See other cases
EUS-guided hepaticogastrostomy for a perihilar colangiocarcinoma
A 72-year-old patient, with unremarkable medical history, presented to the clinic with jaundice that has developed over the preceding 3 weeks and has been progressively worsening, with no associated complaints.
The patient presented with an ECOG score of 2, being overweight and afebrile. Physical examination revealed intensely icteric skin and sclera without abdominal pain. However, the patient reported colic stools and hyperchromic urine.
Laboratory findings indicated significant cholestasis with a total bilirubin level of 37 mg/dl, of which the direct fraction accounted for 34 mg/dl. Additionally, liver enzyme levels were elevated, with GGT at 1754 U/L, FAL at 733 U/L, GOT at 265 U/L, and GPT at 390 U/L. The CA 19-9 marker was notably elevated, exceeding 10,000 IU/ml, while no inflammatory syndrome was observed.
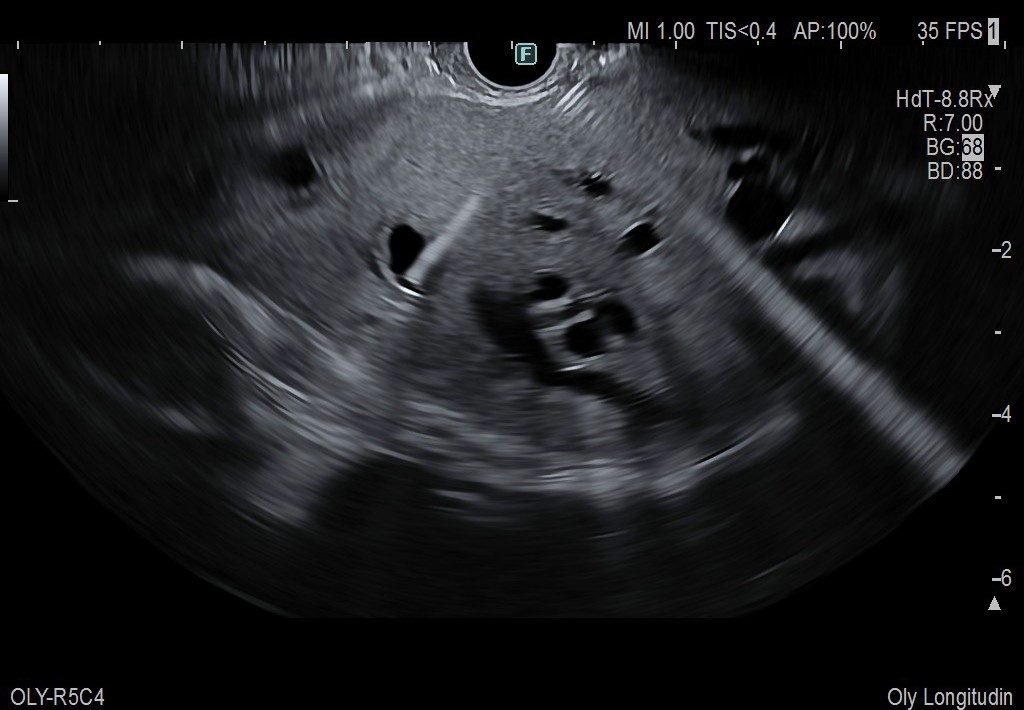
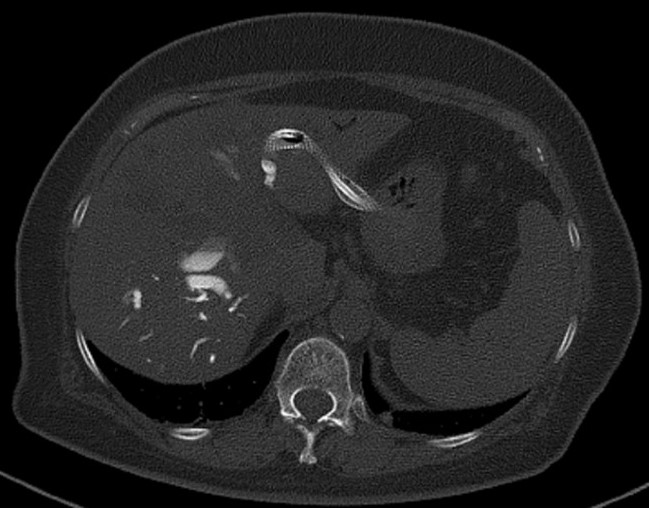
Contrast-enhanced CT confirmed the presence of an expansive lesion at the hepatic hilum (Fig. 1), involving the biliary junction and extending to both left and right hepatic ducts. The lesion measured 50/25/52 mm and exhibited characteristics indicative of a Klatskin type IV Bismuth-Corlette tumor. Furthermore, significant intrahepatic bile duct dilatation was evident in both liver lobes. Confirmation of the diagnosis was obtained through endoscopic ultrasound with fine needle aspiration (FNA) using a 22G needle, which histologically identified a poorly differentiated G3 perihilar cholangiocarcinoma.
After convening the multidisciplinary team and assessing the patient’s condition urgent measures were deemed necessary to facilitate prompt initiation of chemotherapy. Following thorough discussion and obtaining the patient’s consent, the decision was made to perform a endoscopic ultrasound guided hepatic-gastric-anastomosis (EUS-HGS), followed by endoscopic retrograde cholangio-pancreatography (ERCP) to alleviate the obstruction in the right lobe of the liver.
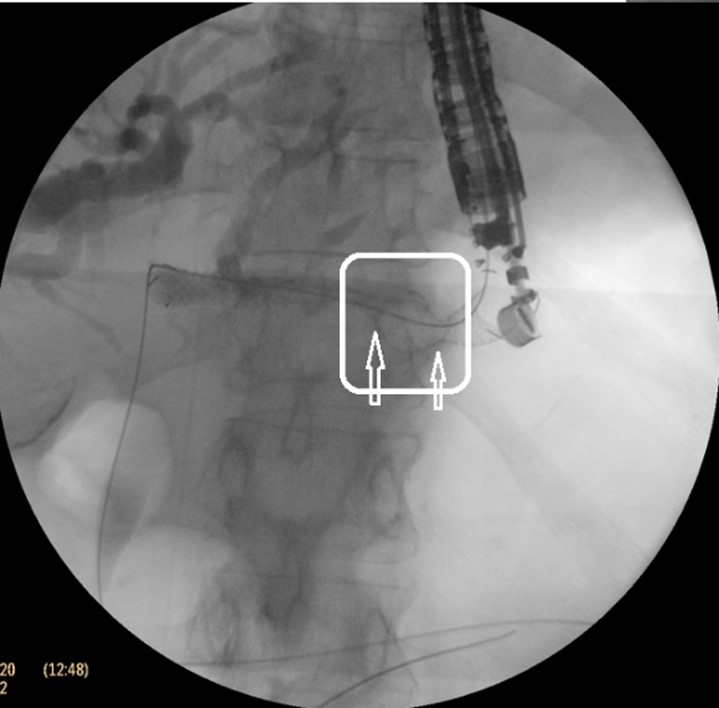
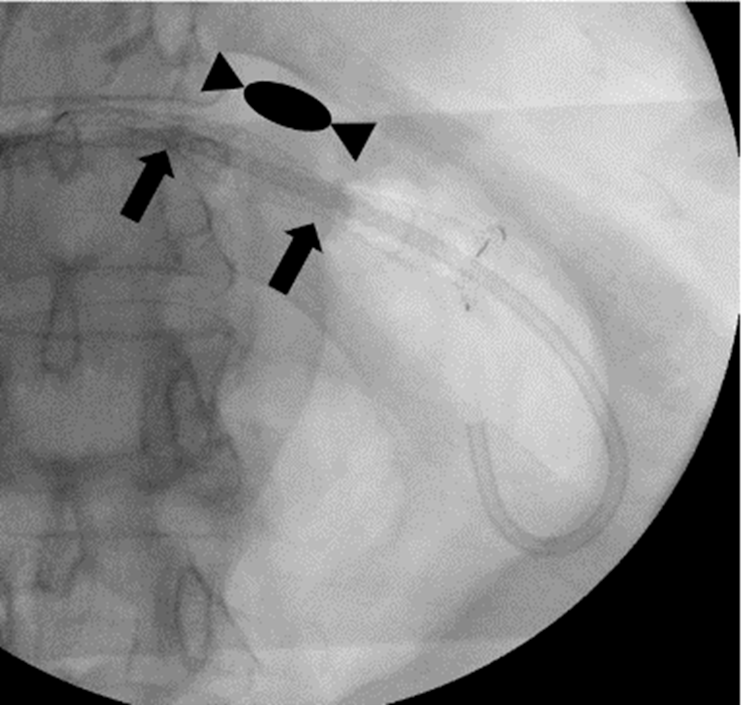
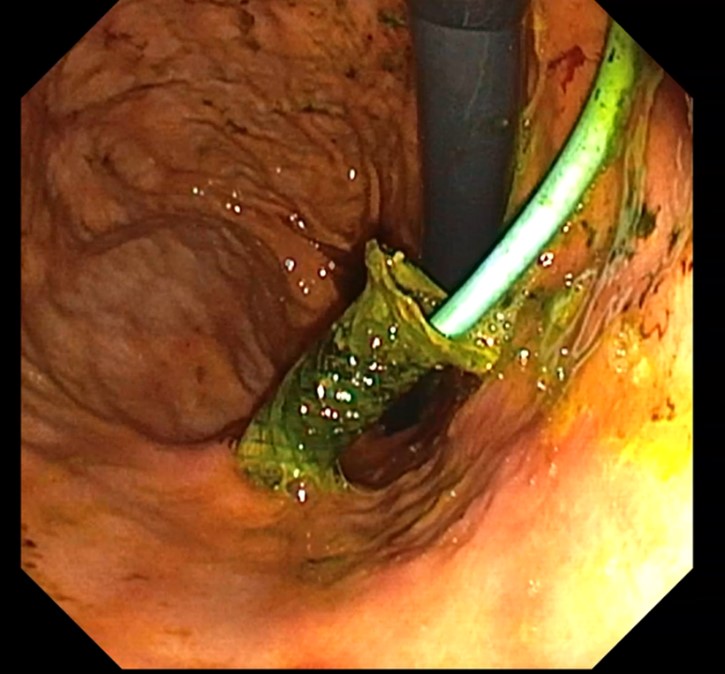
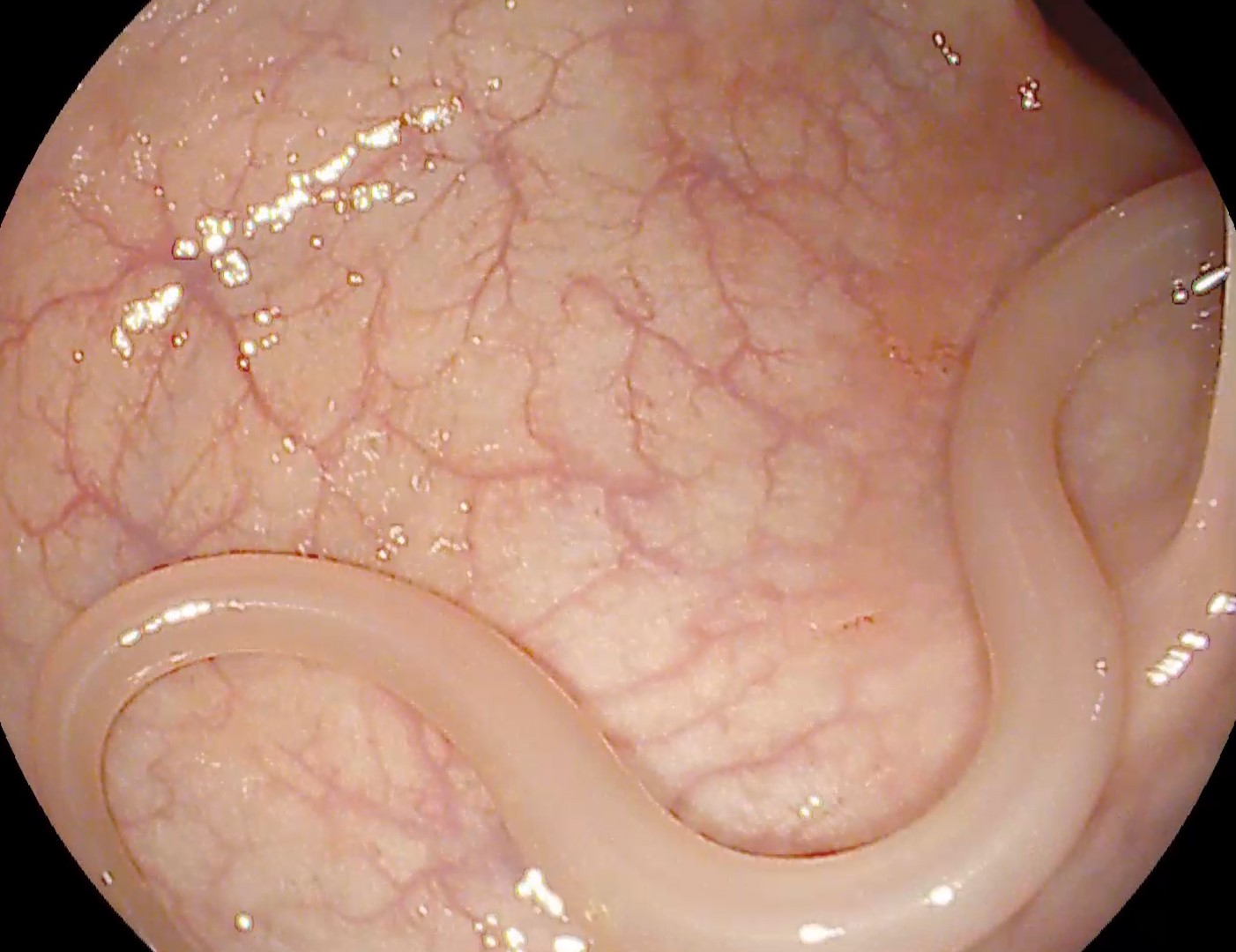
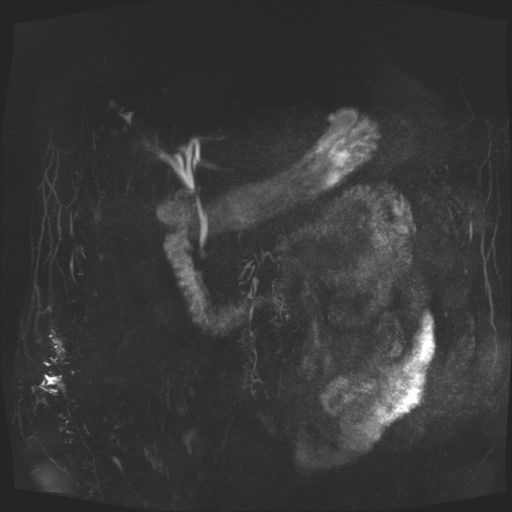
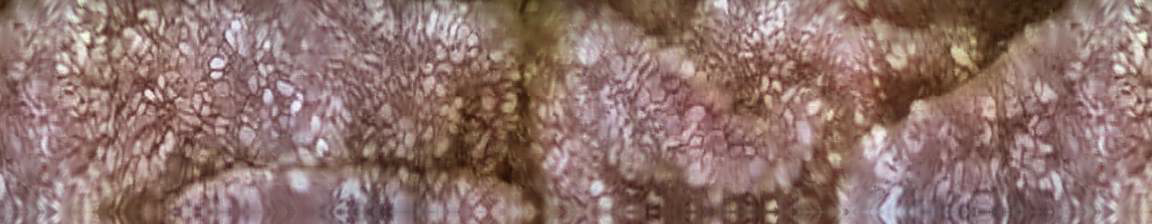
With the patient positioned supine, orotracheally intubated and mechanically ventilated, a linear echoendoscope was utilized to perform the procedure. Through transgastric approach, a dilated biliary branch in the III hepatic segment was identified and punctured using a 19 G FNA needle. Subsequently, a cholangiogram was performed (Fig. 2a,b). A 0.035-inch guidewire was then advanced beyond the stenosis into the duodenum (Fig. 2c), followed by creation of the fistulous tract using a 6F cystotome (Fig. 2d). A GIOBOR-type 10/100 mm metal stent was inserted, with its proximal uncovered end into the bile ducts and its distal end, equipped with a flange, positioned in the stomach. Fluoroscopic imaging revealed two narrowings in the stent separated by an intermediate bulge, known as the “candy sign” (Fig. 3). Additionally, a 10-Fr x 100 mm double pigtail stent was placed within the metallic prosthesis to prevent dislocation and migration (Fig. 4a,b).
Subsequently, ERCP was performed to place a plastic biliary stent in the right bile duct, using a 8.5 Fr x 120 mm stent (Fig. 5).
A follow-up CT scan performed at 24 hours post-procedure confirmed the correct positioning of both transgastric stents without any local complications (Fig. 6).
The patient’s clinical course was uneventful, with no early or late adverse events observed. Notably, there was significant clinical and biological improvement, evidenced by a reduction in cholestasis and gradual resolution of the jaundice. Consequently, the patient was discharged and scheduled for chemotherapy.
Obstructive jaundice due to Klatskin Bismuth-Corlette IV tumor. Biliary drainage by EUS-HGS and ERCP.
Hilar stenoses pose a significant challenge for endoscopists due to their complex nature, requiring the placement of multiple stents and carrying a high risk of complications such as angiocholitis, pancreatitis, and stent occlusion. Percutaneous biliary drainage (PTBD) has historically been the preferred option in these cases.
While PTBD boasts a high success rate, its major drawback lies in the impact on quality of life and the discomfort, pain and associated complications (biliary peritonitis, displacement of the drain tube and angiocholitis) caused by the presence of an external drain tube. Endoscopic drainage via ERCP offers the distinct advantage of avoiding these drawbacks and the potential to restore anatomical biliodigestive communication. However, certain situations necessitate the expertise of an experienced endoscopist.
Bilateral insertion of plastic or metal stents presents technical challenges, requiring the insertion of a guidewire into the intrahepatic bile ducts followed by sequential stent placement. Inserting the second or third stent after the initial stent introduction proves challenging in a bile duct narrowed by tumor stenosis. This challenge can be mitigated by employing stents with smaller diameters, albeit at the expense of reduced permeability rates.
Endoscopic ultrasound guided biliary drainage (BD), such as EUS-HGS, serves as a valuable alternative to surgery, ERCP and percutaneous transhepatic BD in the management of obstructive jaundice. The procedure offers several advantages over conventional approaches, including the avoidance of local complications associated with ERCP, such as pancreatitis, tumor ingrowth and stent occlusion. Furthermore, EUS-HGS is associated with a lower rate of re-intervention compared to ERCP. Given the specific characteristics of our case, namely a Bismuth-Corlette IV tumor with limited communication between the right and left liver lobes, EUS-HGS was deemed the most suitable approach.
Nevertheless, the procedure is not without limitations, which may include the presence of large amounts of ascites, liver metastases in the left lobe and the necessity of a qualified and experienced operator. Such skilled professionals may not be readily available in many medical centers, further complicating the feasibility of the procedure.
The presented case highlights the substantial impact of EUS-HGS on the overall outcome of patients with malignant biliary obstruction secondary to hilar tumors. Serving as a valid alternative strategy for biliary drainage, EUS-HGS not only effectively alleviates obstructive jaundice but also facilitates the early initiation of chemotherapy. This emphasizes the importance of EUS-HGS in optimizing patient care by enabling quick symptom relief and facilitating the implementation of essential oncological treatments.
- Schoch, Armelle1; Lisotti, Andrea1,2; Walter, Thomas3; Fumex, Fabien1; Leblanc, Sarah1; Artru, Pascal1; Desramé, Jérôme1; Brighi, Nicole4; Marsot, Julien5; Souquet, Jean-Christophe6; Napoléon, Bertrand1,. Efficacy of EUS-guided hepaticogastrostomy in prolonging survival of patients with perihilar cholangiocarcinoma. Endoscopic Ultrasound 11(6):p 487-494, Nov–Dec 2022. | DOI: 10.4103/EUS-D-22-00014
- Giovannini, Marc1,. EUS-guided hepaticogastrostomy. Endoscopic Ultrasound 8(Suppl 1):p S35-S39, November 2019. | DOI: 10.4103/eus.eus_47_19
- van der Merwe SW, van Wanrooij RLJ, Bronswijk M, Everett S, Lakhtakia S, Rimbas M, Hucl T, Kunda R, Badaoui A, Law R, Arcidiacono PG, Larghi A, Giovannini M, Khashab MA, Binmoeller KF, Barthet M, Perez-Miranda M, van Hooft JE. Therapeutic endoscopic ultrasound: European Society of Gastrointestinal Endoscopy (ESGE) Guideline. Endoscopy. 2022 Feb;54(2):185-205. | DOI: 10.1055/a-1717-1391.
- Feldman, E. J., Friedman, L. S., & Brandt, L. J. (2015). Sleisenger and Fordtran’s gastrointestinal and liver disease (Issue 1, p. 1). http://lib.tums.ac.ir/site/catalogue/8070
- Paik WH, Park DH. Outcomes and limitations: EUS-guided hepaticogastrostomy. Endosc Ultrasound. 2019 Nov 28;8(Suppl 1):S44-S49. | DOI: 10.4103/eus.eus_51_19.