See other cases
A 79-year-old female patient, with a history of operated and radiotreated breast cancer, presents with sclero-cutaneous jaundice and pruritus.
The patient was conscious, cooperative, underweight, complains of insomnia, presents with sclero-cutaneous jaundice and pruritus, dark urine, and acholic stools.
CT: Suggests a pancreatic head tumor and reveals intra- and extrahepatic bile duct dilation with multiple metastatic liver lesions.
MR: Findings indicative of a proliferative process in the pancreatico-duodenal groove, biliary obstruction in the preampullary region, marked intra- and extrahepatic bile duct dilations, and secondary hepatic lesions.
ERCP attempt: Initial bile duct cannulation attempt fails with a 0.035-inch guidewire, followed by another failure with a 0.025-inch guidewire; the procedure was abandoned.
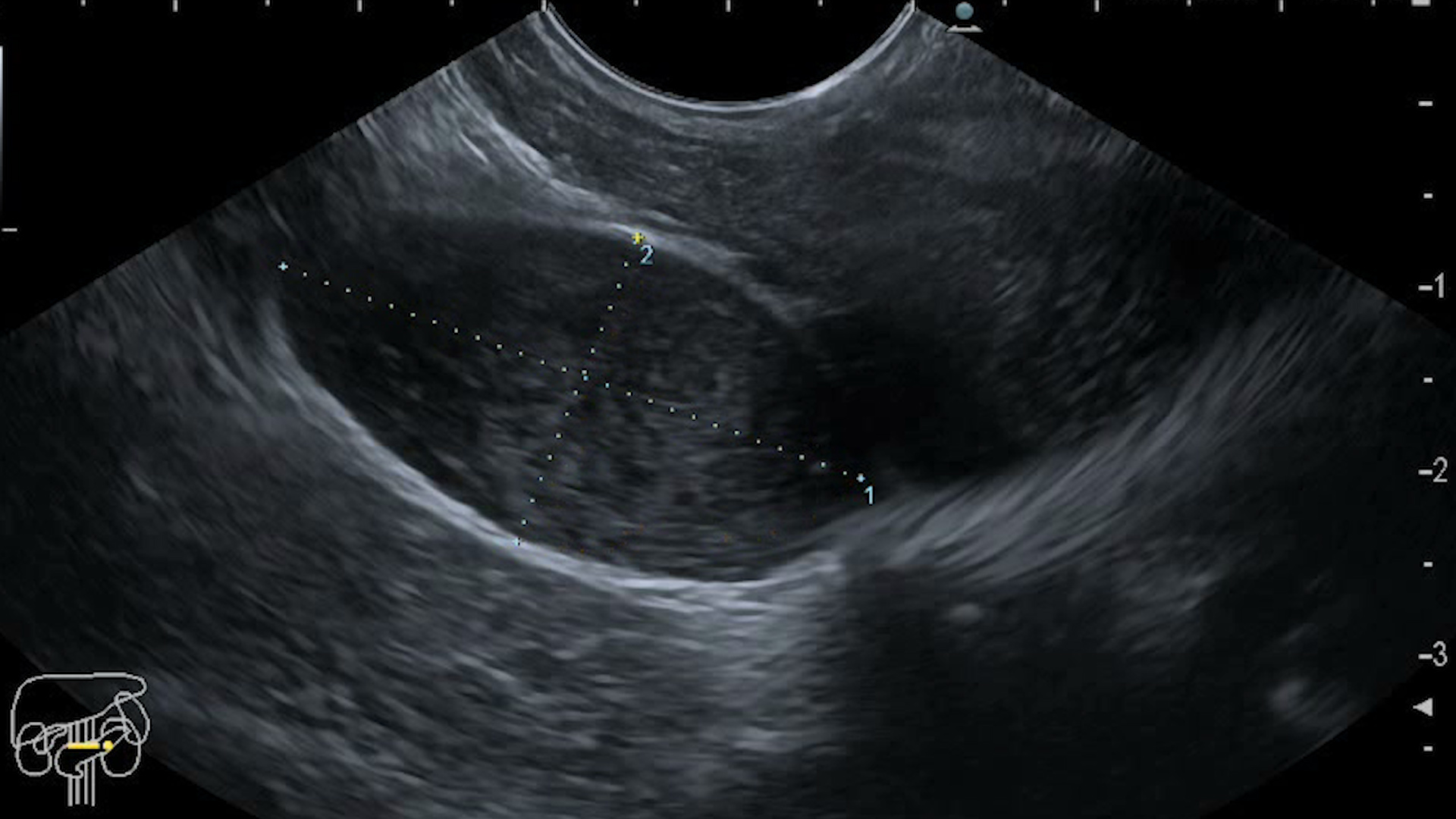
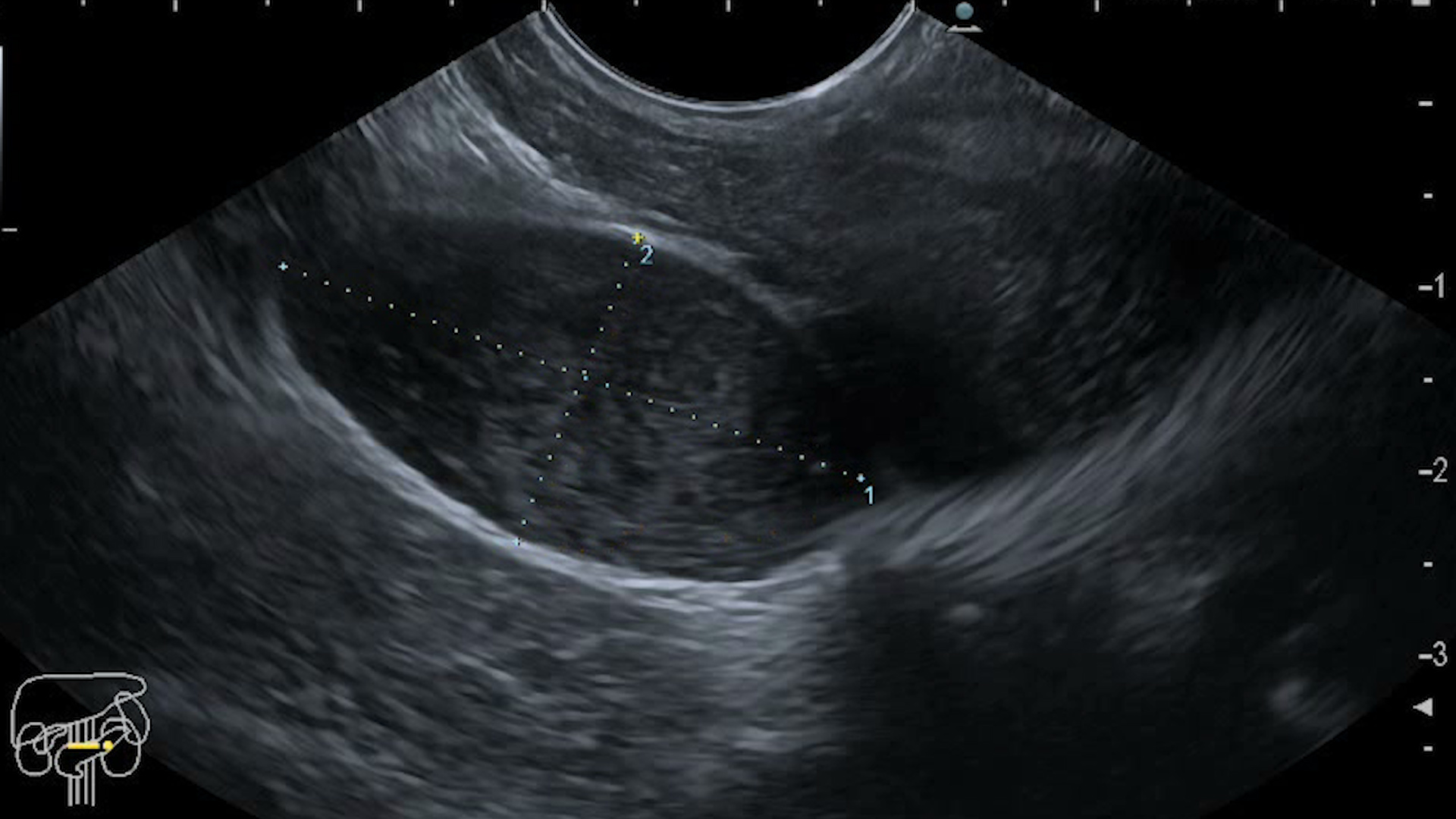
Diagnostic endoscopic ultrasound: Fine-needle biopsy of the tumor in the papillary projection area, involving the common bile duct and pancreatic duct (Figure 2-4). Confirmation of secondary hepatic lesions.
Therapeutic endoscopic ultrasound: EUS-guided bile duct drainage (choledochoduodenostomy) with a Hotaxios 8/8 mm stent and collection of bile cultures, which tested positive for Enterococcus (Figura 5-7).
Histopathological Diagnosis: Histological appearance and immunohistochemical profile consistent with well-differentiated adenocarcinoma (G1).
Malignant distal biliary obstruction is most commonly caused by pancreatic cancer, cholangiocarcinoma, or metastases. In this case, imaging investigations identified an ampullary mass, with EUS-BD being considered a better alternative than PTBD, when ERCP fails, allowing both biliary drainage and tissue sampling. Compared to ERCP, EUS-guided choledochoduodenostomy (EUS-CDS) offers a similar success rate.
For benign tumors, EUS-guided rendez vous (EUS-RV) is preferred.
For malignant tumors, when there is access to the duodenal papilla:
If papilla access is obstructed:
Stent misdeployment, relatively common in EUS-CDS, is associated with an extrahepatic bile duct diameter of ≤ 15 mm and can be avoided by deploying hallway the distal flange while the catheter is pushed more distally.
EUS-BD is an effective alternative to PTBD, after ERCP failure, as it allows both biliary drainage and tissue sampling, making it the preferred method in certain cases.
See other cases