
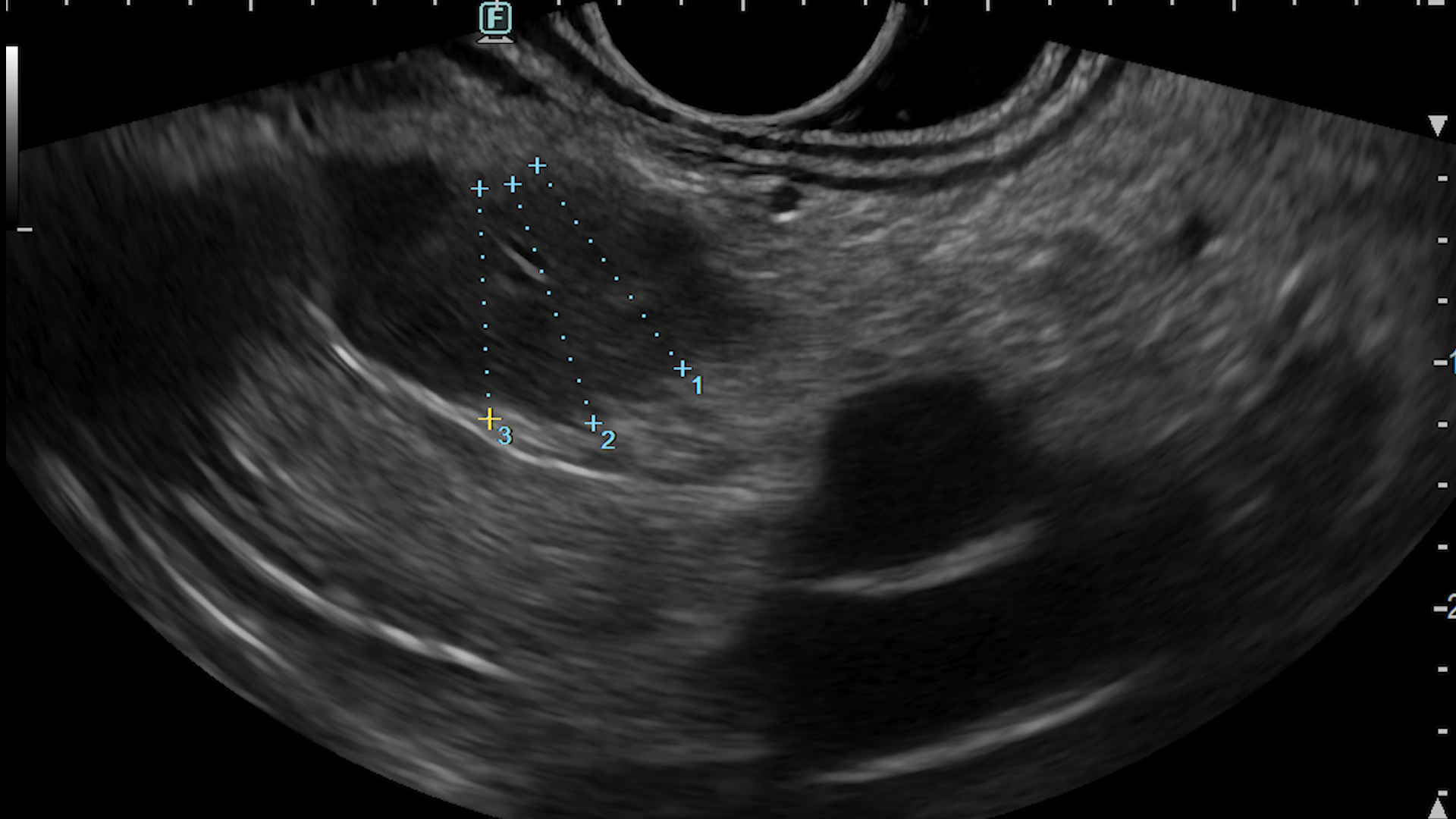
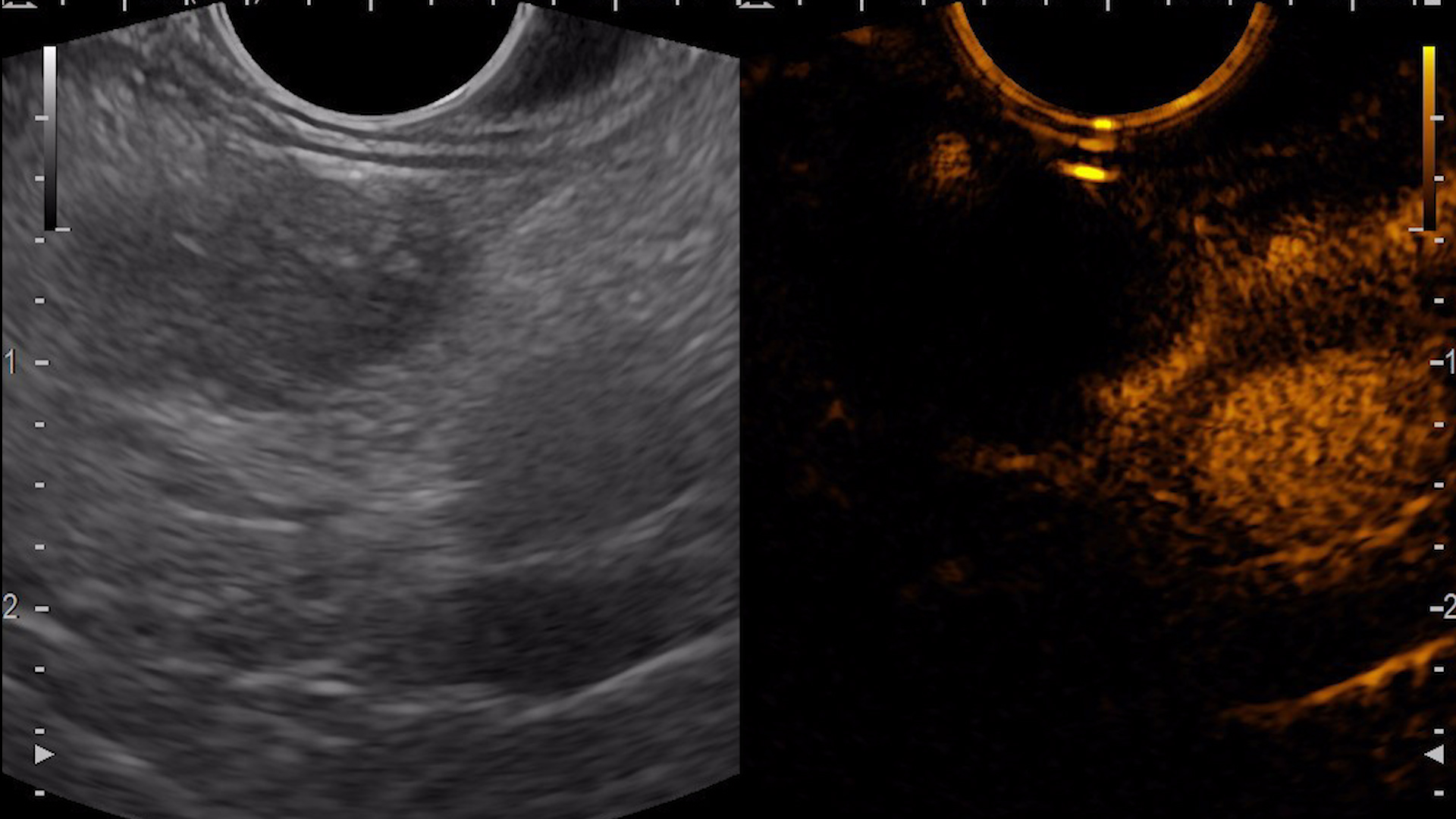
EUS-guided radiofrequency ablation was planned for treatment of the lesion (Fig. 5), using a 10 mm EUS-RFA catheter (Taewong). After probe insertion, the ablation cycle is started and a hyperechoic area of coagulative necrosis is seen over the RFA catheter (Fig. 6). The procedure was carried out in 3 passes, to fully ablate the lesion. Contrast-enhanced EUS, compared to pre-ablation hyperenhancement, revealed no uptake of contrast in the area of the pancreatic tumor (Fig. 7). The procedure was uneventful and the patient recovered very well and rapidly. Second day after the procedure, fasting glycemia rose to 82 mg/dL and in two weeks it reached 98 mg/dL.
Pancreatic insulinoma.
EUS-RFA is a promising technique for treatment of selected pancreatic neoplasms. In a propensity-matched, multicenter study which compared EUS-RFA to surgery, the EUS approach proved high efficacy with fewer complications and shorter hospitalization than surgery. While surgery was associated with no relapse rate, EUS-RFA can require retreatment in several sessions.
- Crinò SF, et al. Clin Gastroenterol Hepatol. 2023; 21(11): 2834-2843. e2. doi:10.1016/j.cgh.2023.02.022