See other cases
Early-Stage Distal Cholangiocarcinoma
We present the case of a 72-year-old male patient, without regular medical check-ups, who presented to the emergency department with sclero-cutaneous jaundice and generalized pruritus, accompanied by a general decline in health, with loss of appetite. Symptoms began approximately one week prior, in an apparently healthy state, and progressively worsened. The patient denies fever, chills, nausea, vomiting, or abdominal pain.
The patient was in generally good condition: conscious, cooperative, temporo-spatially oriented, with icteric skin and sclera, no scratch lesions, normal adipose tissue distribution, cardiorespiratory status stable, no abdominal pain, intestinal transit present, acholic stools, and dark-colored urine for about 2–3 days.
Biological tests: Hepatic cholestasis with 7 mg/dL total bilirubin, predominantly direct bilirubin, without leukocytosis or inflammatory syndrome, and no hepatic cytolysis.
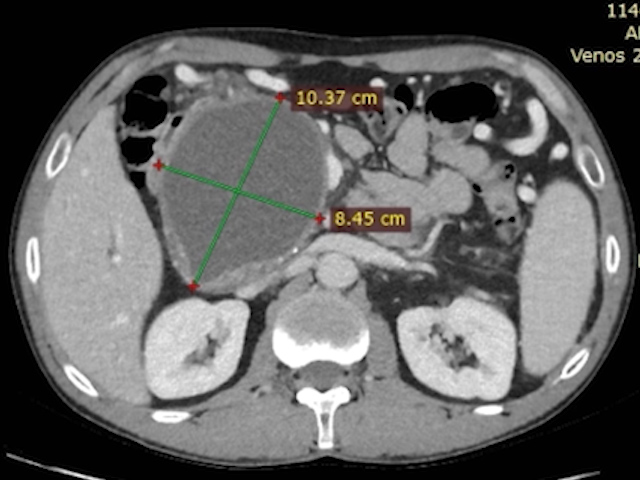
CT Scan revealed:
- A tissue lesion located cranially at the head/uncinate process junction of the pancreas, measuring approximately 19/19/23 mm, isodense, with hyperenhancement during the arterioportal phase. There is a preserved cleavage plane from the spleno-mesenteric confluence, portal vein trunk, celiac trunk, hepatic artery, and superior mesenteric artery, as well as from the adjacent duodenum.
- No cleavage plane and evidence of extrinsic/invasive compression at the distal common bile duct (CBD) and cystic duct insertion, causing upstream biliary dilation (CBD diameter 15 mm, cystic duct 9 mm, main centrohilar bile ducts 11 mm).
- No signs of secondary metastases.
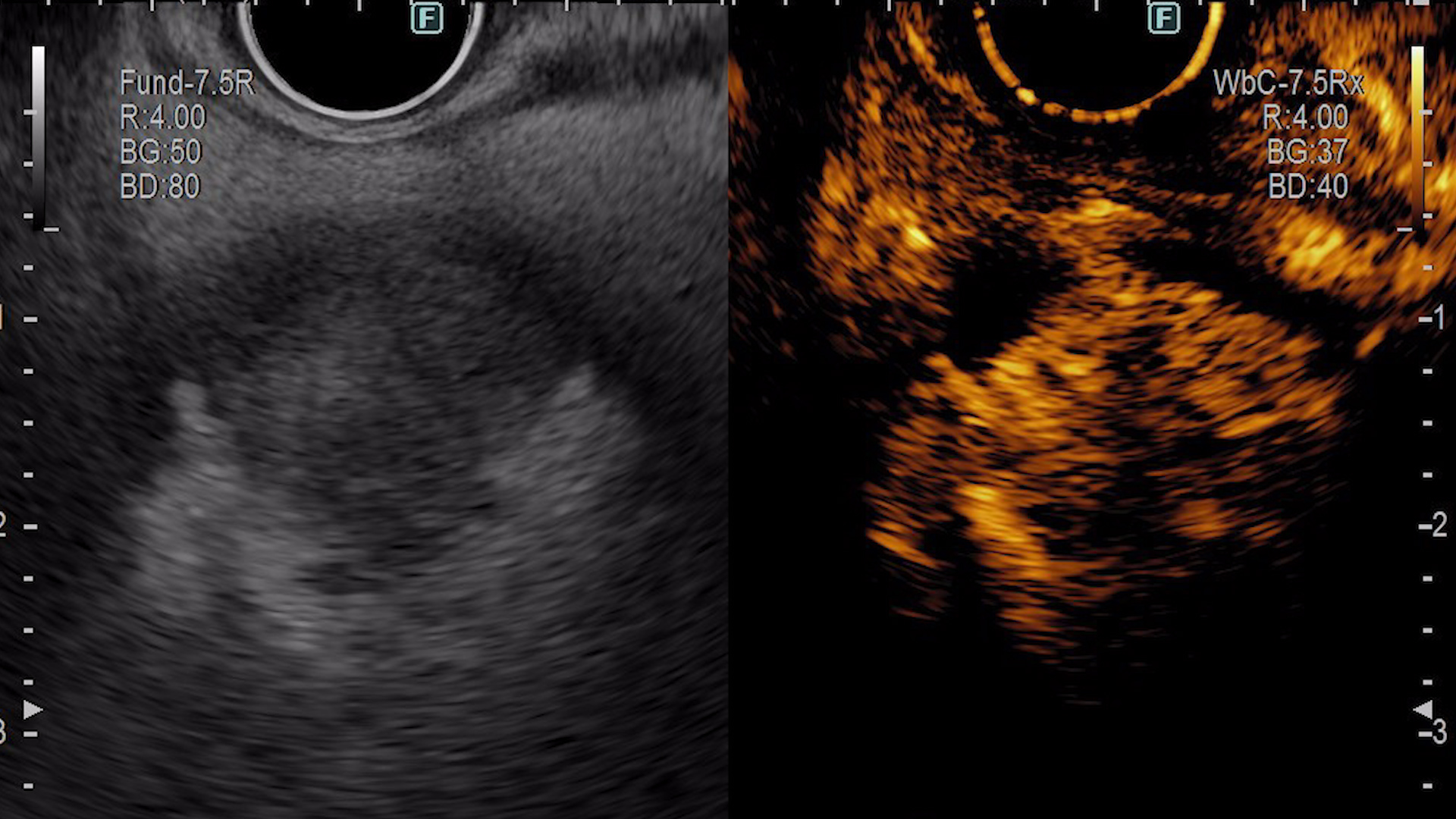
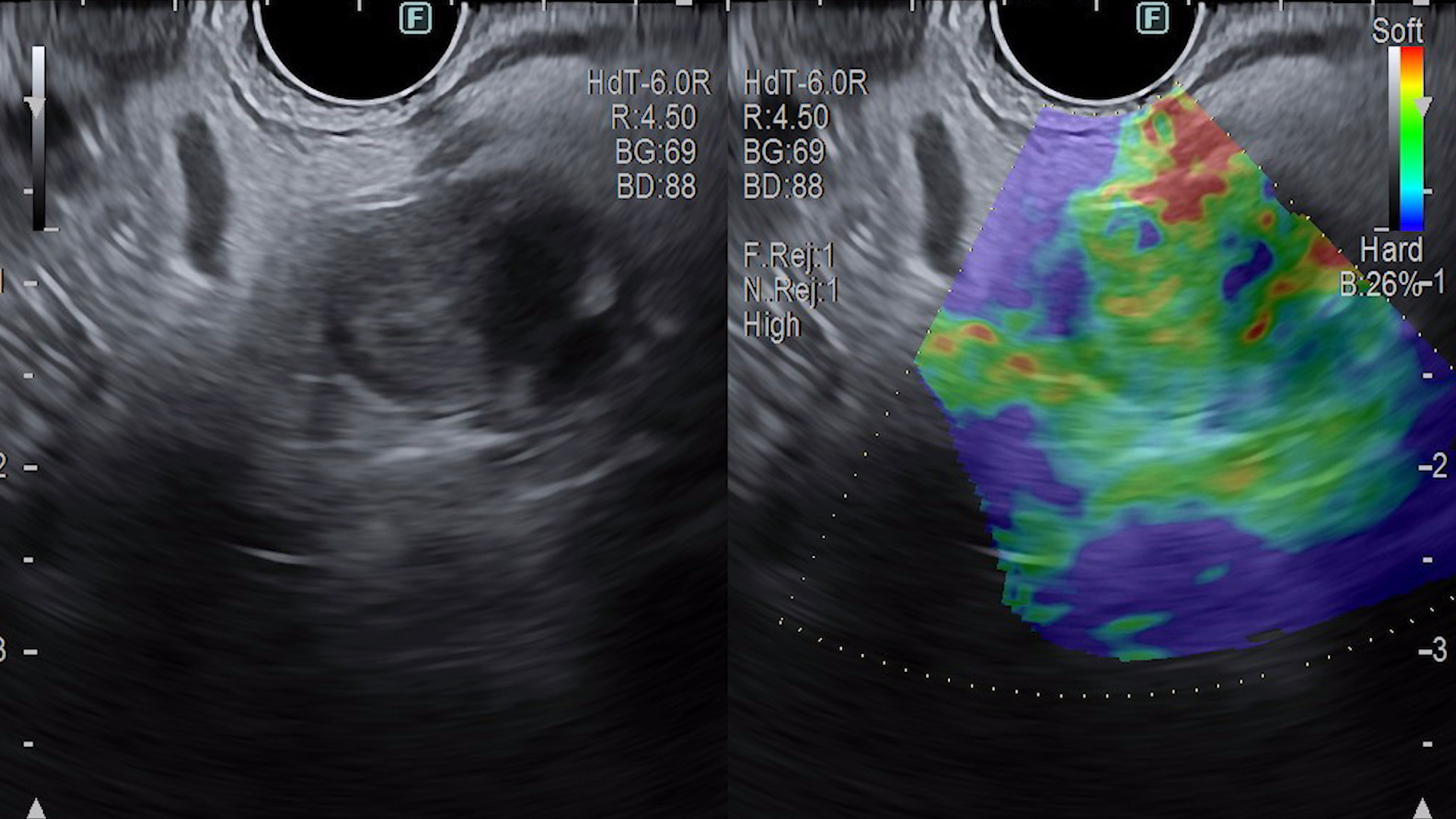
Endoscopic Ultrasound (EUS):
A solid lesion was identified in the distal common bile duct, without papillary invasion, extending to the level of the cystic duct but not invading it, measuring 13.7/20.8 mm. The lesion is hyperechoic with irregular margins. Vascularity present on Doppler exam (Fig. 1). Following contrast administration (SonoVue 4.8 mL), the lesion was hyperenhancing in the arterial phase with rapid wash-out in the venous phase (Fig. 2). Elastography showed a soft appearance (Fig. 3). Two passes were performed with a 22G FNB histological needle (MicroTech, FNB) using a transduodenal approach.
Magnetic Resonance Imaging (MRI):
An intraluminal tumor formation on the posterior wall of the intrapancreatic segment of the common bile duct. A few nonspecific locoregional lymph nodes. No secondary hepatic lesions were detected.
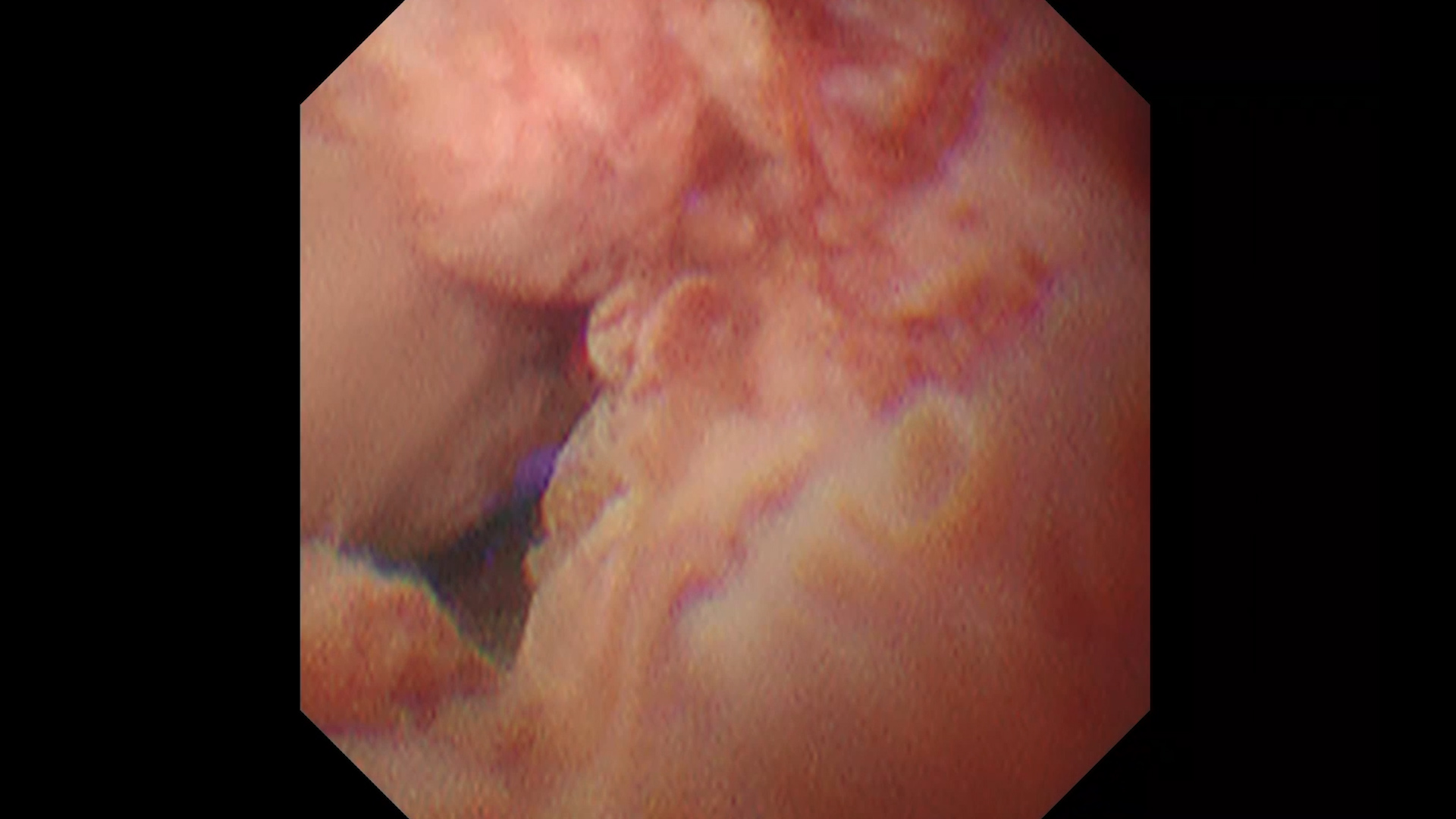
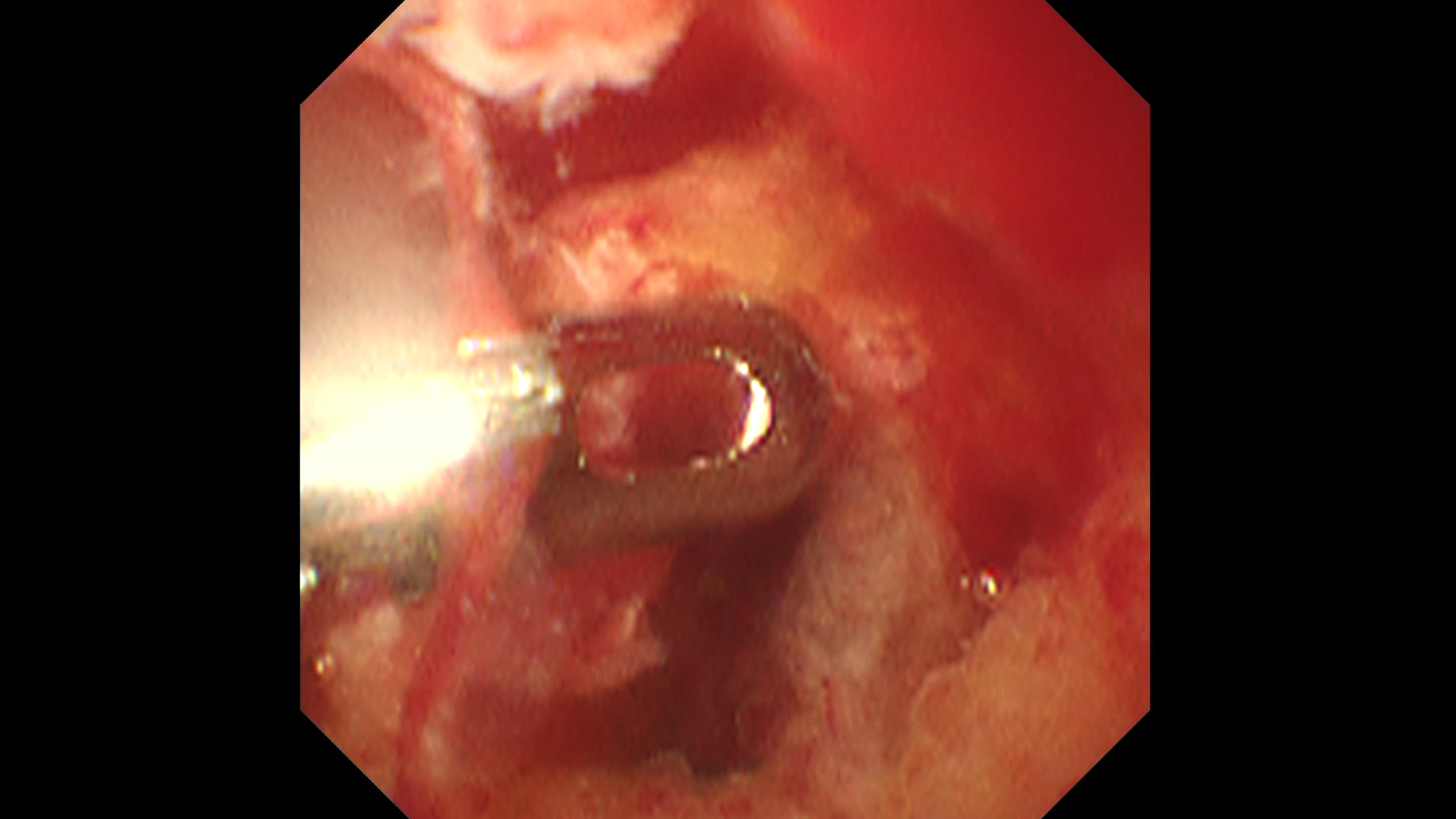
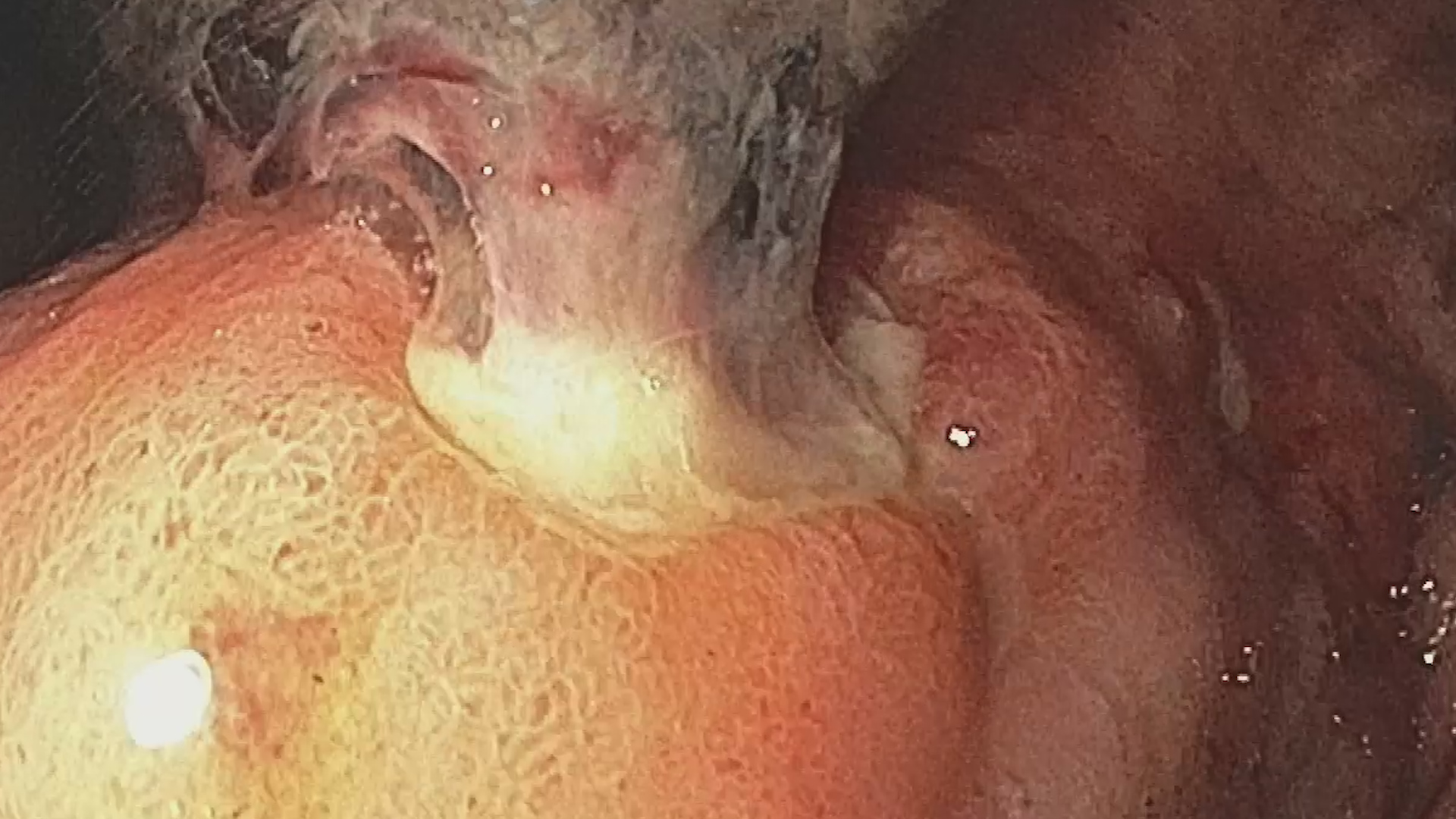
Endoscopic Retrograde Cholangiopancreatography (ERCP) with cholangioscopy:
A wide sphincterotomy was performed. Cholangioscopy revealed a friable, highly vascularized tumor formation that bled upon simple passage of the cholangioscope (Fig. 4). Targeted biopsies were collected (Fig. 5). A guidewire and a fully covered self-expandable metal stent (FC-SEMS) of 10Fr, 6 cm was placed, with successful biliary decompression. Radiologically, the stent extended 2 cm above the tumor.
Histopathologic Examination (from EUS and cholangioscopy samples):
The histopathological appearance was suggestive of a poorly differentiated epithelial tumor proliferation, likely of biliary origin. Immunohistochemical testing is necessary for confirmation.
Distal cholangiocarcinoma (dCCA) located in the intrapancreatic segment of the common bile duct, clinical stage IIIB (T2N1M0 according to TNM classification).
Cholangiocarcinomas are tumors originating from the epithelium of the bile ducts. Based on location, they can be: intrahepatic, perihilar, and distal1. The case presented involves a distal cholangiocarcinoma with intraductal growth. Differential diagnosis between cholangiocarcinoma and other malignant pathologies is often extremely difficult.
In this case, the patient benefited not only from conventional imaging methods but also from high-accuracy techniques. Elastography performed during EUS revealed a low stiffness of the tumor, a characteristic that may be present in cholangiocarcinomas2. Contrast-enhanced imaging confirmed the malignant nature of the lesion, demonstrating typical features such as intense arterial-phase enhancement and early venous-phase wash-out3. Cholangioscopy enabled direct visualization of the lesion, as well as biopsy sampling.
Given the early oncologic stage, the next step considered is curative surgical resection via cephalic duodenopancreatectomy (Whipple procedure). Following final staging and immunohistochemistry, adjuvant treatment will be decided.
In conclusion, bile duct tumors pose a diagnostic challenge, often being diagnosed at late stages. Even when curative intervention is performed early, with R0 resection margins, the recurrence rate exceeds 50% at 5 years4.
- Guedj, N. Pathology of Cholangiocarcinomas. Curr. Oncol. 2023, 30, 370-380. https://doi.org/10.3390/curroncol30010030
- Mohebbi A, Mohammadzadeh S, Mohebbi S, Mohammadi A, Tavangar SM. Diagnostic performance of ultrasound elastography in differentiating hepatocellular carcinoma and intrahepatic cholangiocarcinoma: a systematic review and meta-analysis. Abdom Radiol (NY). 2025 Feb; 50(2): 633-645. doi: 10.1007/s00261-024-04502-6. Epub 2024 Aug 14. PMID: 39138663.
- Gismondo Velardi G, Lico M, Teti A, Maccarone R, Casuscelli G, Militano L, Trecroci IV, Mendicino M, Parlati A, De Caridi A, Loria G, Loria S, Loria S, Gambardella D, Tedesco M, Frosina F, Falco P, Loria F. Diagnosis of intrahepatic cholangiocarcinoma with CEUS. J Ultrason. 2024 Feb 27; 24(96): 20240005. doi: 10.15557/jou.2024.0005. PMID: 38419841; PMCID: PMC10897370.
- Gorji L, Beal EW. Surgical Treatment of Distal Cholangiocarcinoma. Curr Oncol. 2022 Sep 17; 29(9): 6674-6687. doi: 10.3390/curroncol29090524. PMID: 36135093; PMCID: PMC9498206.