See other cases
Chronic pseudotumoral pancreatitis
A 35-year-old man, smoker and chronic alcohol user, recently diagnosed with chronic pancreatitis, with at least 2 episodes of acute pancreatitis in the past, presents for clinical and imaging reevaluation, complaining of intermittent pain in the upper abdomen.
Clinical: good general state, underweight (BMI = 17.6 kg/m2), hemodynamically stable, supple but painful abdomen.
Biological: mild leukocytosis with neutrophilia, Hb = 12.7g/dL, slight iron deficiency (sideremia = 59 microg/dL), lipasemia 3.5 x normal values; CA19-9 within normal limits.
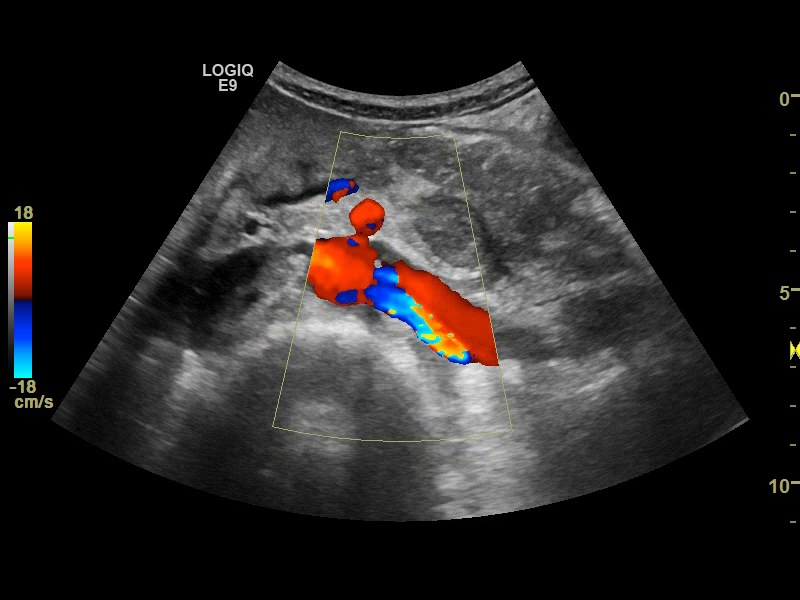
Abdominal ultrasound – inhomogeneous pancreas, with calcifications; at the pancreatic tail, an inhomogeneous, imprecisely delimited tumor of about 35 mm is observed, with a central hypoechoic area; posterior to this, the splenic vein appears obstructed either by extrinsic compression or by in situ thrombosis.
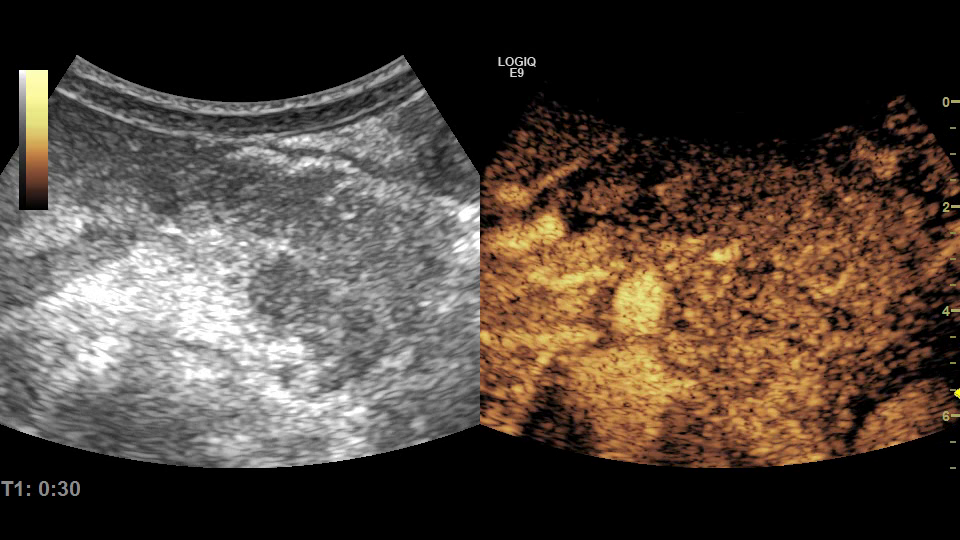
Contrast-enhanced ultrasound (CEUS) – the pancreatic tail tumor shows enhancement in the arterial phase and discrete wash-out in the venous phase. The possibility of a neuroendocrine tumor was also discussed.
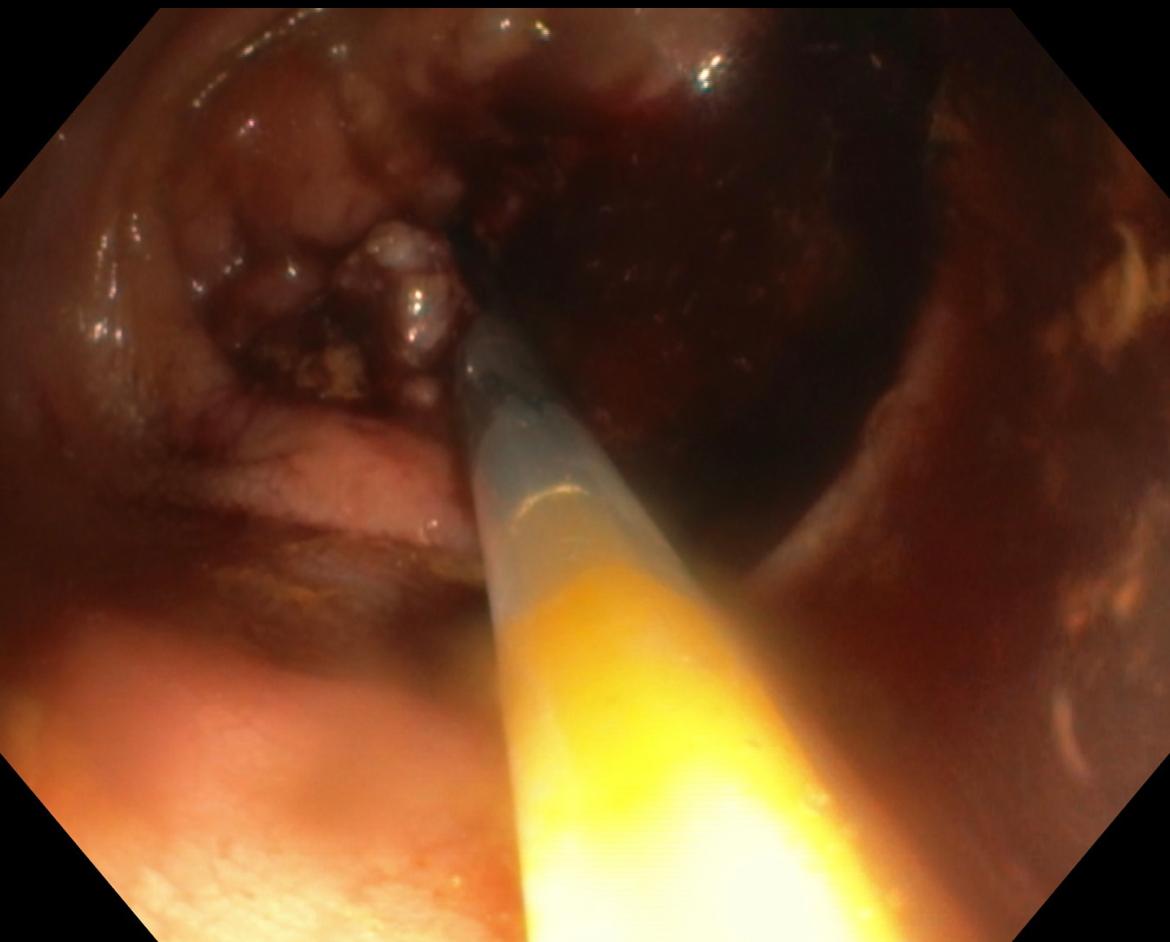
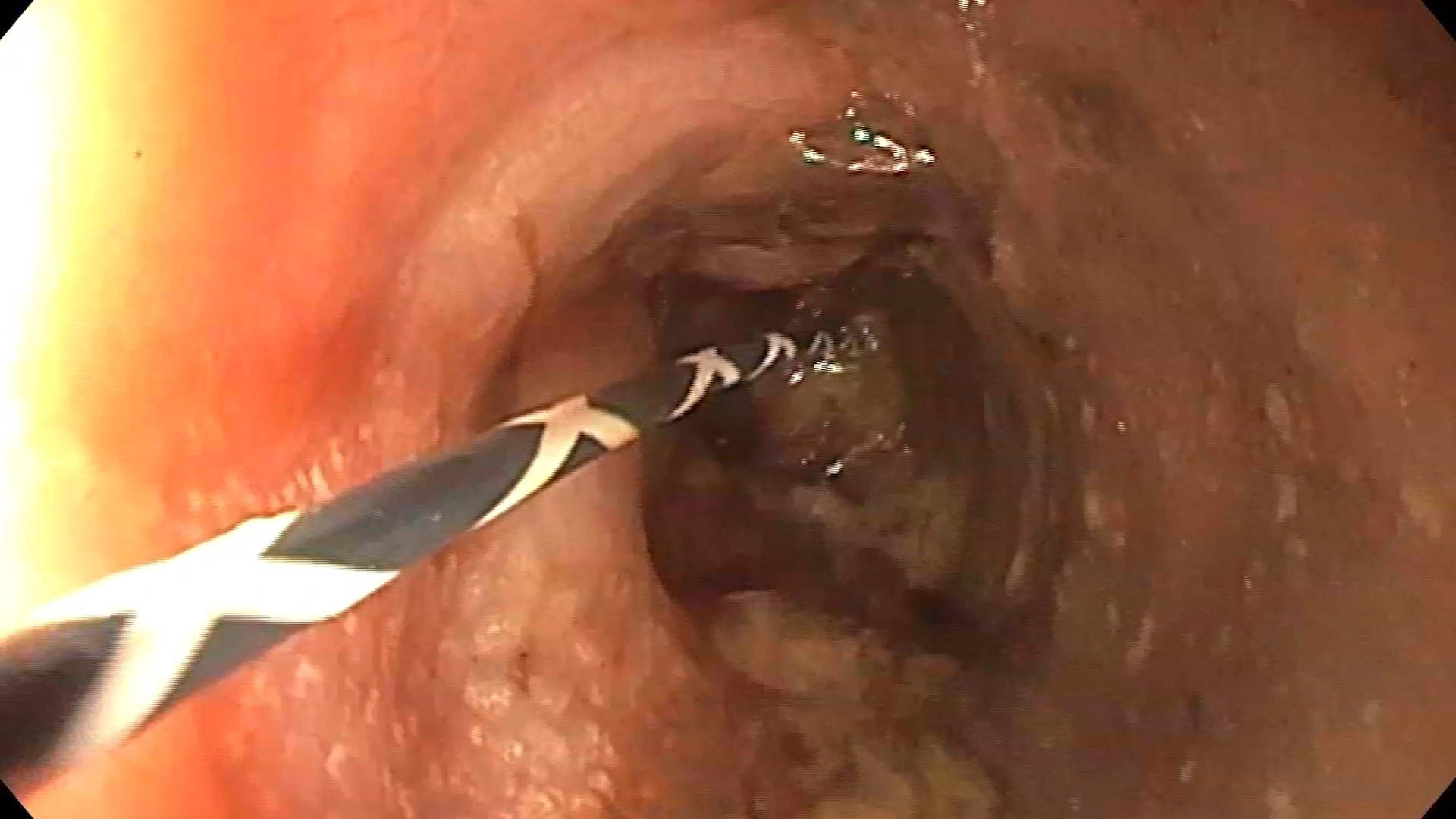
EUS-FNA – highlights the imprecisely delimited, intensely inhomogeneous caudal lesion, without Doppler signal, from which biopsies are taken.
Cytological and microhistological examination: no definite malignancy criteria on the examined material.
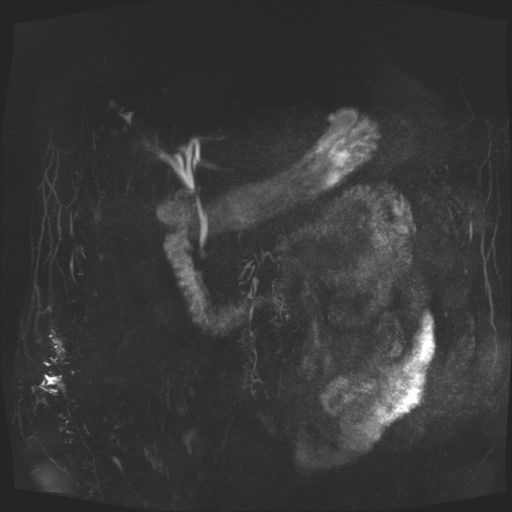
Abdominal CT with contrast performed showed the same appearance of inhomogeneous pancreas, with calcifications, pseudotumorally enlarged in the body and tail of the pancreas, with visualization of the contrast in the distal portion of the splenic vein, which appears more slender and with collateral circulation at this level.
Chronic pseudotumoral pancreatitis. Splenic vein stenosis.
Conventional imaging methods (ultrasound, abdominal CT with contrast, MRI) are used to identify pancreatic tumoral lesions, invasion into adjacent structures and metastases, but in patients with chronic pancreatitis the examination is difficult due to the morphological changes of the pancreas.
Pancreatic neuroendocrine tumors are relatively rare entities, especially in association with chronic pancreatitis. The characteristic of neuroendocrine tumors is the rich vascularity, which leads to hyperennhancement in the arterial phase, as in the present case, in contrast to pancreatic adenocarcinomas, which are characterized by imprecise contour delineation and reduced enhancement in all phases on contrast examination.
EUS with FNA biopsy has superior sensitivity and specificity for establishing the diagnosis. In patients with chronic pancreatitis, however, there may be difficulties in distinguishing between pseudotumoral inflammation and malignancy. Also, cellular atypia in chronic pancreatitis is sometimes difficult to distinguish from those found in pancreatic adenocarcinoma.
As a consequence of the chronic inflammatory process, the patient also developed splenic vein stenosis, an entity that occurs in 10-40% of patients with chronic pancreatitis. The diagnosis can be established by non-invasive imaging methods (ultrasound, CT, MRI, EUS). In the present case, the stenosis was difficult to diagnose sonographically (including by CEUS and Doppler examination), with CT and EUS examination establishing the final diagnosis.
The particularity of the case is represented by the young age of the patient, recently diagnosed with chronic pancreatitis, in which a pseudotumoral lesion with possible criteria of malignancy was discovered on contrast examination, suggestive of a neuroendocrine neoplasia. EUS revealed an imprecisely delimited lesion, with minimal Doppler signal, aspects rather suggestive of a pancreatic adenocarcinoma. EUS-FNA ruled out the suspicion of malignancy, finally establishing the diagnosis of chronic pseudotumoral pancreatitis with splenic vein stenosis, and the subsequent clinical evolution was favorable.
1. Hart PA, Conwell DL Chronic Pancreatitis: Managing a Difficult Disease. Am J Gastroenterol 2020; 115: 49-55.
2. Grassia R, Imperatore N, Capone P et al. EUS-guided tissue acquisition in chronic pancreatitis: Differential Diagnosis between pancreatic cancer and pseudotumoral masses using EUS-FNA or core biopsy. Endosc Ultrasound 2020; 9: 122–129.
3. Khanna L, Prasad SR, Sunnapwar A et al. Pancreatic Neuroendocrine Neoplasms: 2020 Update on Pathologic and Imaging Findings and Classification. Radiographics 2020; 40: 1240-1262.