See other cases
A 58-year-old female with a history of acute biliary necrotizing pancreatitis 6 months ago, complicated by the development of a peripancreatic necrotic fluid collection, increasing in size on consecutive imaging, presents with abdominal pain, loss of appetite, early satiety and weight loss about 5 kg/6 months, with progressive worsening of symptoms.
Clinical – palpable, painful epigastric mass.
Biological – hyperamylasemia, marked hyperlipasemia (2.5 x, and 33 x the upper limit of normal, respectively), minimal inflammatory syndrome, abnormal glycemia (fasting blood glucose 118 mg/dL, HbA1c 6.2%), CA 19-9 within normal limits.
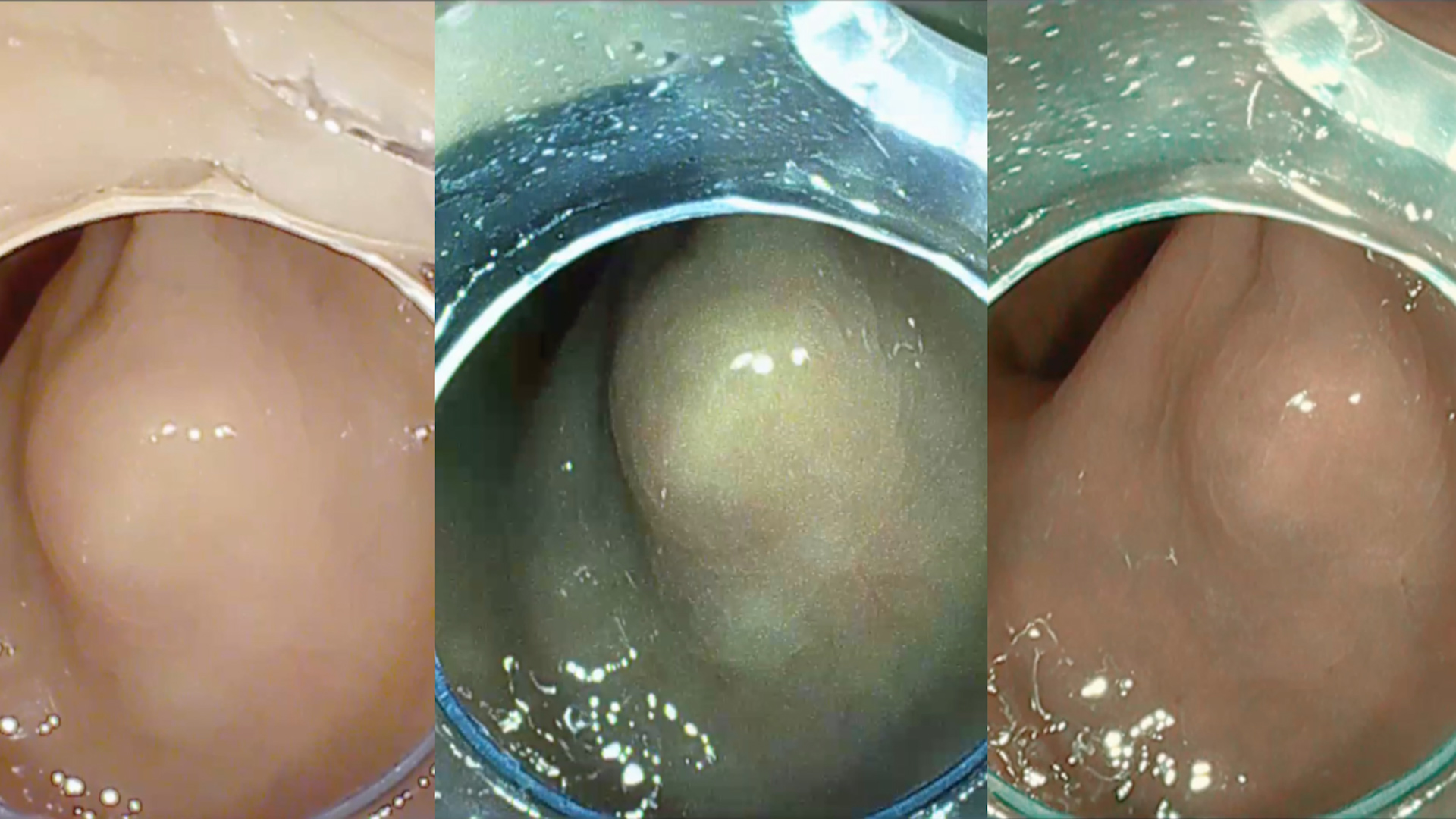
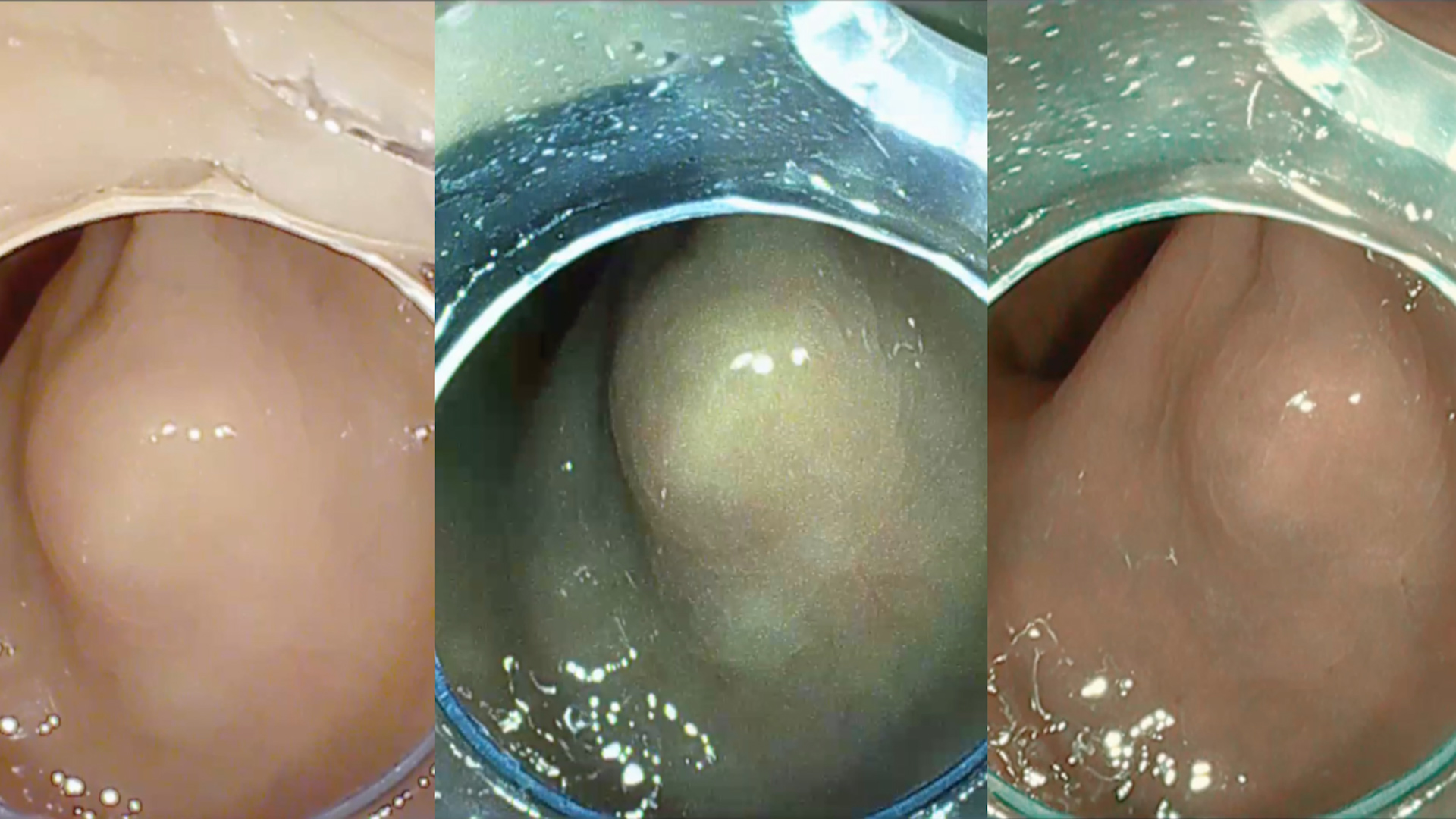
Abdominal ultrasound reveals a 10/9/7 cm fluid collection with hyperechoic debris, located in the body-tail pancreatic area. Computed tomography (CT) reveals dimensional progression of the well-defined, inhomogeneous peripancreatic collection, suggestive of WOPN (walled-off pancreatic necrosis).
Walled-off pancreatic necrosis (WOPN). Considering the necrotic content ~ 30% it was decided for endoscopic ultrasound-guided drainage with HotAxios 10/15 mm luminal apposition metal stent (LAMS). A favorable postprocedural evolution was noted, with regression of the collection 4 weeks after drainage, when stent extraction was performed. 3-month follow-up revealed an asymptomatic patient with good appetite and remission of glycemic abnormalities.
About 40% of acute pancreatitis cases are complicated by the development of peripancreatic fluid collections, most of which resolve spontaneously. About 15% of them mature and progress to the formation of pseudocysts or WON.
Patients’ history, along with the morphological evaluation of the cystic lesion, as well as of the rest of the pancreatic parenchyma, are important clues for the differential diagnosis with a pancreatic cystic neoplasm, which may present as acute pancreatitis.
Once the diagnosis of peripancreatic fluid collection is established, drainage should be delayed for at least 4 weeks after the acute pancreatitis onset, as before this interval the wall of the collection is immature.
Evaluation of a collection involves cross-sectional imaging to assess the topography and size of the lesion, the presence and extent of necrosis and exclusion of a pseudoaneurysm. Magnetic resonance imaging is superior to computer tomography for assessing the necrotic content of the collection and its connection to the ductal system or the presence of interrupted pancreatic duct.
Drainage is indicated for symptomatic (persistent abdominal pain, vomiting, weight loss) or complicated lesions (infected or mass-effect on the upper digestive tract or biliary tree).
Drainage can be performed transpapillary (for collections located in the head of the pancreas, which communicate with the Wirsung duct) or transmural – with plastic or metal stents. Luminal apposition metal stents (LAMS) are preferred over plastic stents for WOPN drainage due to their larger caliber, high clinical success rate, and the possibility of performing necrosectomy. In the case of multiple/multiloculated collections with a difficult approach, drainage can be performed using combined endoscopic + percutaneous techniques and possibly the use of multiple stents (multigateway approach), to optimize drainage and reduce the risk of infection of remaining collections.
Minimally invasive endoscopic, percutaneous, or combined drainage procedures are currently the standard of care for the management of peripancreatic or intraabdominal post-acute pancreatitis symptomatic or complicated collections. It is noticeable the resolution of glycemic abnormalities after drainage of the collection in the presented case.
See other cases