See other cases
Endoscopic Ultrasound Management of Duodenal Stenosis in Groove Pancreatitis
A 75-year-old patient, smoker, chronic alcohol consumer, with dyslipidemia and peripheral arterial disease with a femoral stent, presenting as an emergency for persistent emetic syndrome that began approximately 6 months earlier, with worsening over the past 2 months, accompanied by inability to eat and abdominal pain.
Clinical: altered general condition, dehydrated, cachectic (BMI 18), hemodynamically and respiratory stable. Abdomen severely painful in the epigastric region, without signs of peritoneal irritation.
Biological: retention syndrome, lipase 4× the upper limit of normal, hemoconcentration with leukocytosis and neutrophilia.
Contrast-enhanced computed tomography (CT) revealed duodenal wall thickening up to 17 mm over a length of up to 5 cm adjacent to the pancreatic head, with mild upstream dilation and stasis, along with fat stranding and fine fluid streaks. The pancreatic head appeared slightly enlarged but with homogeneous contrast enhancement.
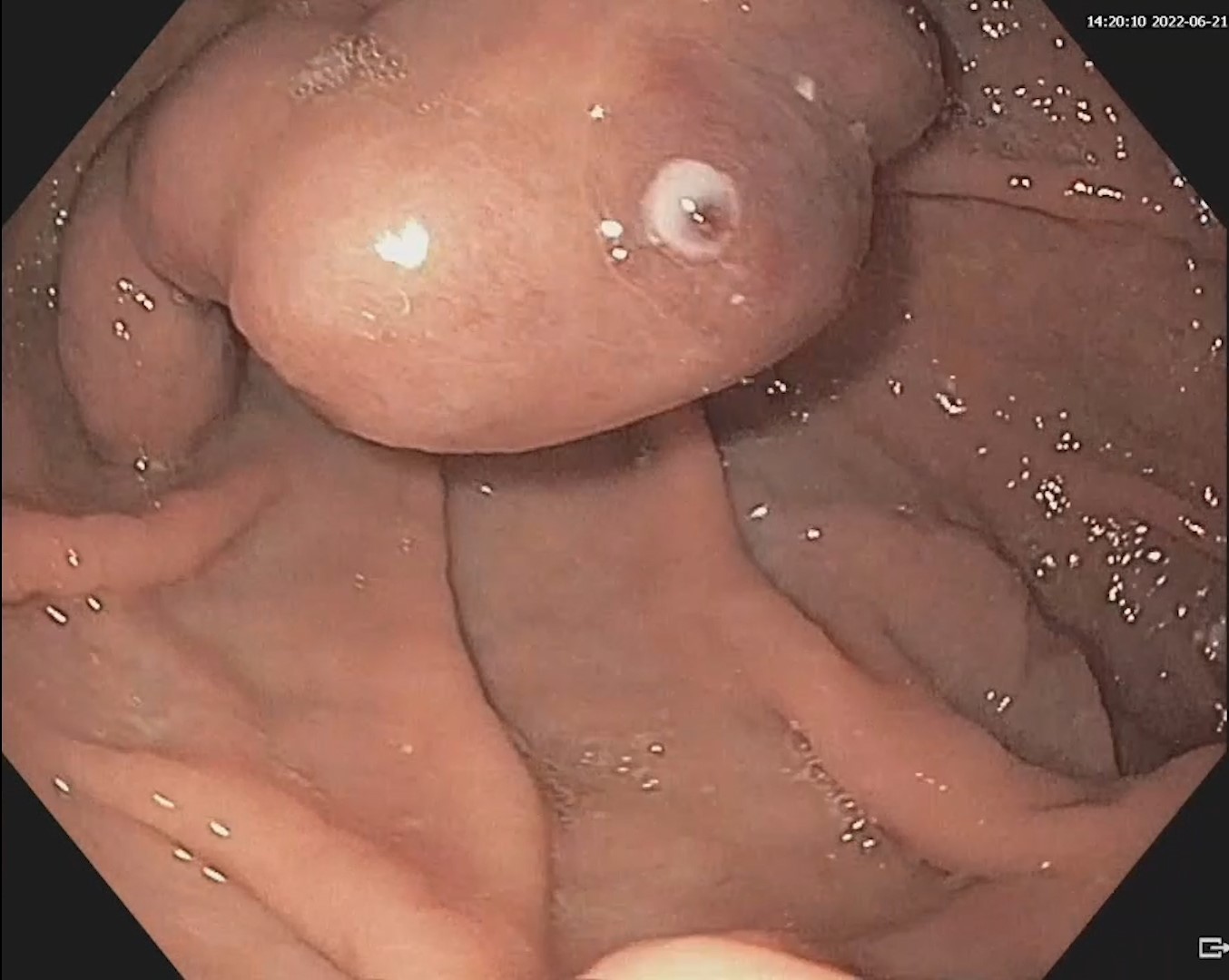
Further investigations included upper digestive endoscopy, which showed a severe stenosis that allowed passage of the endoscope with difficulty, without dysplastic features on macroscopic evaluation or NBI. Biopsies taken from this level were negative for malignancy.
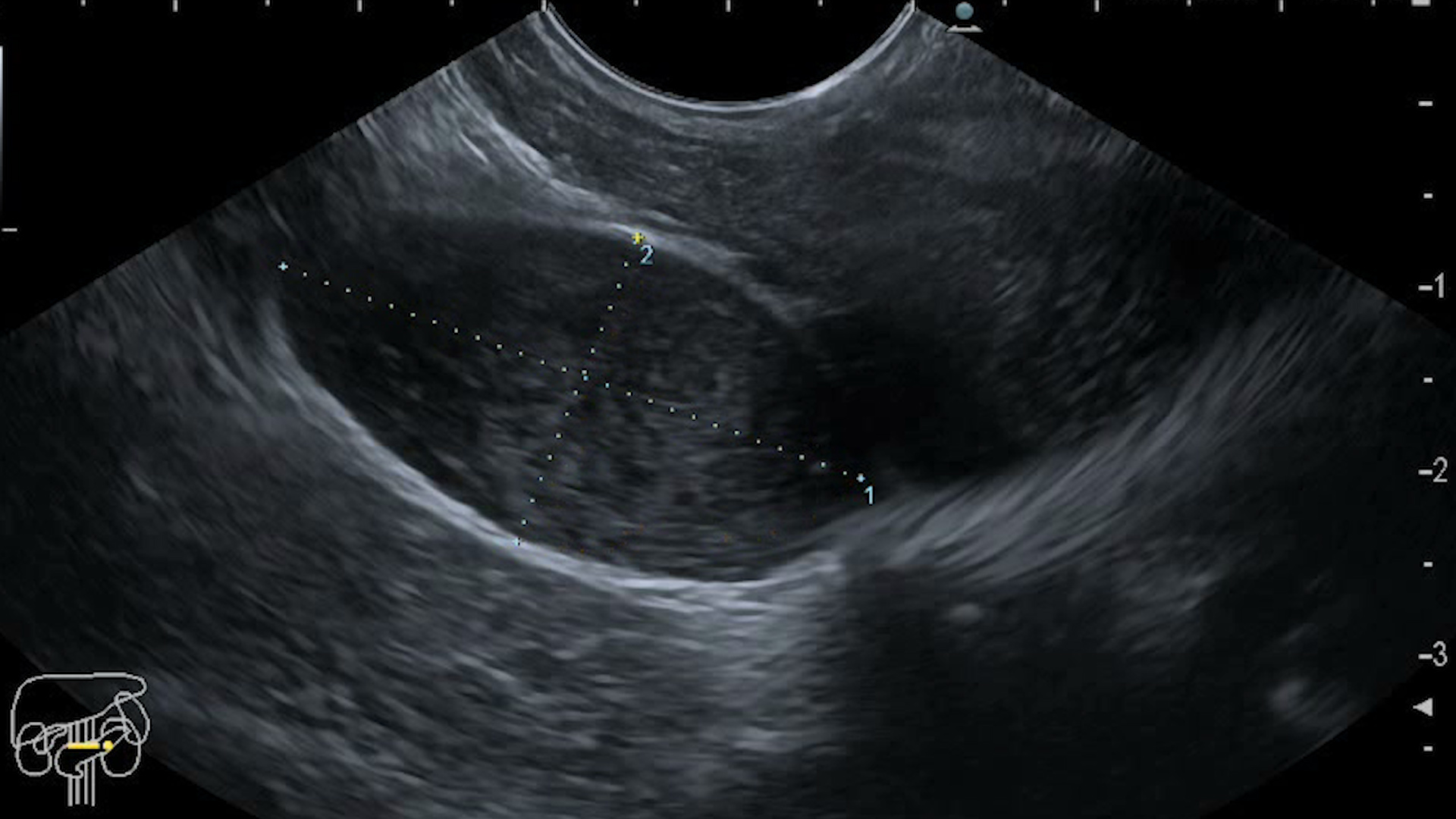
Endoscopic ultrasound of the pancreas showed criteria for chronic pancreatitis (Rosemont classification: 1 major and 3 minor criteria), with a thickened duodenal wall, heterogeneous echotexture, and a 5 mm cystic lesion within the wall (Fig. 1). Placement of a nasoenteral feeding tube was decided for nutritional support, and enteral feeding was well tolerated, with a weight gain of about 3 kg over 3 weeks.
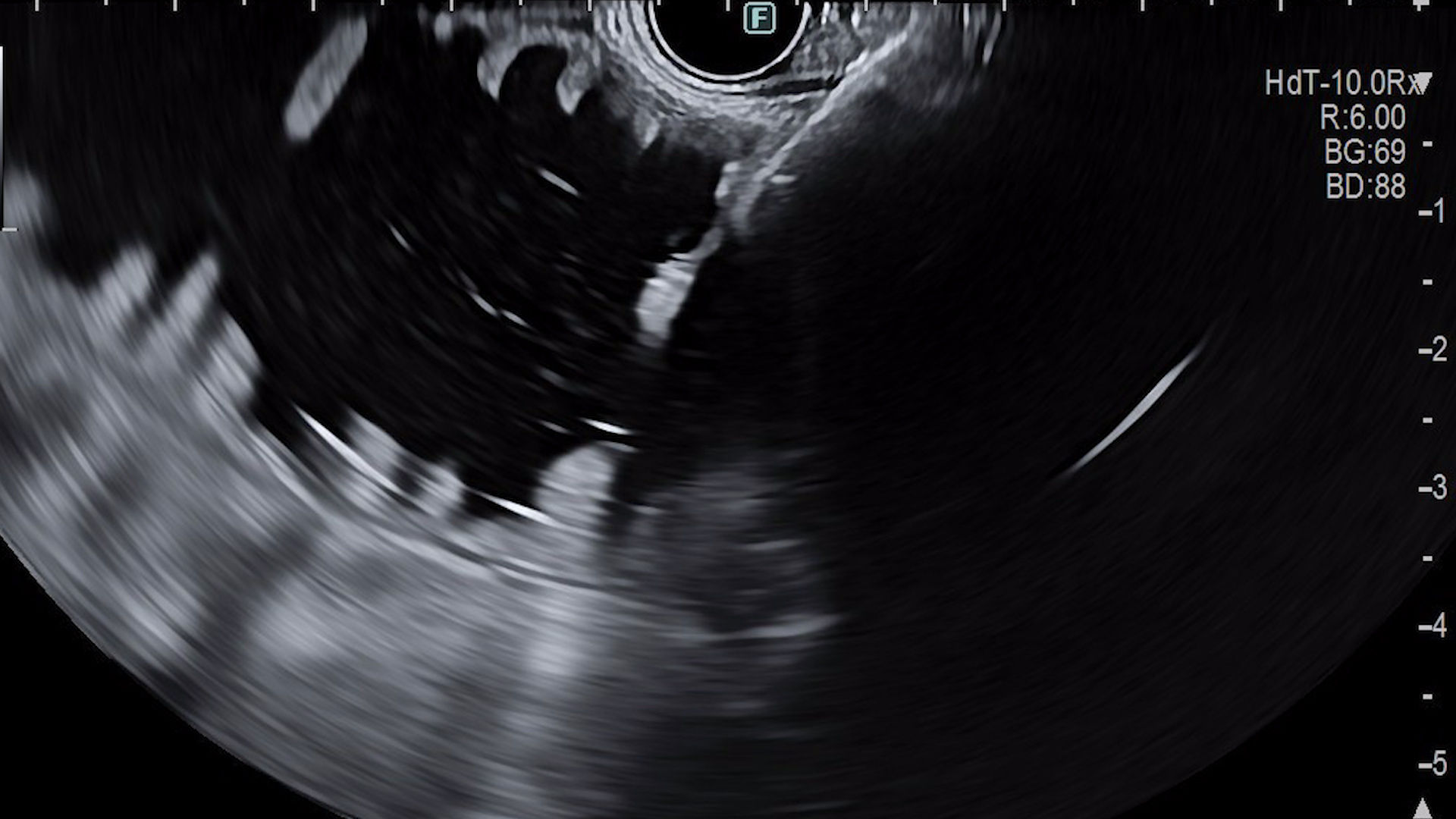
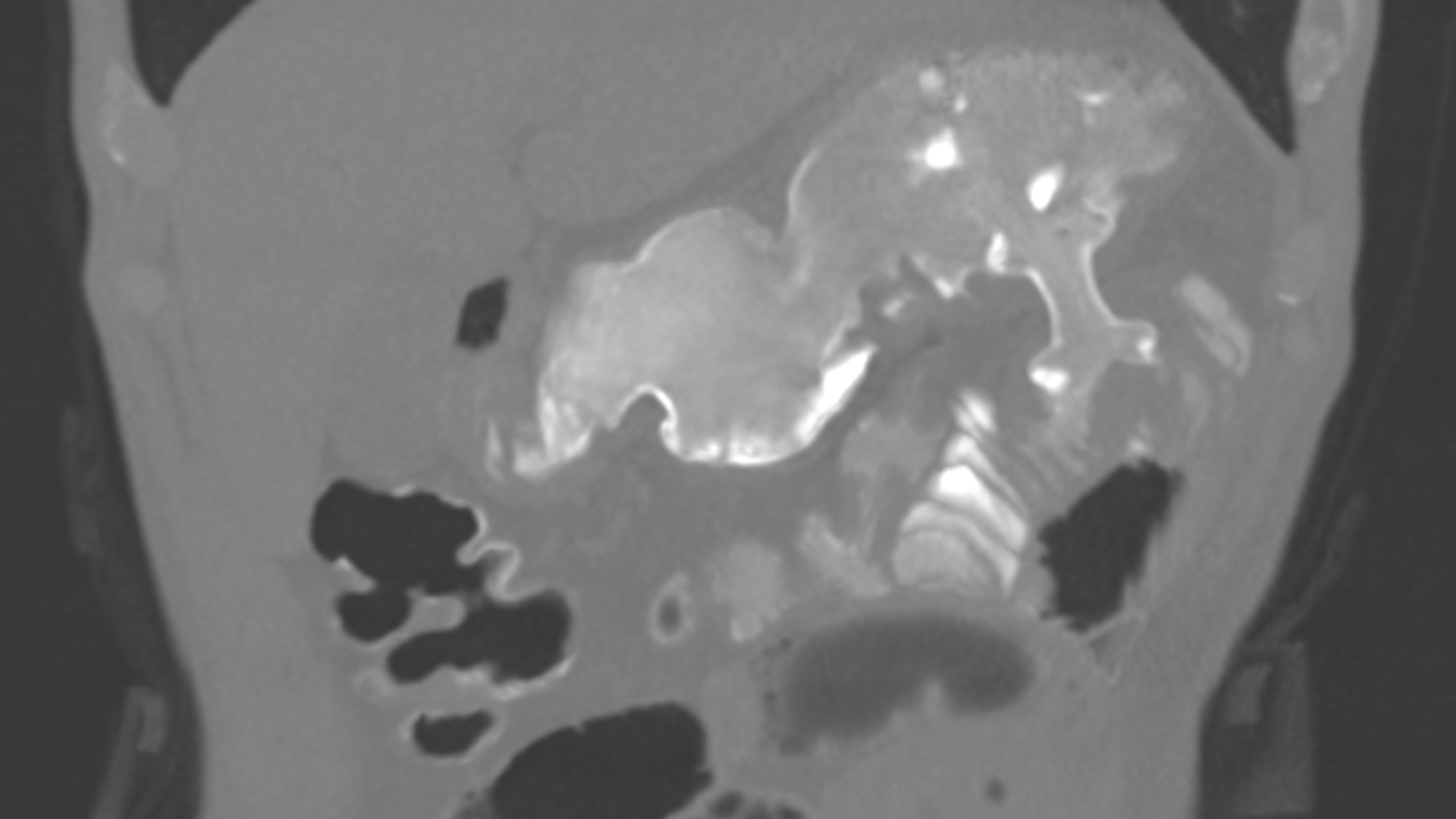
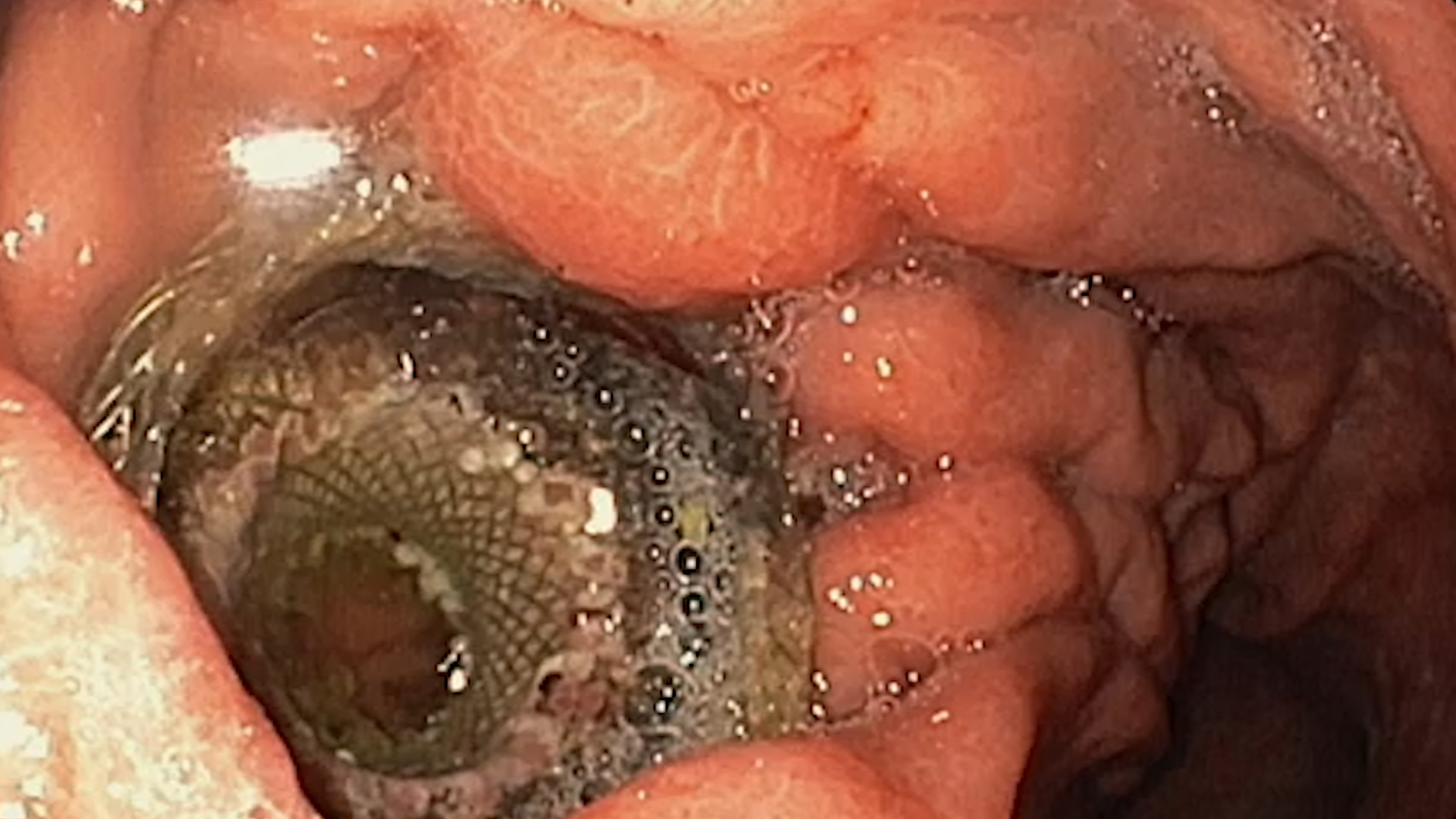
Taking into account the age, comorbidities and refusal of surgery, endoscopic ultrasound (EUS) gastrojejunostomy with a lumen apposing metal stent (LAMS) was then performed, under respiratory support. The nasoenteral tube technique was used, instilling approximately 400 mL of saline mixed with methylene blue into the enteral loop for distension. After removing the tube, a linear echoendoscope was introduced into the stomach to identify the dilated small bowel loop. After Doppler verification to avoid blood vessels, puncture was performed and a 20/10 mm LAMS (HotAxios, Boston Scientific) was deployed under EUS and fluoroscopic guidance (Fig. 2). After releasing the proximal flange, methylene blue-colored saline was visualized in the stomach. A barium transit study was performed to confirm patency (Fig. 3), showing favorable findings. CT examination with oral contrast was performed after 24h, showing a permeable gastrojejunostomy, without contrast extravasation (Fig 4).
The patient had a good evolution at 6 weeks post-placement, without subjective complaints, with weight gain, and with no endoscopic complications related to the stent (Fig. 5).
Groove pancreatitis complicated by duodenal stenosis. EUS guided gastrojejunostomy (EUS-GJ).
Gastric outlet obstruction reduces patients quality of life, limiting oral intake. Malnutrition and dehydration are the main causes of clinical and biological deterioration¹. EUS-GJ has become a recognized method due to its minimally invasive nature and its high technical and clinical success rates of 87–100% and 84–100%, respectively². Groove pancreatitis is a rare, debilitating disease, which usually necessitates major interventions like surgical pancreatico-duodenectomy (Whipple disease) or limited gastro-enterostomy laparoscopic interventions, if alimentary intolerance is on first plane.
Compared with surgical gastroenterostomy, EUS-GJ offers the advantages of reducing intra- and perioperative complications, especially in oncologic patients, as well as shortening hospital stay³. It may serve as an intermediate method prior to definitive surgical intervention or, in certain cases, as a long-term solution, with stent lifespan reported up to 1 year⁴.
EUS-guided GJ is a minimally invasive treatment option for duodenal stenosis due to malignant invasion but also due to benign conditions, especially in cases where surgery is contraindicated.
- Wannhoff, Andreas et al. Endoscopic ultrasound-guided gastroenterostomy for the treatment of gastric outlet obstruction secondary to acute pancreatitis. Endoscopy 2025; 57(3): 249-254. doi: 10.1055/a-2452-5307
- Tonozuka R, Tsuchiya T, Mukai S, et al. Endoscopic Ultrasonography-Guided Gastroenterostomy Techniques for Treatment of Malignant Gastric Outlet Obstruction. Clin Endosc 2020; 53(5): 510-518. doi: 10.5946/ce.2020.151
- Tyberg A, Perez-Miranda M, Sanchez-Ocaña R, et al. Endoscopic ultrasound-guided gastrojejunostomy with a lumen-apposing metal stent: a multicenter, international experience. Endosc Int Open 2016; 4: E276-E281. doi: 10.1055/s-0042-101789
- James TW, Greenberg S, Grimm IS, Baron TH. EUS-guided gastroenteric anastomosis as a bridge to definitive treatment in benign gastric outlet obstruction. Gastrointest Endosc 2020; 91: 537-542. doi: 10.1016/j.gie.2019.11.017