See other cases
Endoscopic management of anastomotic biliary stenosis/stricture post orthotopic liver transplant
Known patient with orthotopic liver transplant, performed for HCV liver cirrhosis approximately 12 months prior, presents to the clinic for yellow coloring of the mucosa and skin, generalized itching and malaise.
Clinical: jaundice, painful in the right hypochondrium
Biological: total bilirubin 3,2 mg/dl, direct bilirubin 2,7 mg/dl, gammaGT 800 U/l, ALP 900 U/l, ALT 260 U/l, AST 230 U/l, CRP 78 mg/l
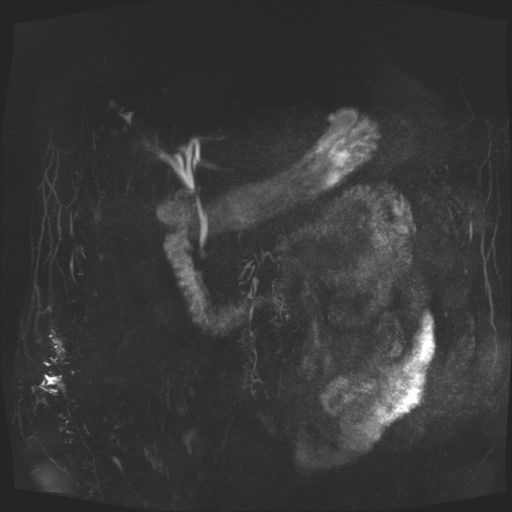
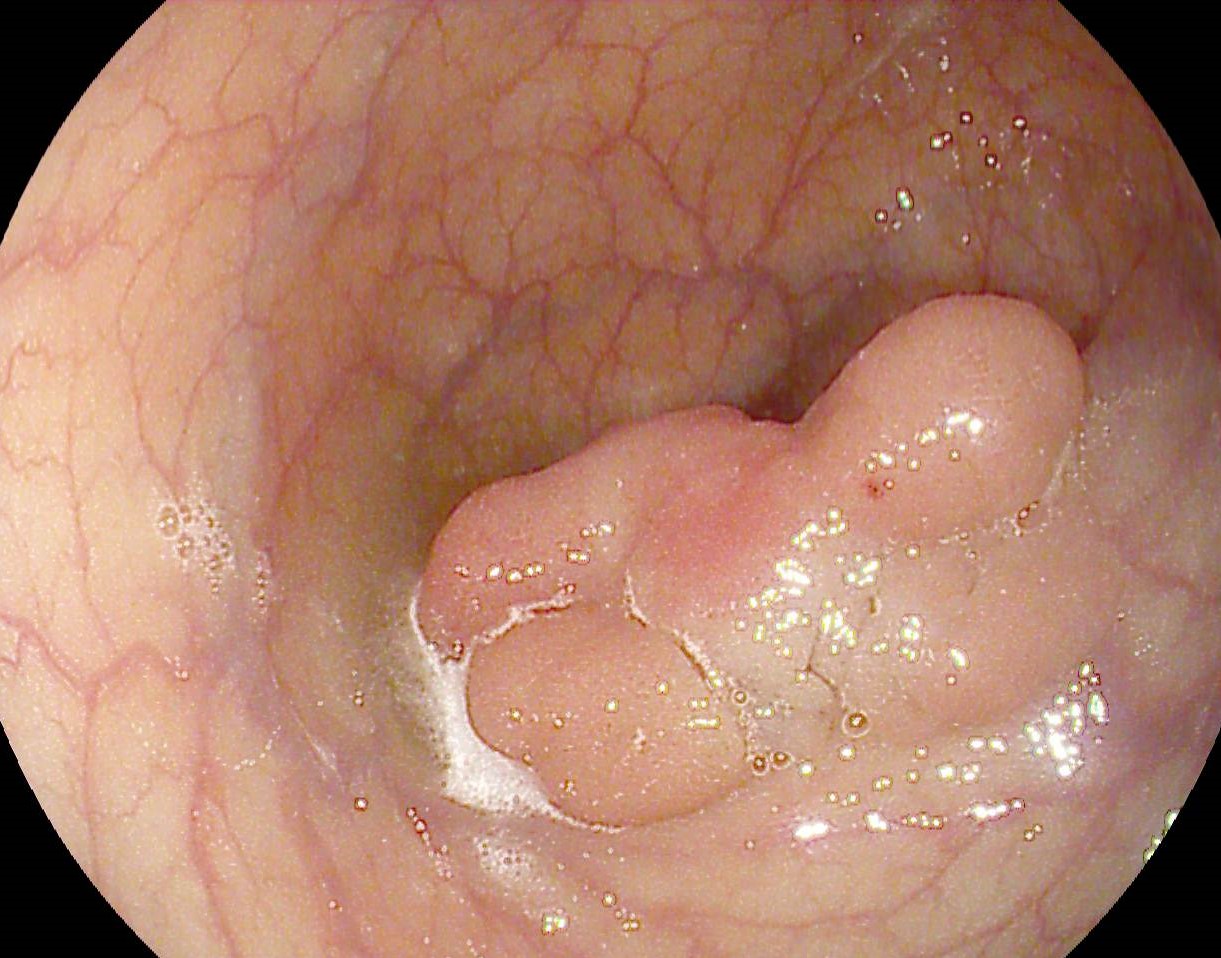
MRCP revealed fine dilations of intrahepatic bile ducts in both liver lobes due to a tight primary biliary anastomotic stricture (Figure 1)
ERCP was performed with cannulation of the main bile duct. Injection of radiopaque contrast in the biliary tree revealed a tight stricture/ stenosis at the site of anastomosis with pre-stenotic dilation of 6 mm and post stenotic dilated intrahepatic ducts. Retrograde sphincterotomy was performed followed by pneumatic dilation of the anastomotic biliary stricture with a 6 mm balloon. Two plastic biliary stents of 8Fr/10 cm, respectively 7.5 Fr/10 cm were inserted with efficient biliary drainage. The patient was discharged 3 days after the procedure with improvement of clinical status and normalization of the hepatic enzymes.
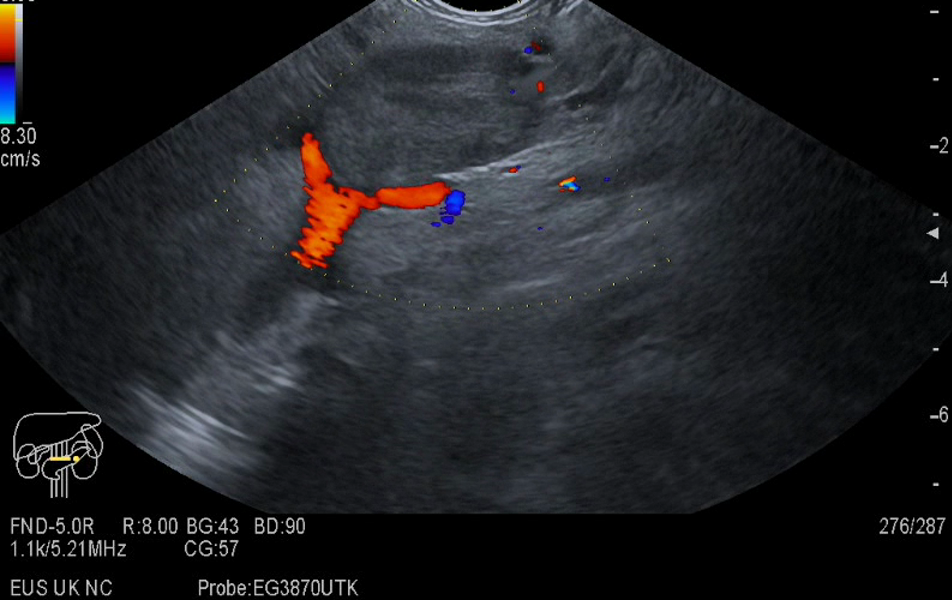
10 weeks after the procedure the patient was scheduled for endoscopic evaluation of the anastomotic biliary stricture. The bloodwork did not show significant changes. ERCP was performed with snare extraction of the two biliary stents. Injection of radiopaque contrast showed a discrete anastomotic biliary stricture without intrahepatic duct dilations. Sphincteroplasty with a 8 mm balloon and insertion of four plastic biliary stents (two 8 Fr/10 cm and two 7.5 Fr /10 cm) followed afterwards with efficient biliary drainage (Figure 2). Patient was discharged with good general condition.
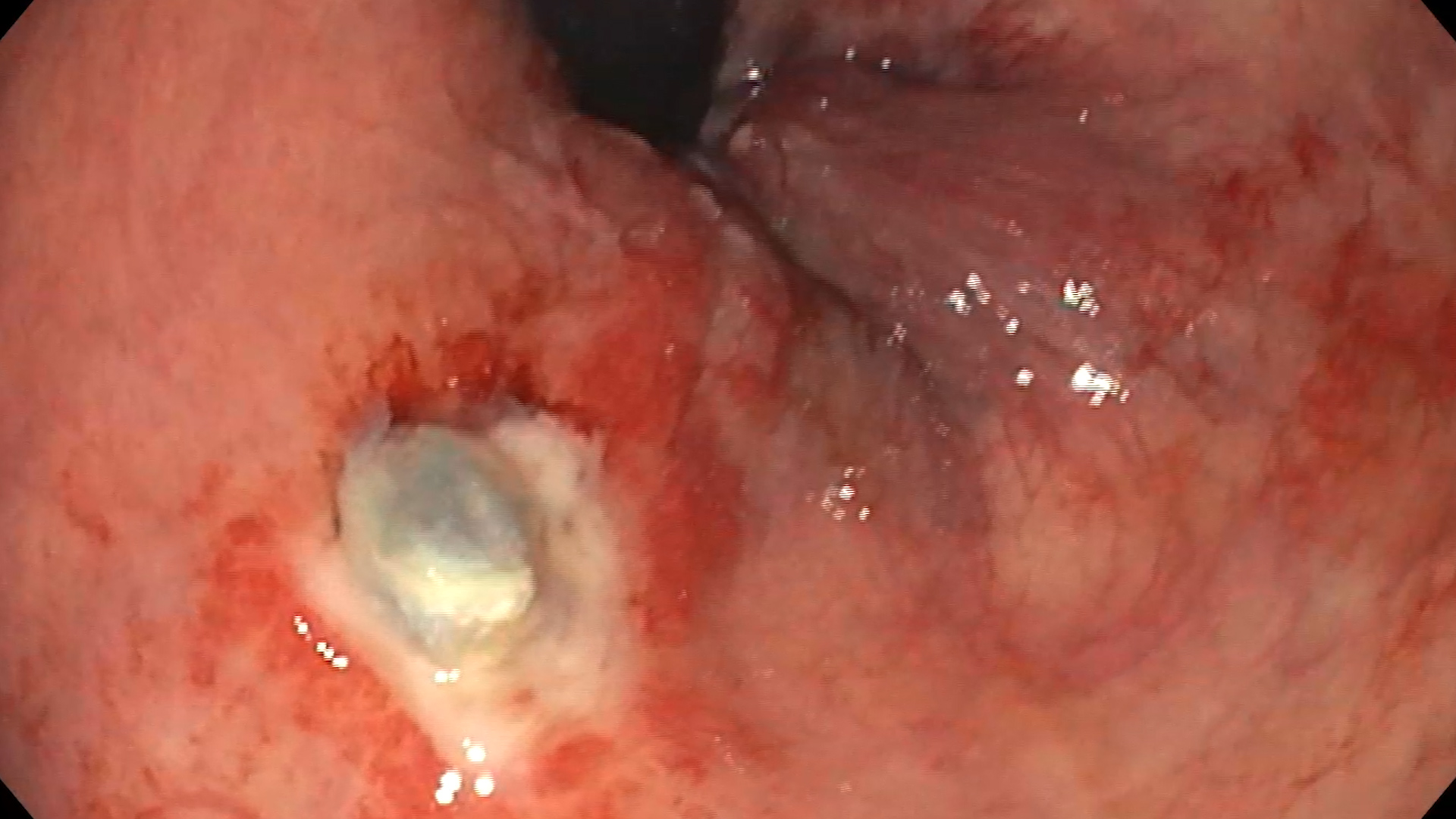
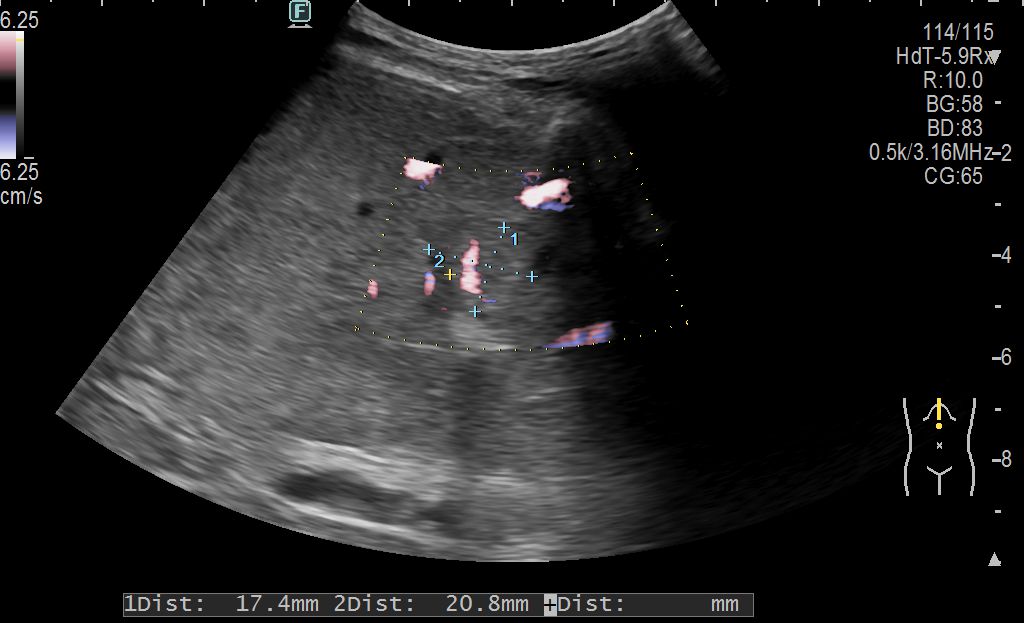
8 weeks after, the patient presented to emergency room with altered general status and pain in right hypochondrium. Bloodwork revealed leukocytosis and raised C reactive protein. Abdominal x-ray reported the migration of a biliary stent and absence of pneumoperitoneum (Figure 3). Magnetic resonance with contrast of pelvis and abdomen revealed the migration of a biliary stent, no intrahepatic duct dilations, no intraabdominal collections. ERCP was performed with extraction of all four biliary stents. Contrast injection of the biliary tract revealed the calibration of the biliary tract stricture. With frontal view endoscope on contralateral wall of major duodenal papilla a 3 mm fistula is seen. An OTSC clip- Padlock was used for complete closure of the wall defect (Figure 4). Barium swallow exam after 24 h did not reveal upper GI tract extraluminal leakage.
Benign choledocho-choledochian anastomosis stenosis. Duodenal fistula – OTSC clip mounting. Post liver transplant status.
Anastomotic biliary strictures after liver transplant represent a severe post operatory complication. The management can be either endoscopic or surgical, but the main treatment method is endoscopic biliary stenting.The method of inserting the biliary stents is guided by the possibility of advancing the guidewire in the intrahepatic bile ducts and the degree of stenosis at the level of the choledochal anastomosis. Dilation of biliary stenosis is performed with pneumatic dilation balloons or dilation bougies and is a key point in biliary stenting. Plastic biliary stents with multiple diameters or self-expanding biliary stents can be used.
The endoscopic management by ERCP for biliary anastomosis stenoses after orthotopic liver transplantation is the main method of treatment and presents a high degree of complexity. Severe complications like cholangitis, main bile duct perforation or duodenal fistulas can occur.
- Mohit Girotra, Kaartik Soota, Jagpal S Klair, Shyam M Dang, Farshad Aduli. World Journal of Gastrointestinal Endoscopy. 2015 May; 7(5): 446-459
- Carlos Macias Gomez and Jean Marc Dumonceau. Endoscopic management of biliary complications after liver transplantation: An evidence-based review. World Journal Gastrointestinal Endoscopy. 2015 Jun 10; 7(6): 606-616