See other cases
Double endoscopic stenting for an advanced pancreatic head adenocarcinoma
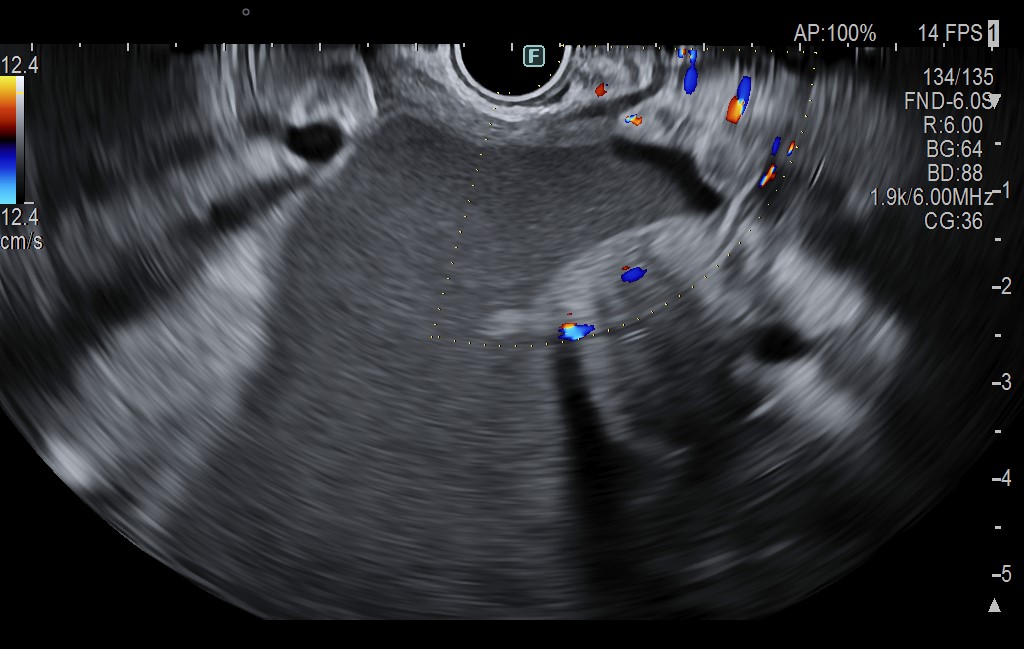
A 55-year-old patient, recently diagnosed with a pancreatic head neoplasm (ductal adenocarcinoma) with peritoneal metastases, presented to the Emergency Department with melena and recent-onset jaundice. One month prior, the patient had sought care at another facility for upper gastrointestinal bleeding secondary to a gastric ulcer, which was histopathologically confirmed as a consequence of adjacent tumor invasion. At that time, a definitive diagnosis of the pancreatic lesion was established via EUS with fine-needle biopsy. The echoendoscope could not be advanced into the duodenum due to a likely tumor-induced duodenal stricture.
Clinically, the patient presented an altered general status, he was jaundiced, with a markedly distended abdomen due to ascites, and with diffuse abdominal tenderness both spontaneously and upon palpation. Rectal examination revealed melena.
Biologically, there was evidence of severe anemia, hypoalbuminemia and significant cholestasis.
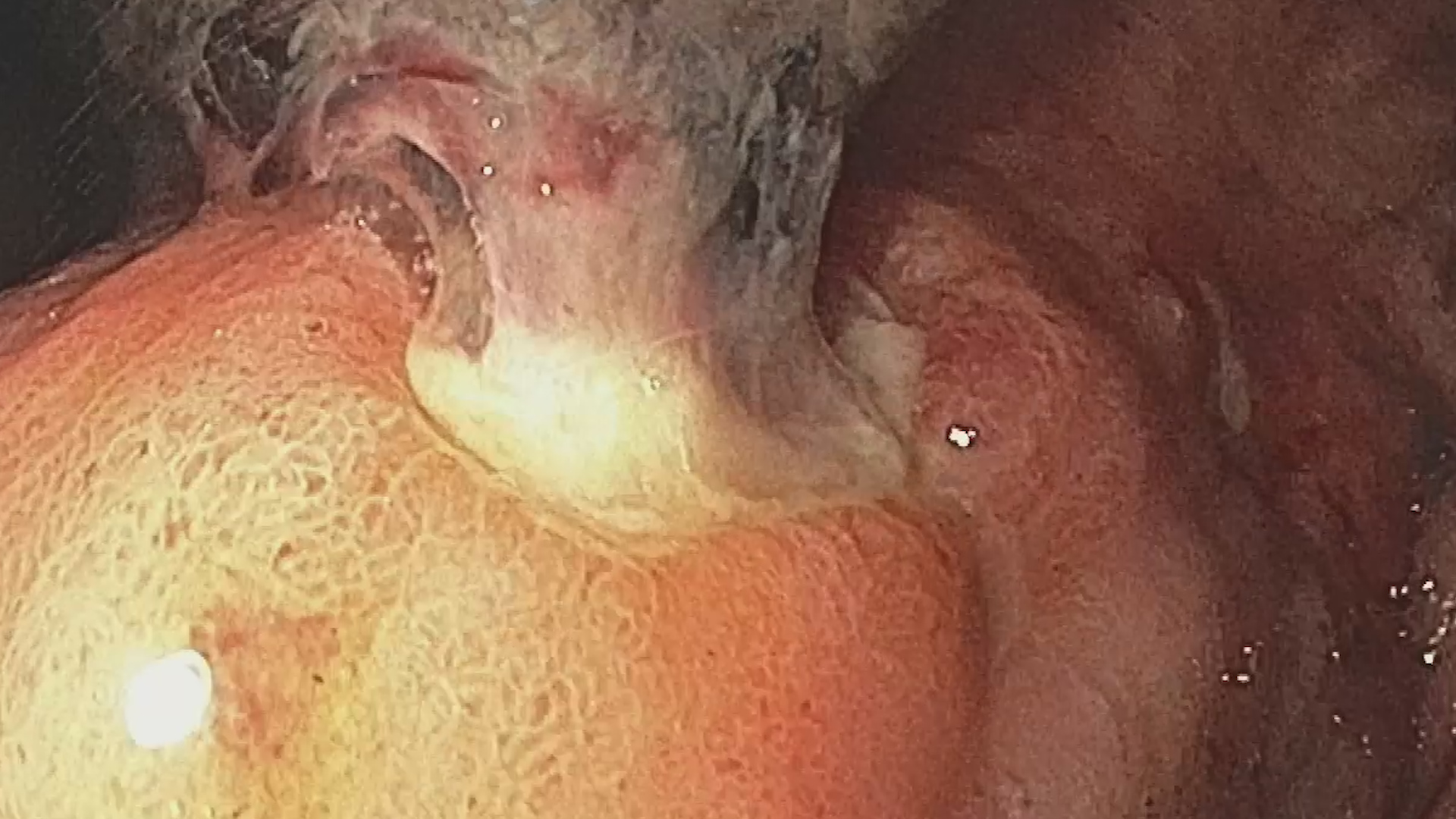
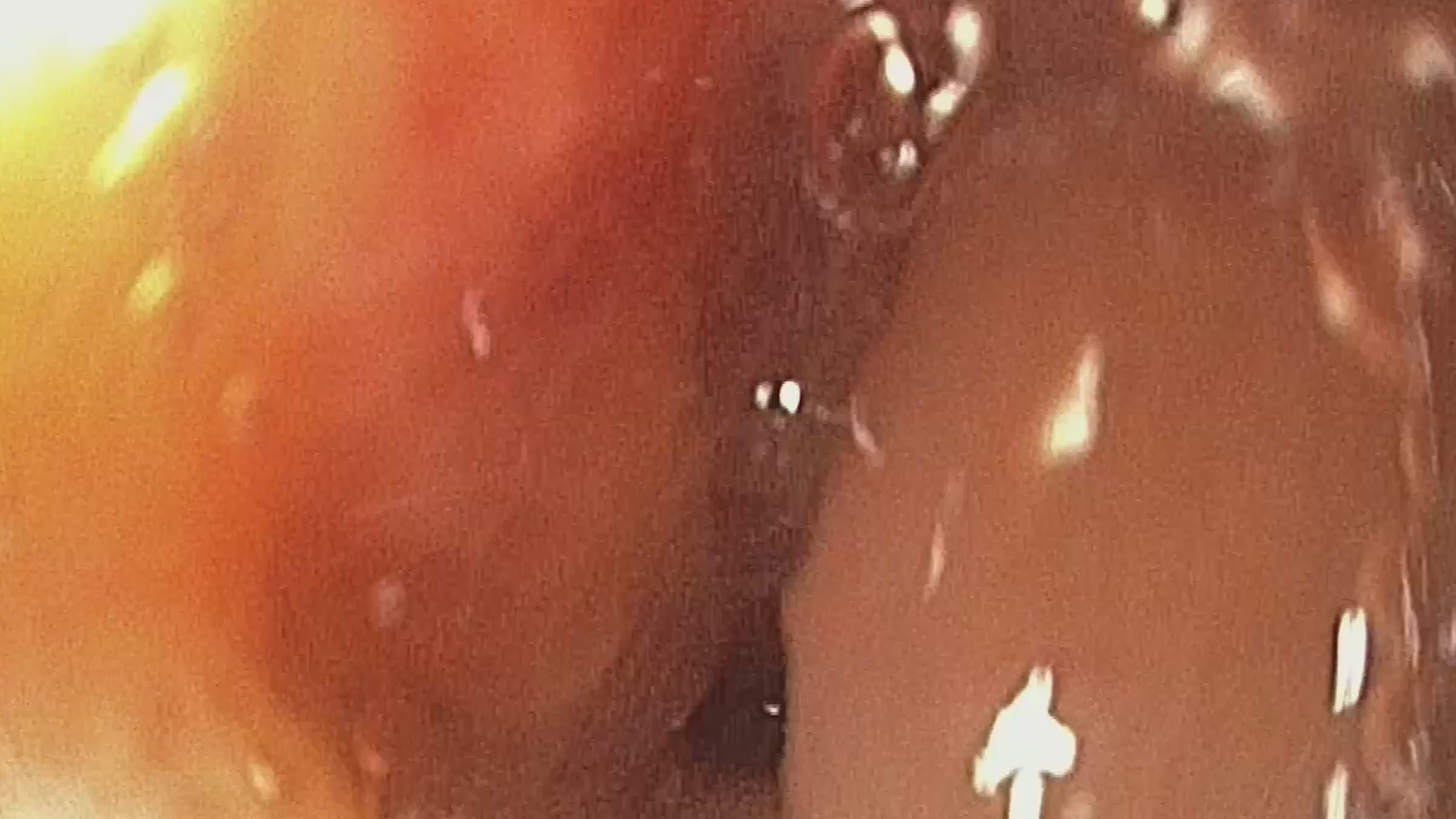
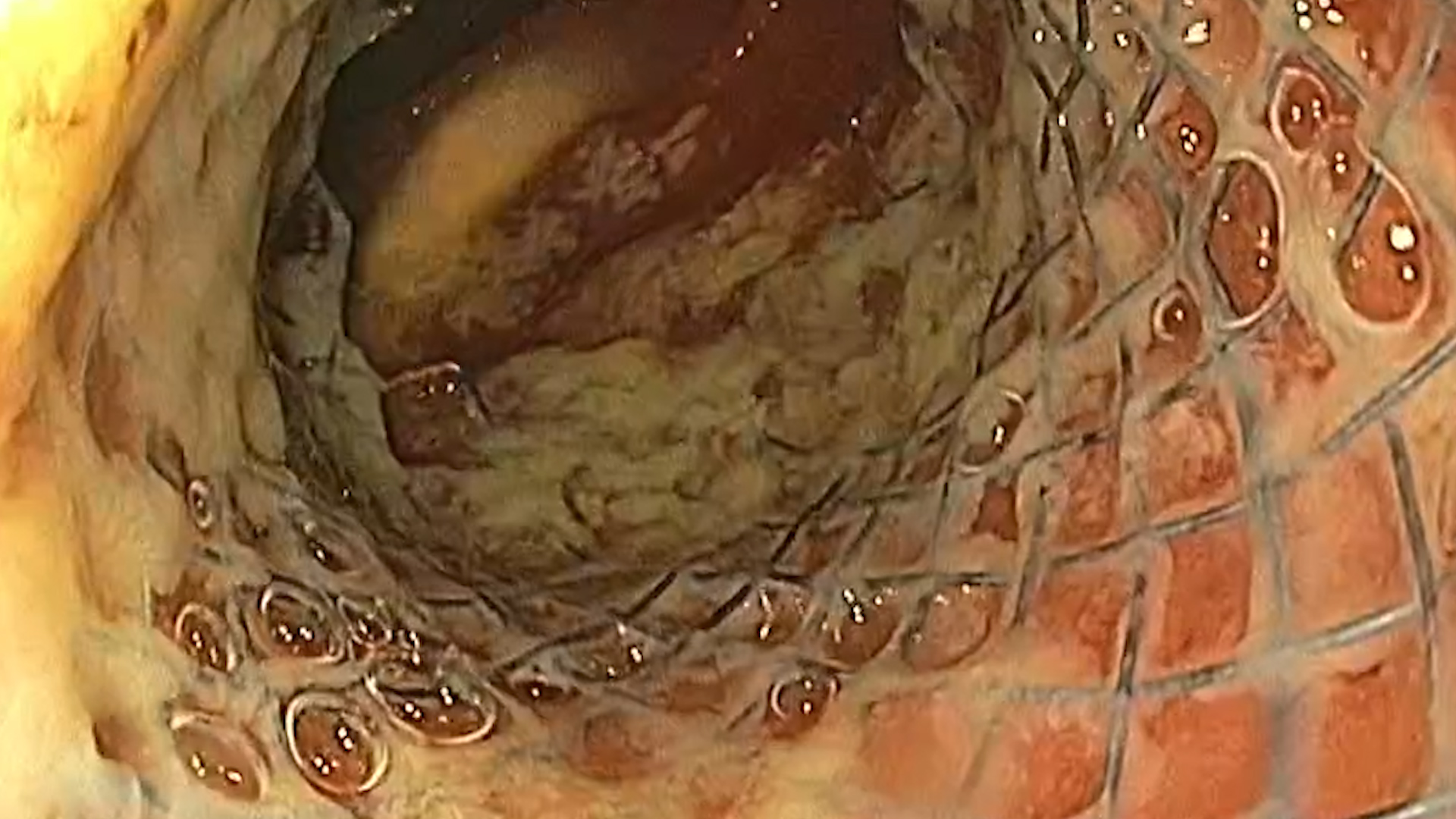
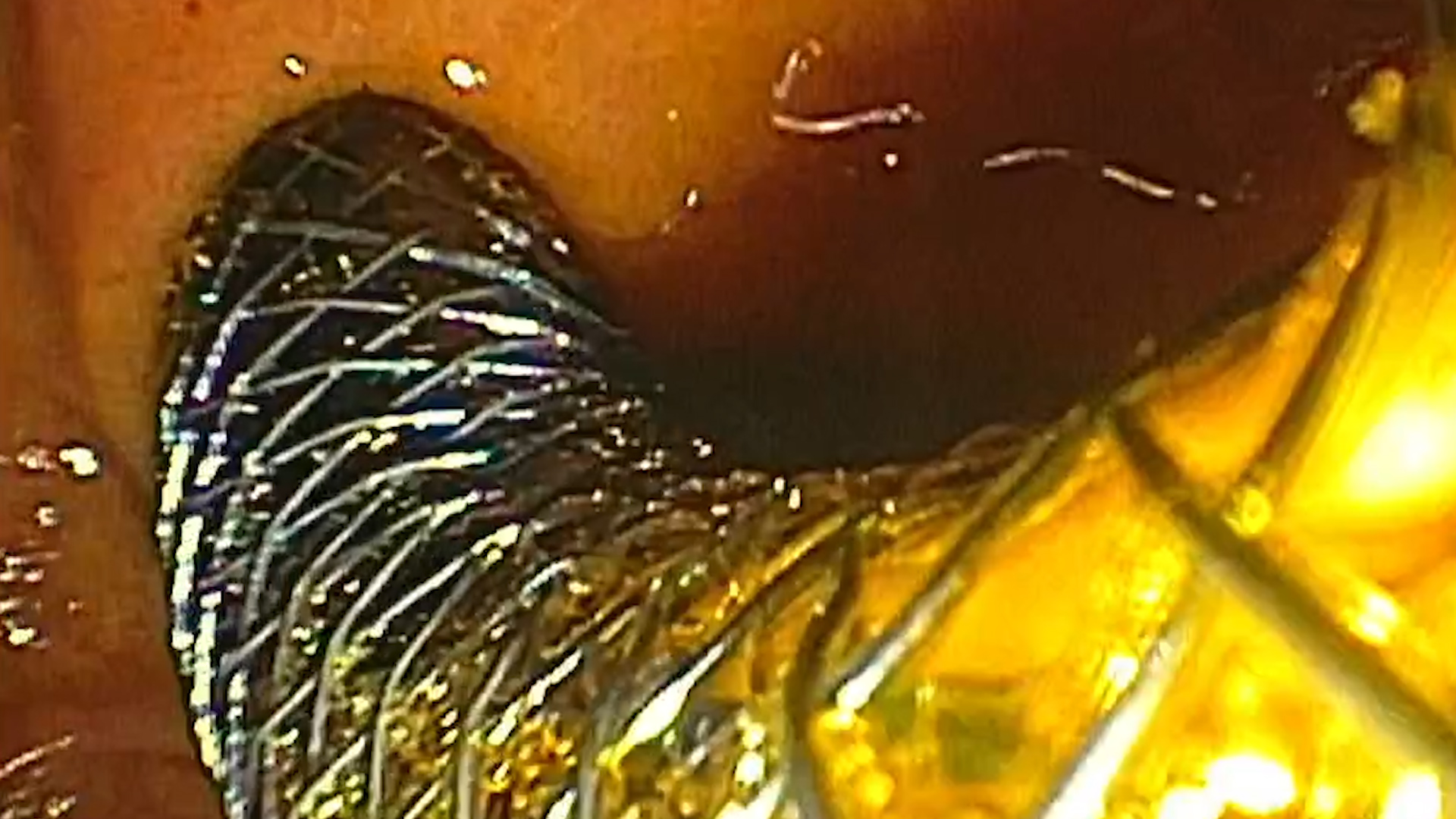
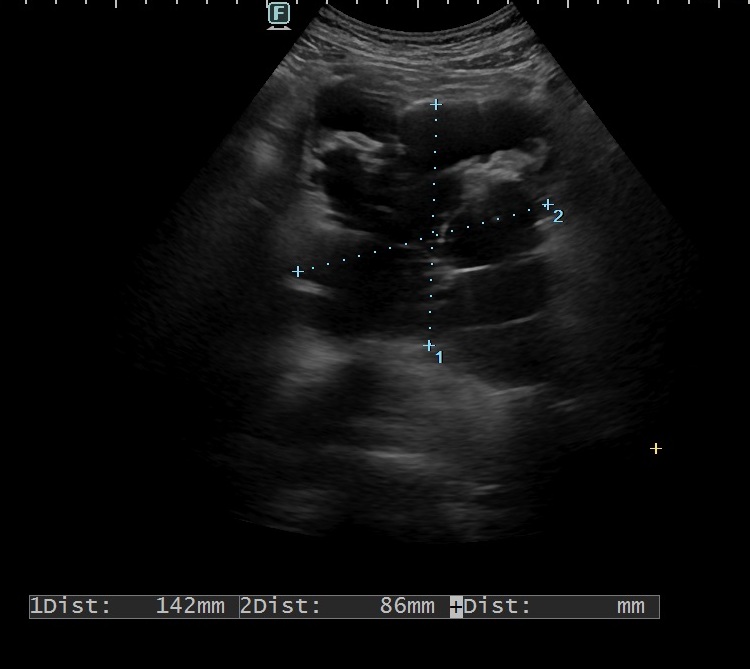
The first investigation performed was an urgent upper gastrointestinal endoscopy, which revealed significant gastric stasis and an irregular gastric ulcer approximately 20 mm in size (Figure 1), with a large adherent clot that could not be removed endoscopically (Forrest IIB). A tight duodenal stricture with malignant aspect was also observed, which could be passed with the diagnostic endoscope but not with the duodenoscope (Figure 2), extending from the duodenal bulb to the proximity of the major papilla, which appeared normal. Consequently, conservative management of the gastric ulcer was initiated, with a favorable outcome. 48 hours later, enteral stenting was performed under radiological guidance – a 20×80 mm self-expandable uncovered metal stent was positioned trans-pylorically (Figure 3-4). Subsequently, two days later, ERCP was performed (Figure 5). Cholangiography revealed a short distal common bile duct stricture with malignant features, prompting the placement of a 10 Fr/10 cm plastic biliary stent. The patient’s condition improved significantly, with near-complete resolution of the cholestasis at the time of discharge. One week later, the patient returned for fever accompanied by the recurrence of jaundice. Laboratory tests indicated significant leukocytosis with neutrophilia and cholestasis. ERCP was repeated, and the plastic biliary stent was replaced with a fully covered 8×80 mm expandable metal stent, ensuring effective drainage (Figure 6-7). The patient responded well to broad-spectrum antibiotic therapy.
Upper gastrointestinal bleeding from a gastric ulcer due to adjacent tumor invasion. Duodenal stricture from adjacent tumor invasion. Distal common bile duct stricture. Pancreatic head neoplasm (pancreatic ductal adenocarcinoma) with peritoneal metastases.
Complications associated with pancreatic tumors are numerous, however duodenal and biliary obstructions carry the most significant functional consequences. In this case, the patient’s presentation was atypical, featuring upper gastrointestinal bleeding from an ulcer due to adjacent tumor invasion, alongside malignant duodenal stenosis and jaundice resulting from common bile duct invasion. Currently, endoscopic techniques offer a wide range of options for palliation. Regarding gastric outlet obstruction, management can be either endoscopic (via the placement of a trans-pyloric enteral stent or a EUS-guided gastroenterostomy) or surgical, through the creation of a digestive bypass. Generally, the endoscopic approach is reserved for patients with low survival rates or those considered to have a high surgical risk. Duodenal stenosis associated with a biliary stricture presents particular challenges in endoscopic management. Enteral stenting is performed under radiological guidance, requiring precise placement of a metal stent in order to avoid obstructing the papilla. Therefore, marking of the ampullary region is necessary, either by submucosal injection of contrast material or by placing a proximity hemostatic clip. Biliary decompression should ideally be addressed approximately 48 hours after enteral stenting, to allow for adequate stent expansion.
Endoscopic approach represents a minimally invasive option for palliation of duodenal and biliary obstruction in patients with advanced pancreatic head neoplasms. The procedure is complex but provides prompt recovery associated with rapid improvement in gastric outlet obstruction and jaundice.
1. Dumonceau JM, Tringali A, Papanikolaou IS et al. Endoscopic biliary stenting: indications, choice of stents, and results: European Society of Gastrointestinal Endoscopy (ESGE) Clinical Guideline – Updated October 2017. Endoscopy. 2018;50(9):910-930.
2. Reijm AN, Zellenrath PA, van der Bogt RD et al. Self-expandable duodenal metal stent placement for the palliation of gastric outlet obstruction over the past 20 years. Endoscopy. 2022;54(12):1139-1146.
3. Mazur R, Trna J. Principles of Palliative and Supportive Care in Pancreatic Cancer: A Review. Biomedicines. 2023;11(10):2690.