See other cases
Dieulafoy lesion
A 57-year-old patient with no medical history presented with hematemesis and melena of 24-hour onset.
Pallor, BP = 120/80 mmHg, HR = 113 bpm, normal abdominal examination, liver and spleen clinically within normal limits, on rectal exam – melena.
Hemoglobin – 6.2 g/dL, normal RBC indices.
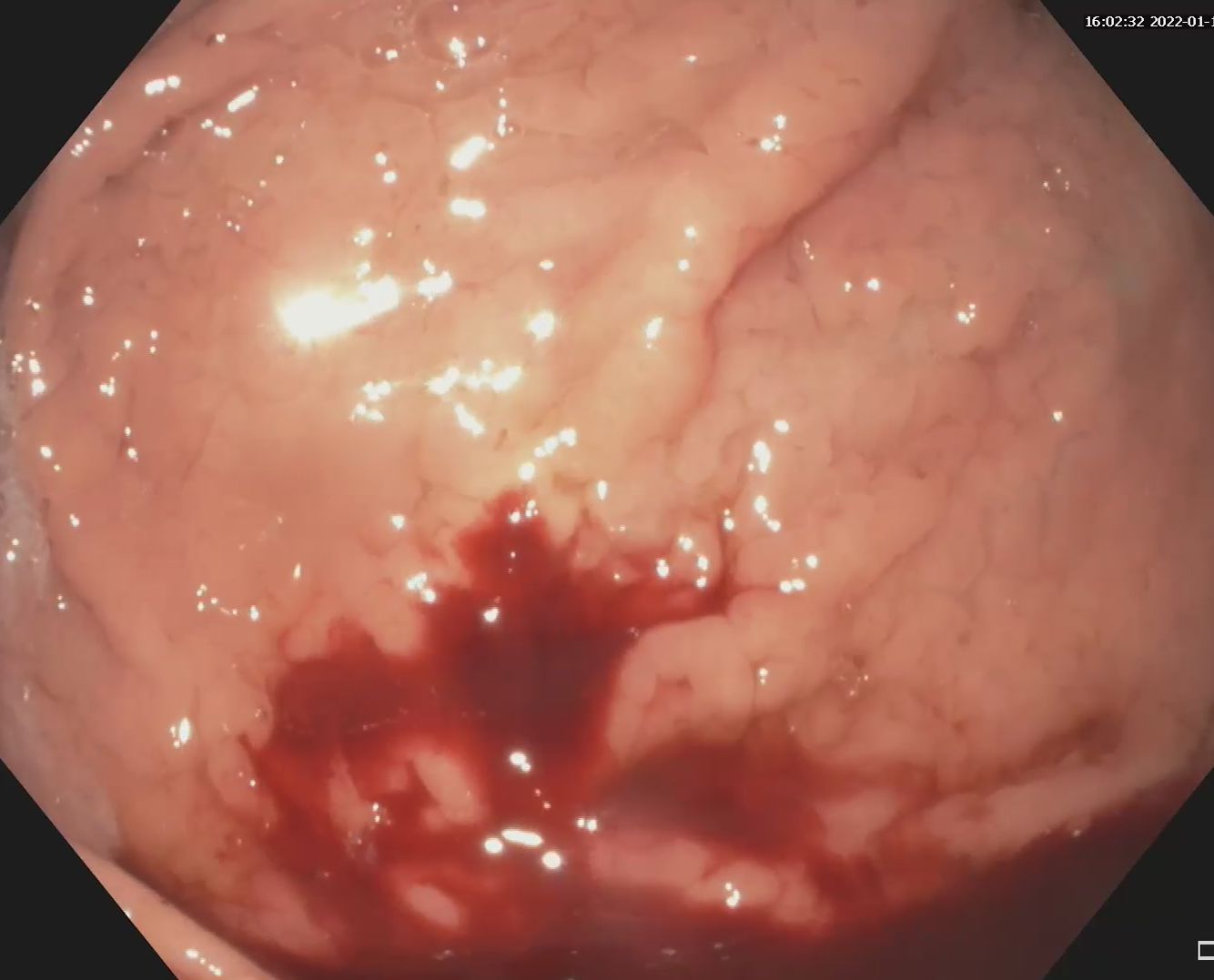
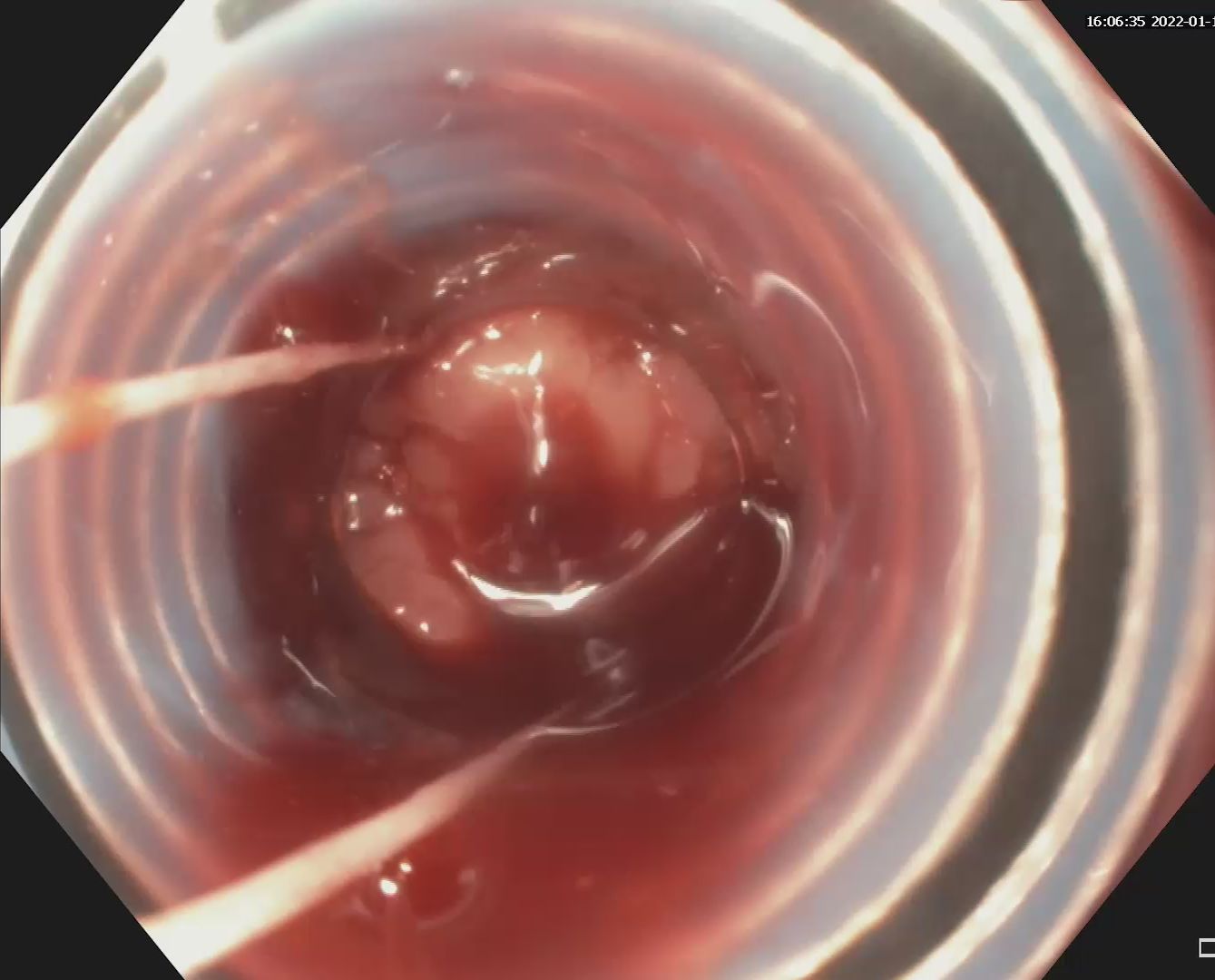
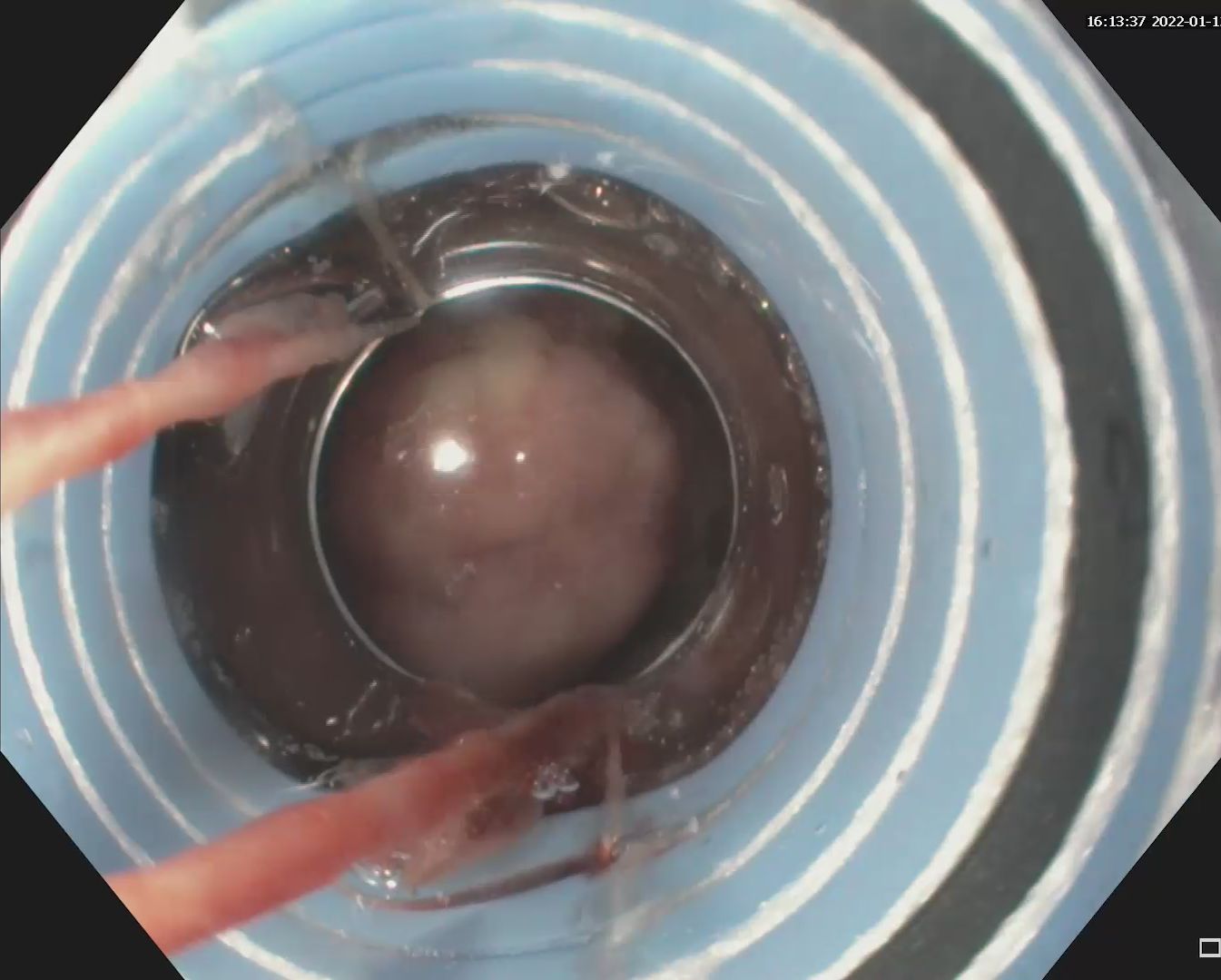
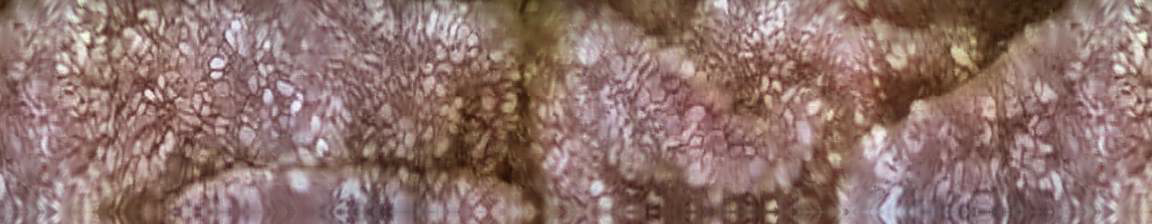
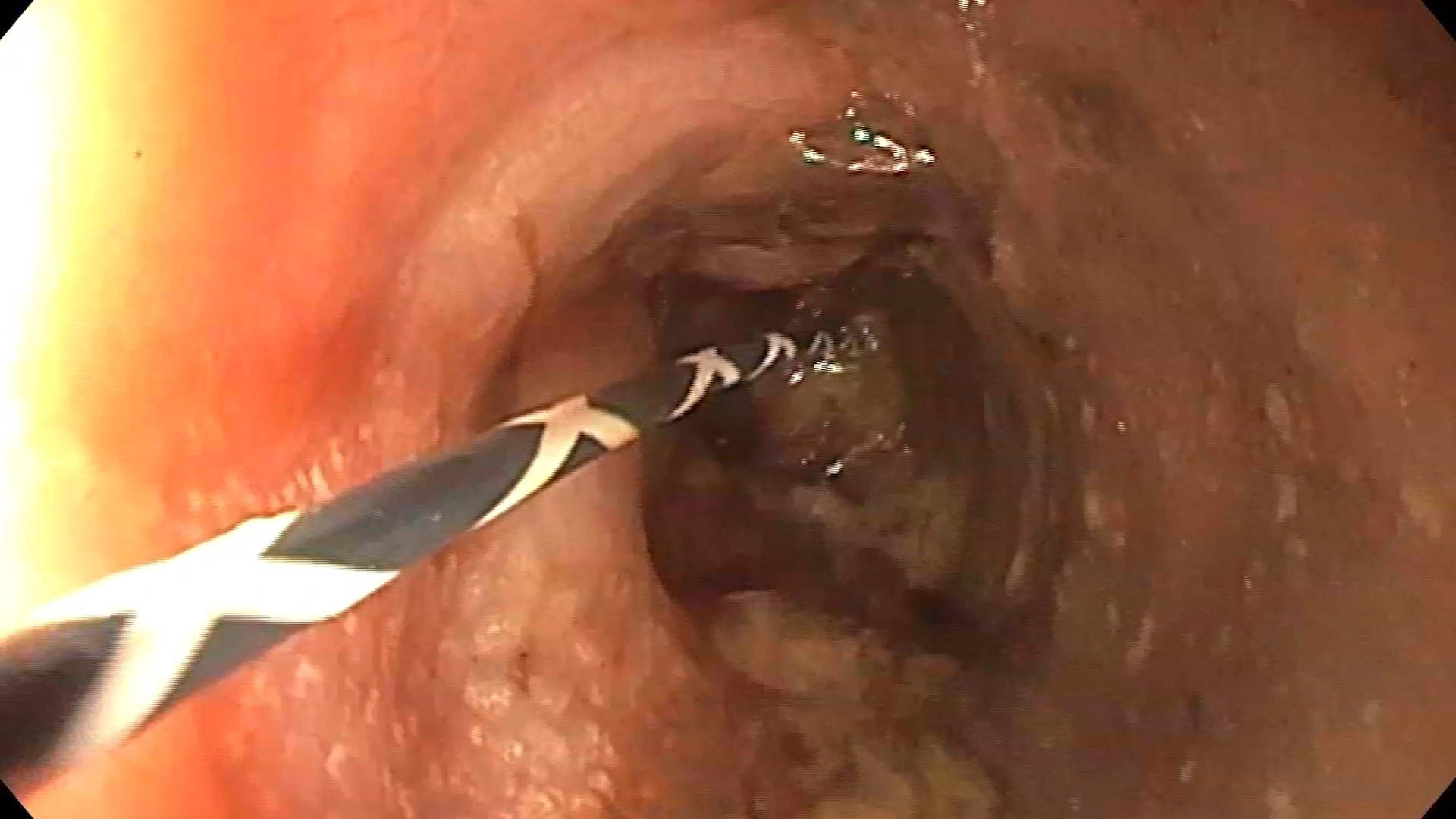
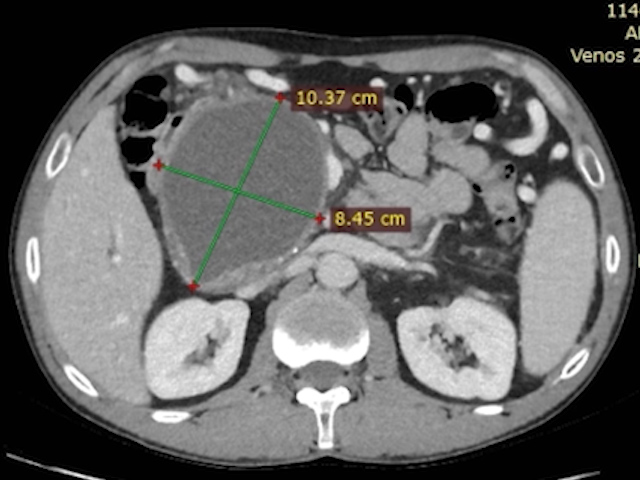
Upper GI endoscopy revealed fresh blood and clots in the stomach; at the level of the fornix a blood vessel with active pulsating bleeding is visualized, without identifying any ulcer. A diagnosis of gastric Dieulafoy lesion was established and an elastic ligature was placed with effective definitive hemostasis.
Upper gastrointestinal bleeding from gastric Dieulafoy lesion.
The case illustrates the endoscopic appearance and management of a rare cause of gastrointestinal bleeding—the Dieulafoy lesion. This is a vascular anomaly characterized by the presence of a persistently enlarged submucosal artery that does not narrow as it approaches capillarization and protrudes through a small mucosal defect. The exact mechanism that causes bleeding is unclear. It can be caused by the pressure that the vascular pulsations exert on the epithelium, with the appearance of a small mucosal defect, localized ischemia and the exposure of the vessel to the digestive contents, with consequent rupture in the lumen. Another possible explanation is the occurrence of thrombosis and subsequent necrosis, followed by its rupture. The lesion can occur anywhere in the digestive tract, but the typical location is in the vertical portion of the stomach, especially at the lesser curvature of the stomach. Clinically, digestive bleeding from a Dieulafoy lesion is typically intermittent and painless, often significant (sometimes even fatal). The diagnosis is often difficult to establish if the bleeding is not active or if recent stigmata of bleeding (eg, adherent blood clot) are not present due to the small size of the lesion, the absence of a mucosal lesion and the intermittent nature of the bleeding. The methods of endoscopic hemostasis are the conventional ones – injection, mono- or bipolar electrocoagulation, placing hemostatic clips and elastic ligatures, without a consensus regarding the optimal modality. In some cases refractory to endoscopic therapy, angiography and surgery are necessary to achieve hemostasis.
1. Jeon HK, Kim GH. Endoscopic Management of Dieulafoy’s Lesion. Clin Endosc 2015; 48: 112-20.
2. Wang Y, Bansal P, Li S, Iqbal Z, Cheryala M, Abougergi M. Dieulafoy’s lesion of the upper GI tract: a comprehensive nationwide database analysis. Gastrointestinal Endoscopy 2021; 94: 24-34.