See other cases
Aorto-enteric fistula
A 84-year-old patient with a history of high blood pressure and smoking presented to the emergency room with lower abdominal pain and marked physical asthenia. At the Emergency Department, the patient presented hematochezia.
Clinical: hemodynamically stable, lower abdominal pain with no signs of peritoneal irritation.
Biological: WBC 32700 /microL, hemoglobin=8.1 g/dL, PLT = 321 000 /microL, INR=1.23, creatinine =1.4 mg/dl, Na=136 mmol, K=5.3 mmol, CRP = 292 mg/L, procalcitonin = 2.32 ng/mL.
Given the symptoms, it was decided to urgently perform a CT scan with contrast:
– No contrast extravasation in the digestive tract, instead: infrarenal aortic aneurysm (130 mm cranio-caudal), with parietal thrombus, cuffed by a collection suggestive of a retroaortic abscess
– The aneurysm + the collection formed a forceps that almost completely stenoses the inferior vena cava; superior mesenteric artery with severe atheroma and thready flow.
A vascular surgery consultation was initially performed: no surgical indication at the moment and admission to the gastroenterology department was decided. Emergency upper GI endoscopy revealed a large adherent clot in the fornix and stasis fluid (penetrating to approx. 5-6 cm of D2). A 60 cm rectosigmoidoscopy was also performed: mucosal lesions compatible with the diagnosis of ischemic colitis.
Paraclinical reevaluation after 12 h: WBC = 26 000 /microL, hemoglobin = 7.1 g/dL
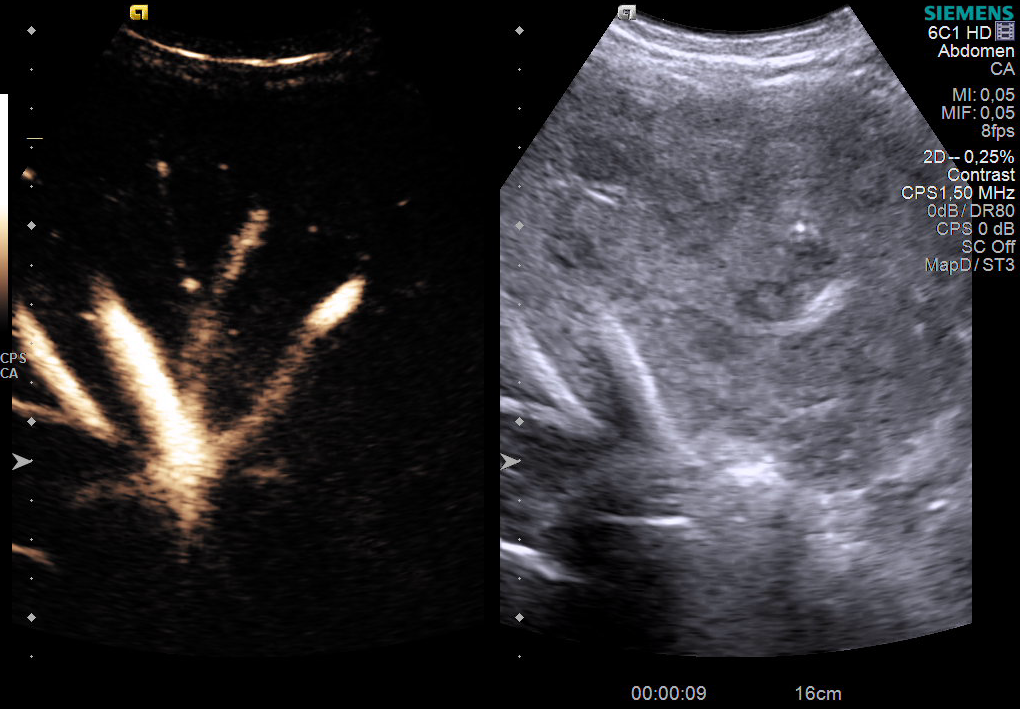
Taking into consideration that the source of the upper bleeding was uncertain: re-evaluation of the CT scan images showed the absence of the demarcation line between the inferior duodenal angle and the aneurysmal wall, with the suspicion of a possible aorto-duodenal fistula (Figure 2 + 3).
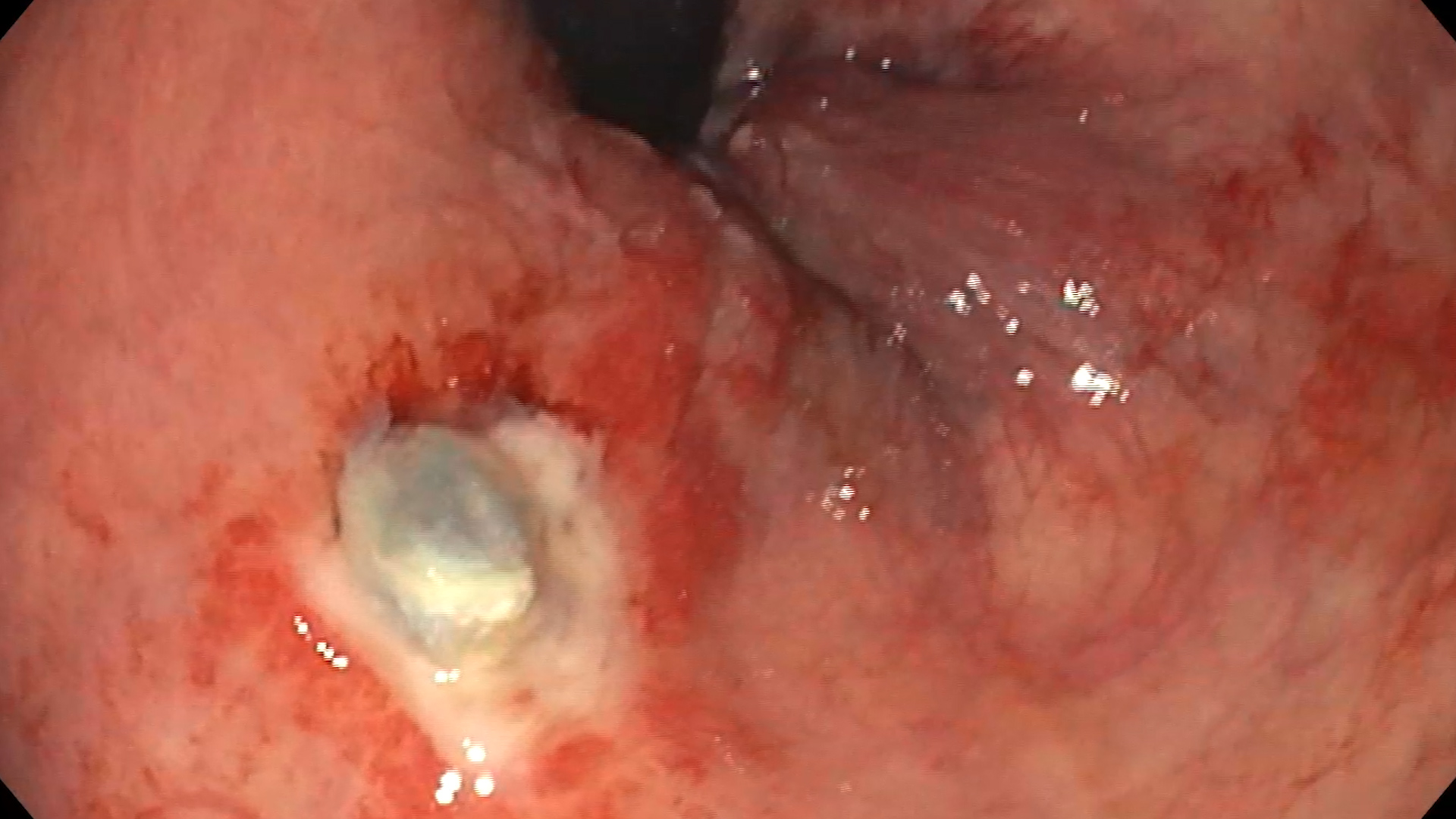
Upper GI endoscopy after 12 h: a clot at the level of the fornix, with no underlying lesion; gastric mucosa was lined with fresh blood; the bulb and D2 appeared covered with fresh blood. On withdrawal, an infrapapillary lesion suggestive for an aorto-enteric fistula was visualized with difficulty. It was re-examined with the duodenoscope that revealed the lesion: erosion with a diameter of approx. 10-12 mm with a deep punctate hole – in the clinical and imaging context, most likely aortoenteric fistula (Figure 1).
The patient was transfered to the cardio-vascular surgery section, Fundeni Clinical Institute. Emergency surgery was performed to remove the aneurysm of the infrarenal abdominal aorta and the fistula, double-layer duodenorrhaphy and aorto-aortic interposition of a silver Dacron prosthesis (Figure 4).
Aortoenteric fistula is a rare cause of frequently fatal gastrointestinal bleeding, difficult to diagnose. Mortality is approximately 77% with treatment and 100% without treatment. Most often the fistula occurs at the duodenal level. Aortoenteric fistulas are of 2 types:
1. Primary: most often an aneurysm with compression of the digestive tract, tumors, foreign bodies, radiotherapy
2. Secondary (most common): erosion after aortic graft
The particularity of the case was represented by the rare cause and the difficult diagnosis of the upper digestive hemorrhage through the aortoenteric fistula. The approach and treatment required a multidisciplinary team and good cooperation / coordination between the different departments for a fast and effective treatment, often this complication of the aneurysm being fatal.
The patient was discharged after 17 days with a good general condition.
1.Yang Y, Hu D, Peng D. Primary aortoesophageal fistula: a fatal outcome. Am J Emerg Med 2018; 36: 343.e1–343.e3.
2.Saers SJ, Scheltinga MR. Primary aortoenteric fistula. Br J Surg 2005; 92: 143–152.