See other cases
Endoscopic ultrasound guided gastrojejunal anastomosis for benign gastric outlet obstruction
A 41-year-old patient, heavy drinker, diagnosed with chronic pancreatitis and multiple episodes of exacerbation who referred to the clinic for significant weight loss and postprandial vomiting.
Clinical – underweight, dehydrated patient, fierce abdominal pain mostly in the upper abdomen associated with multiple postprandial vomiting.
Biological – leukocytosis and dyselectrolytemia (hypochloremia); CEA, CA 19-9 within normal ranges.
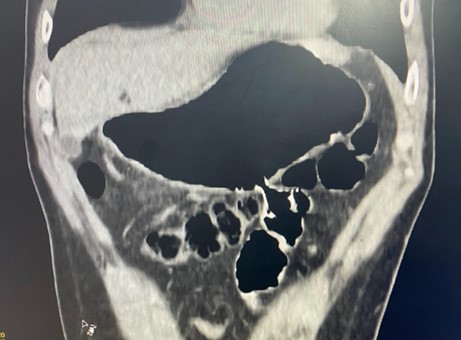
Contrast enhanced computer tomography (CECT) revealed chronic pancreatitis with important inflammatory changes and marked stenosing effect on the proximal duodenum, absence of passage of the oral contrast agent and secondary gastric stasis (Figure 1 a,b,c).
Gastric outlet obstruction secondary to acute pancreatitis.
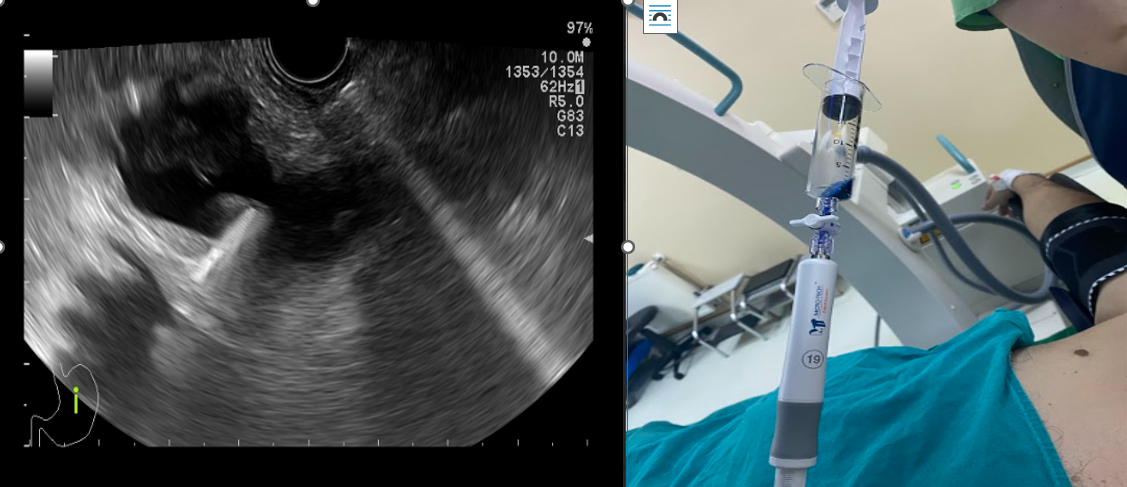
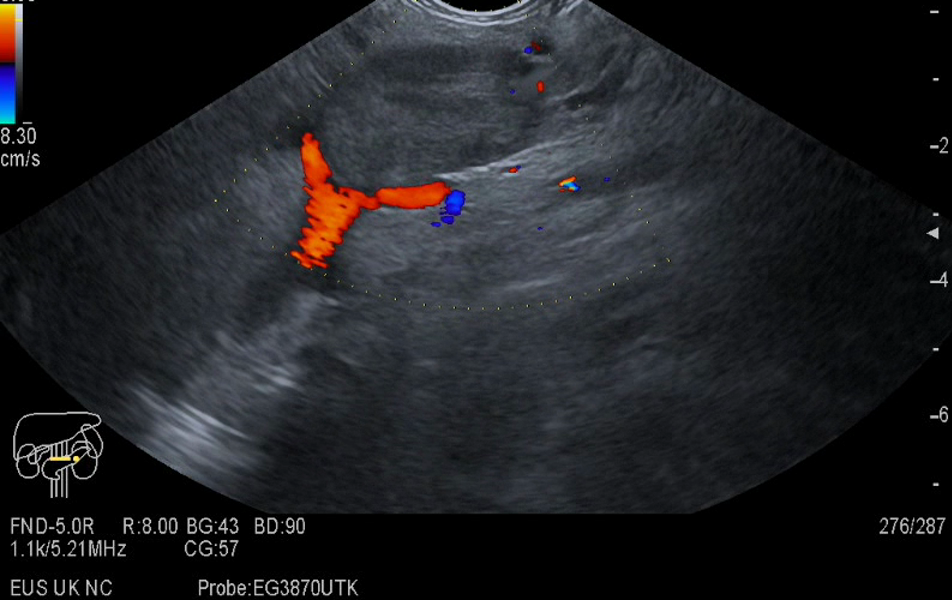
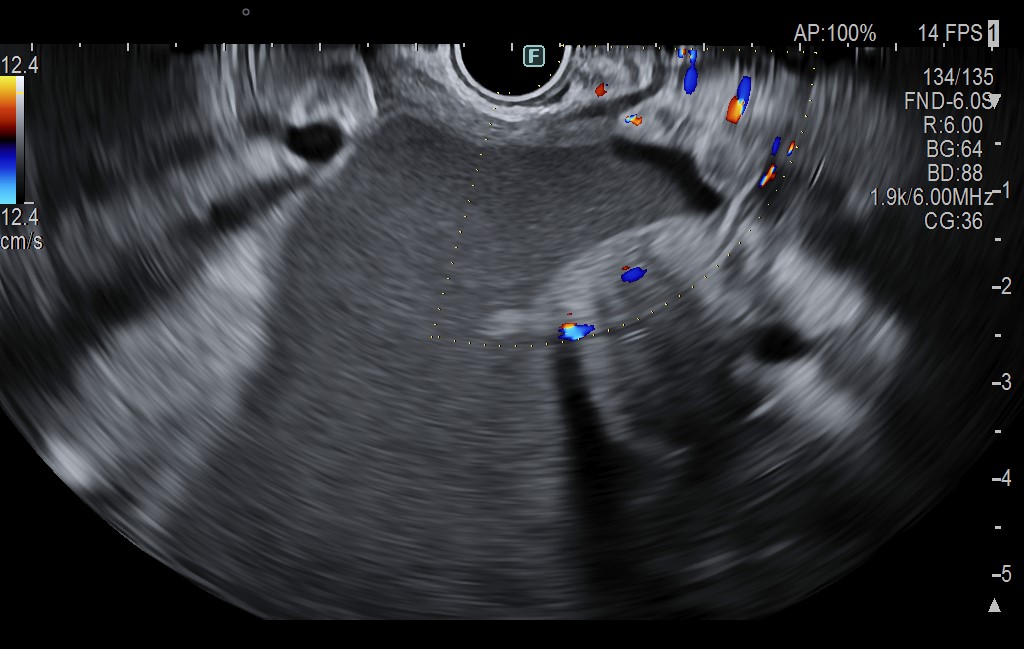
The patient refused surgery, therefore it was proposed for endoscopic ultrasound (EUS) guided gastrojejunal anastomosis. The technique was performed under endotracheal intubation and mechanical ventilation. The first step was to insert a nasocystic catheter beyond the stenosis and Treitz angle in the jejunum. Through it, at least 500 ml of saline mixed with methylene blue and contrast agent were continuously infused to achieve the necessary distension of jejunum and bring it close to the gastric wall. After EUS detection of a jejunal loop in contact with the stomach, a fine needle puncture was performed with methylene blue aspiration, confirming the right positioning (Figure 2 a,b). Subsequently, under EUS and fluoroscopic guidance one-step gastroenteral anastomosis was performed using a HotSpaxus (Taewoog Medical, South Korea) 16/20 mm lumen apposing metal stent (LAMS) with an electrocautery at the tip.
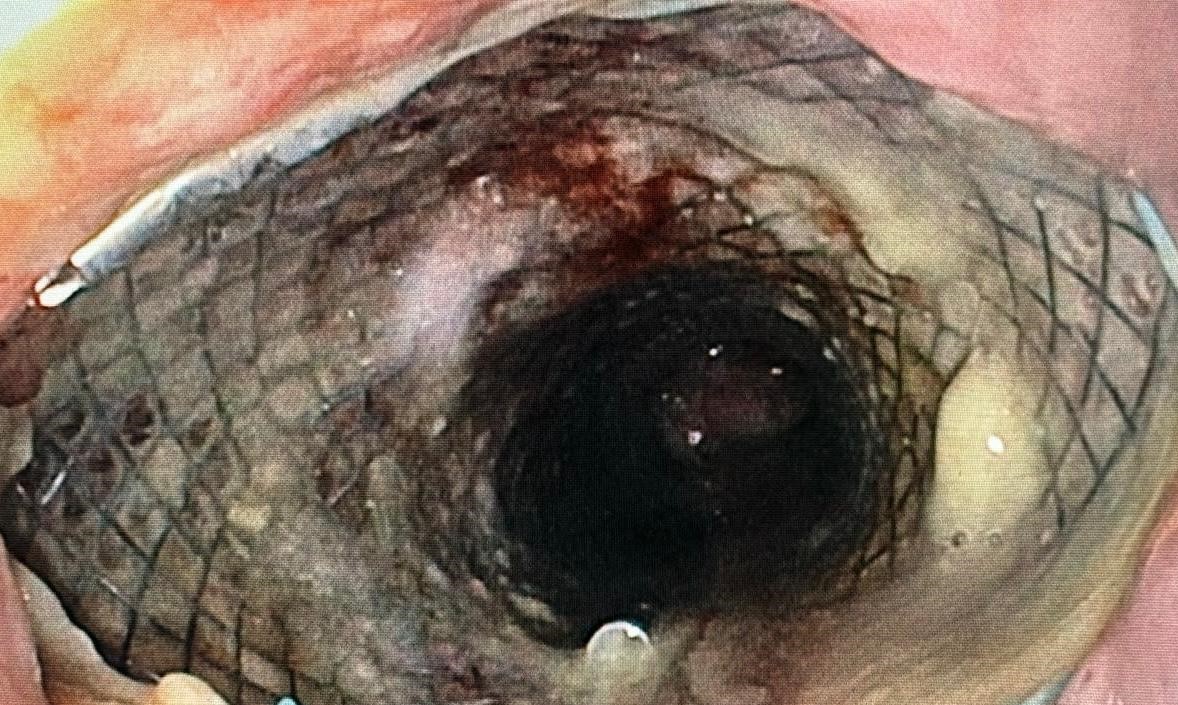
The correct stent position was confirmed by the absence of contrast agent leakage at fluoroscopic control (Figure 3). Abdominal CT exam described the right positioning of the stent without any immediate adverse events. The evolution was favourable, with the resumption of oral nutrition after few hours and discharge within 24 hours (Figure 4). One month after procedure, CT imaging described in situ stent, with complete expansion and optimal patency (Figure 5).
This is an uncommon form of manifestation of chronic pancreatitis, affecting the region between the pancreatic head and duodenum. It often appears in middle-aged men with a history of alcohol abuse.
Inflammatory digestive stenosis may have a favorable response to conservative treatment with antisecretory and anti-inflammatory medication, along with enteral nutrition on the nasojejunal tube and parenteral solutions. Moreover, the differential diagnosis of this pathology includes duodenal cancer, pancreatic neoplasm or invasive cholangiocarcinoma. Thus, exacerbation of chronic pancreatitis with duodenal obstruction could easily be underdiagnosed.
EUS-guided gastrojejunoanastomosis offers a minimally invasive and effective way for recovering the gastrointestinal pathway, representing a reliable alternative to duodenal stenting and surgery. The technique can be used either in benign or malignant gastric outlet obstruction.
- Chandan et al. EUS-guided gastroenterostomy versus enteral stenting for gastric outlet obstruction: Systematic review and meta-analysis, Endosc Int Open, 2021
- Pallisera-Lloveras A, Ramia-Ángel JM, Vicens-Arbona C, et al. Groove pancreatitis. Rev Esp Enferm Dig 2015;107:280–8.
- Balakrishnan V, Chatni S, Radhakrishnan L, et al. Groove pancreatitis: a case report and review of literature. JOP 2007;8:592–7.
- Li J, Liu Q, Liu Z, Cen C, Yang Y, Ye J, Xu L, Lu X, Chen D, Ruan W. Acute pancreatitis associated with duodenal obstruction induced by groove pancreatitis: A case report. Medicine (Baltimore).