See other cases
Esophageal perforation after foreign body ingestion
A 72-year-old patient with a known history of multiple cardiac comorbidities and chronic kidney disease presents to the Emergency Room for retrosteral pain 4 days after the accidental ingestion of a foreign body (pill package).
Clinical: altered general status, hemodinamically stable, without crepitations in the neck area or superior thorax, no spontaneous or palpatory abdominal pain.
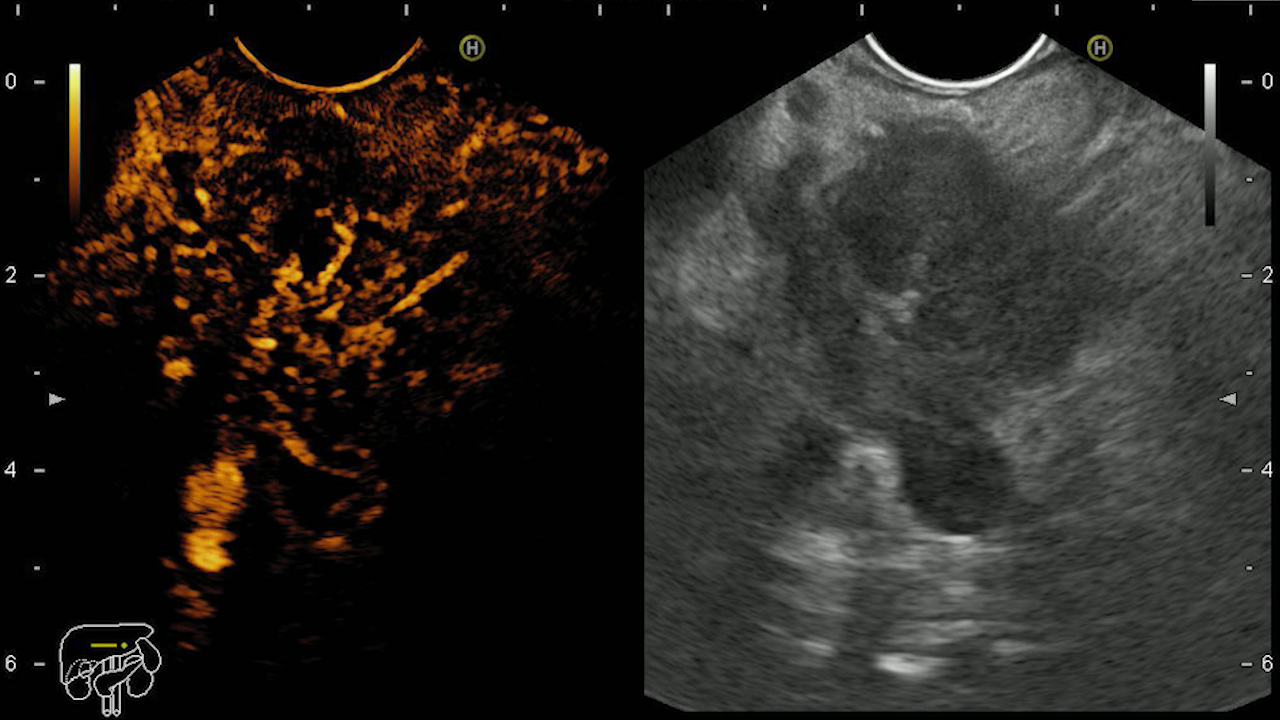
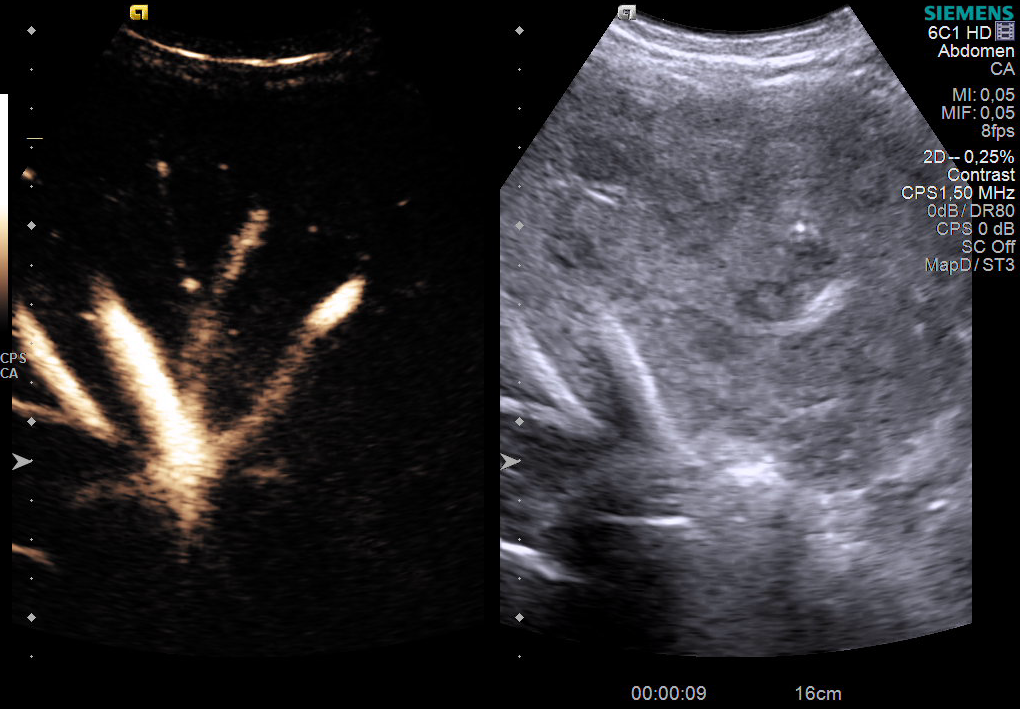
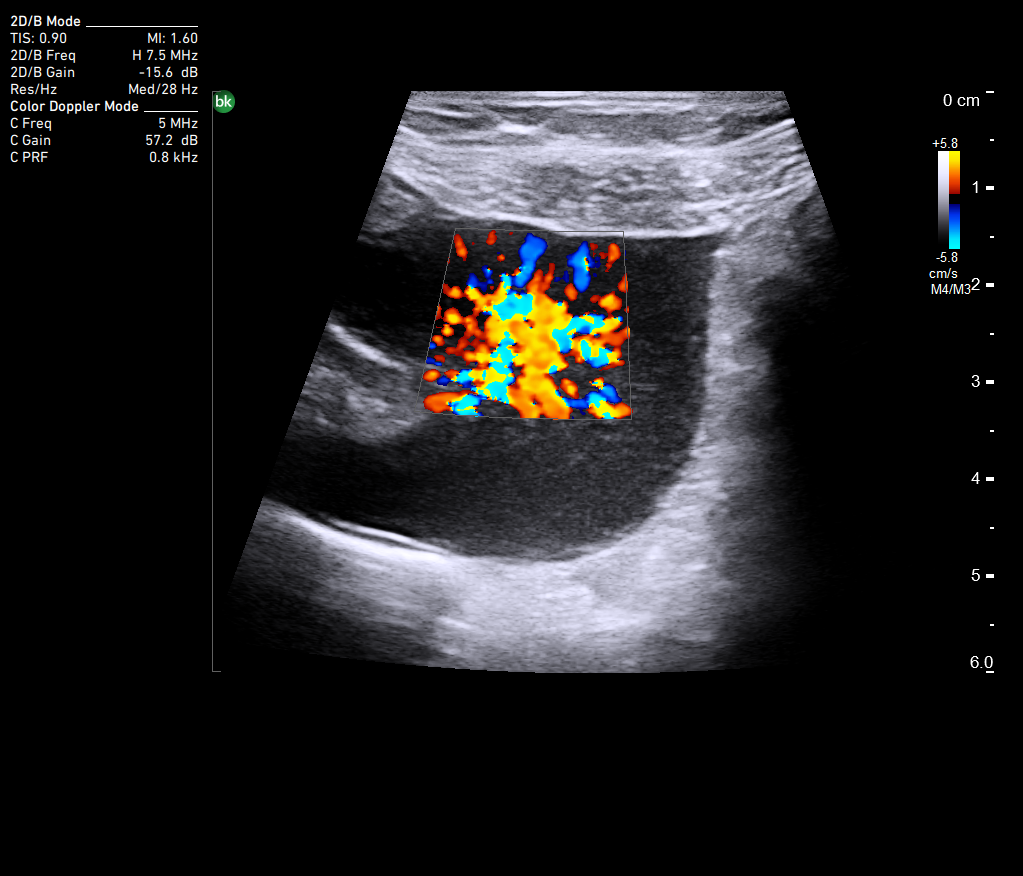
Thorax+abdomen CT without contrast: Minimal right-sided pneumothorax, global cardiomegaly, minimal bilateral pleural effusion; in the distal esophagus – area with mixed densities of 7.9/3.1 cm containing slightly spontaneous hiperdense structure measuring 1.9 cm that may correspond to a foreign body; the area described seems to communicate with an inhomogenous zone with aerial component localised on the projection area of the right pleural space, measuring 4.6/2.3 cm, raising the suspicion of a right-sided eso-pleural fistula.
The patient is admitted in the Thoracic Surgery Department where a right pleural drain is placed. She is administered orally a solution of methylene blue that passes in the pleural drainage tube, thus confirming the existence of a eso-pleural fistula.
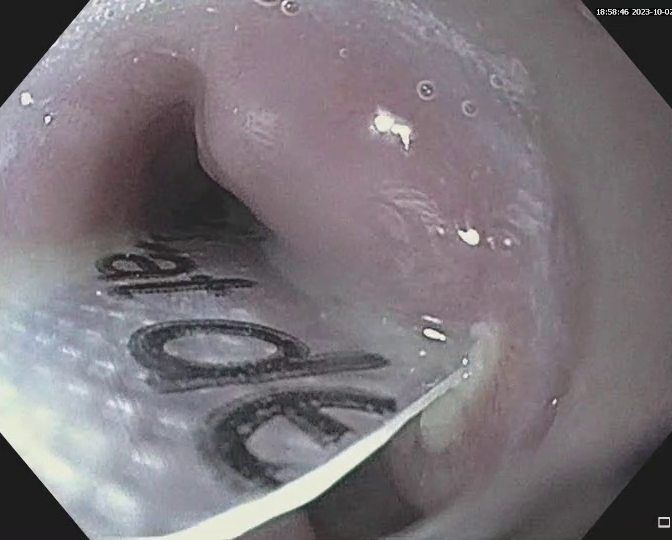
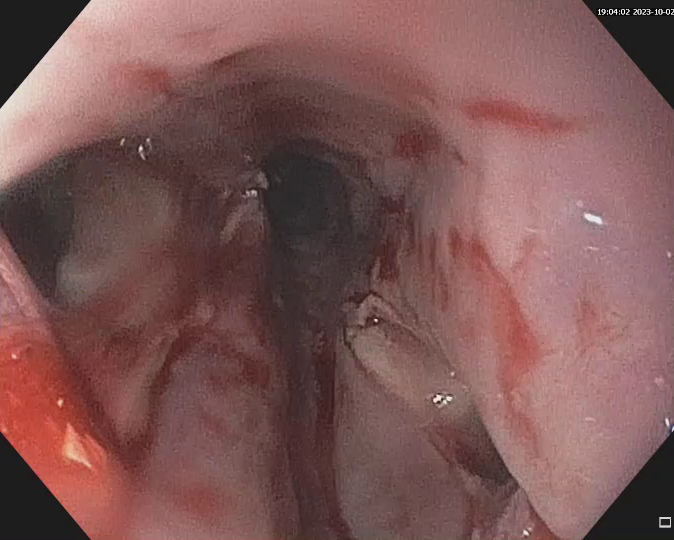
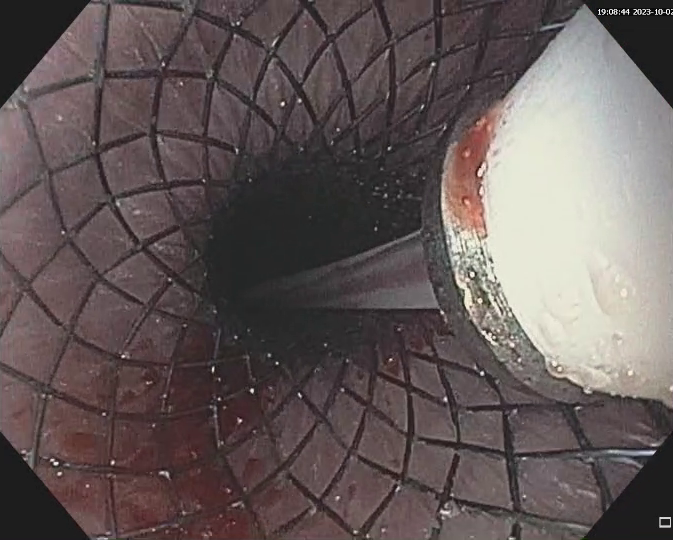
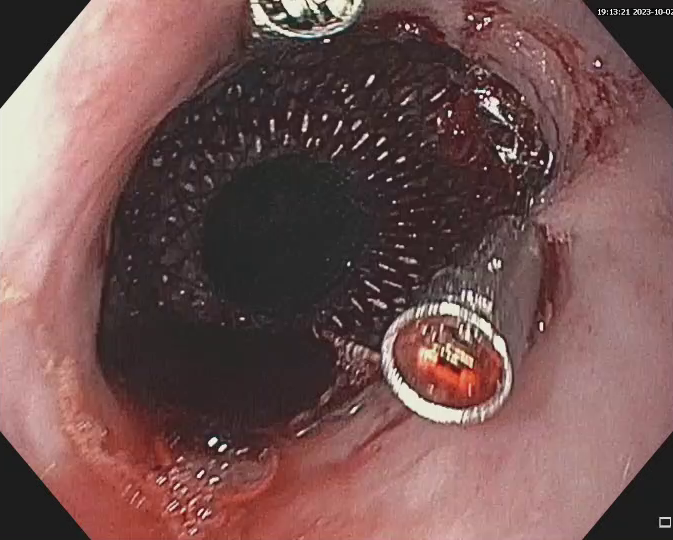
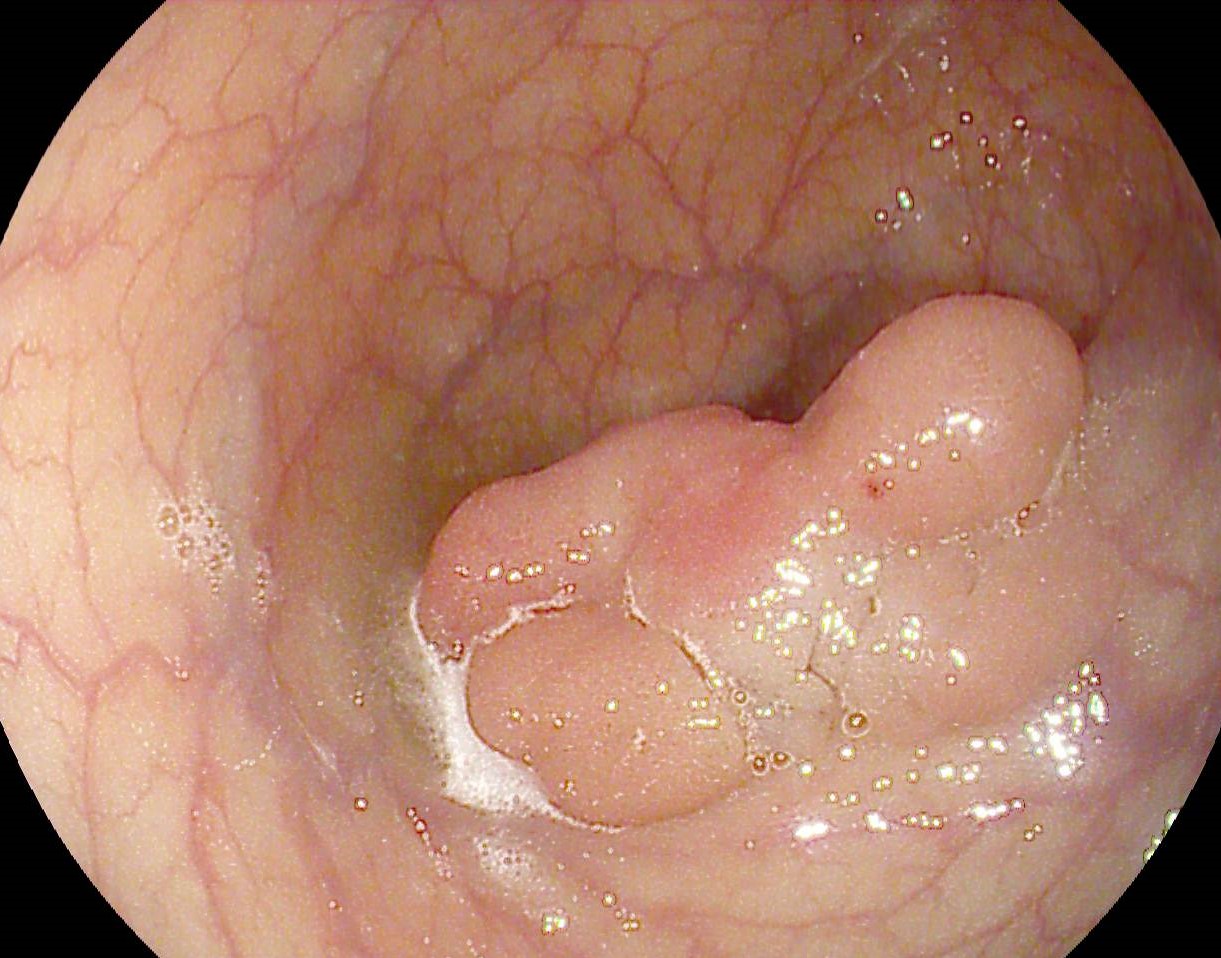
Upper GI endoscopy: In the middle segment of the esophagus the foreign body is identified (pill package), being impacted in two opposite walls. Two perforations are also seen at both the described contact points. The foreign body is extracted with an alligator forceps, after mounting a plastic cap on the endoscope tip for protection. The esophagus is reintubated and the two perforations are seen, measuring 8 and 10 mm respectively. A 120 x 20 mm fully covered metal stent is placed under direct vision and anchored at the proximal part with two 16 mm repositionable clips.
Esophageal foreign body – endoscopic removal. Double esophageal perforation. Fully covered metal stent placement. Right eso-pleural fistula.
Esophageal foreign bodies may be alimentary (fragments of meat, chicken or fish bones) or non-alimentary in origin, the latter category comprising a large variety of objects. Esophageal foreign body impaction is an endoscopic emergency (especially if the foreign body is sharp) because of the risk of perforation that rises as time passes.
Guidelines recommend emergency upper GI endoscopy, ideally in 2 hours and maximum in 6 hours after presentation in the case of an impacted sharp esophageal foreign body. For sharp foreign bodies, a device that protects the esophagus is advisable, in order to avoid producing additional lesions. This can either be an overtube or a plastic cap. Endotracheal intubation may be necessary in cases with high risk of aspiration – uncooperative patient, proximal esophageal location of the foreign body. Esophageal perforation is the most dreaded complication of foreign bodies, being associated with high mortality. It may be treated endoscopically, the optimum method depending on location and size. Small perforations, measuring less than 2 cm, can be closed using repositionable or over-the-scope clips and larger ones can be treated by placing fully-covered metal stents or vacuum therapy. Simultaneously, the patient may benefit from placing an endoscopic percutaneous gastrostomy that allows feeding. Placing a stent in a patient with no esophageal stenosis is associated with a high risk of migration (up to 25%) so anchoring the prosthesis with TTS or OTS clips is desirable. If collections are present in the mediastinum or elsewhere, they should be surgically drained. The optimal duration the stent should be maintained is not standardized, varying between 4 and 8 weeks, after which the prosthesis is removed by endoscopy.
Fully-covered esophageal metal stents can successfully be used in esophageal perforations of various causes. Due to migration risk, it is advisable that stents are anchored with TTS or OTS clips.
- Spaander MCW, van der Bogt RD, Baron TH, et al. Esophageal stenting for benign and malignant disease: European Society of Gastrointestinal Endoscopy (ESGE) Guideline – Update 2021. Endoscopy. 2021;53(7):751-762
- Birk M, Bauerfeind P, Deprez PH, et al. Removal of foreign bodies in the upper gastrointestinal tract in adults: European Society of Gastrointestinal Endoscopy (ESGE) Clinical Guideline. Endoscopy. 2016;48(5):489-496
- ASGE Standards of Practice Committee, Ikenberry SO, Jue TL, et al. Management of ingested foreign bodies and food impactions. Gastrointest Endosc. 2011;73(6):1085-1091.
- Chirica, M., Kelly, M.D., Siboni, S. et al.Esophageal emergencies: WSES guidelines. World J Emerg Surg. 2019; 14, 26