See other cases
A rare case of pancreatic schwannoma diagnosed preoperatively by EUS-FNB
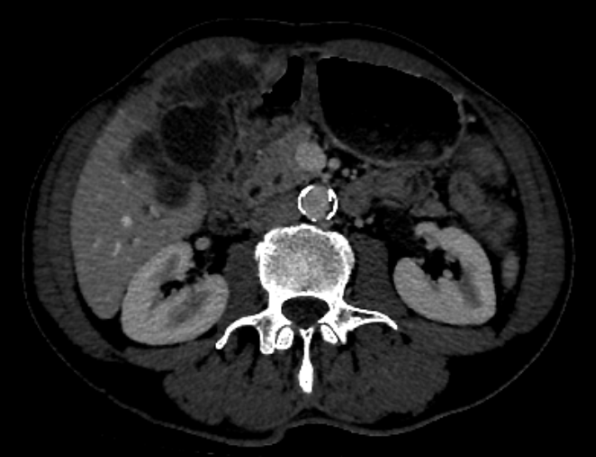
We present a 54-year-old patient which was evaluated for an enlarged “retroperitoneal” lymph node depicted on cross-sectional imaging (contrast-enhanced CT).
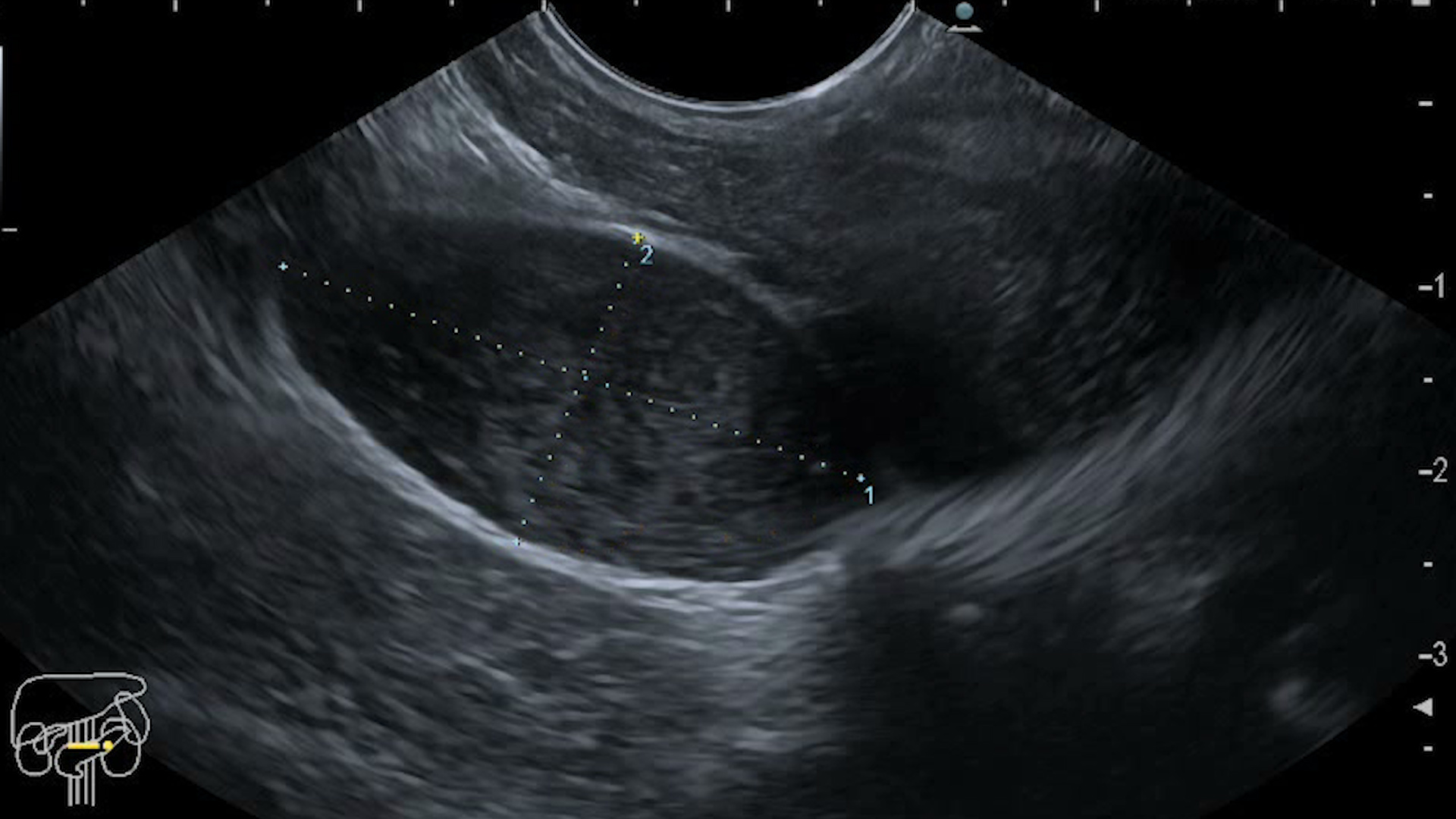
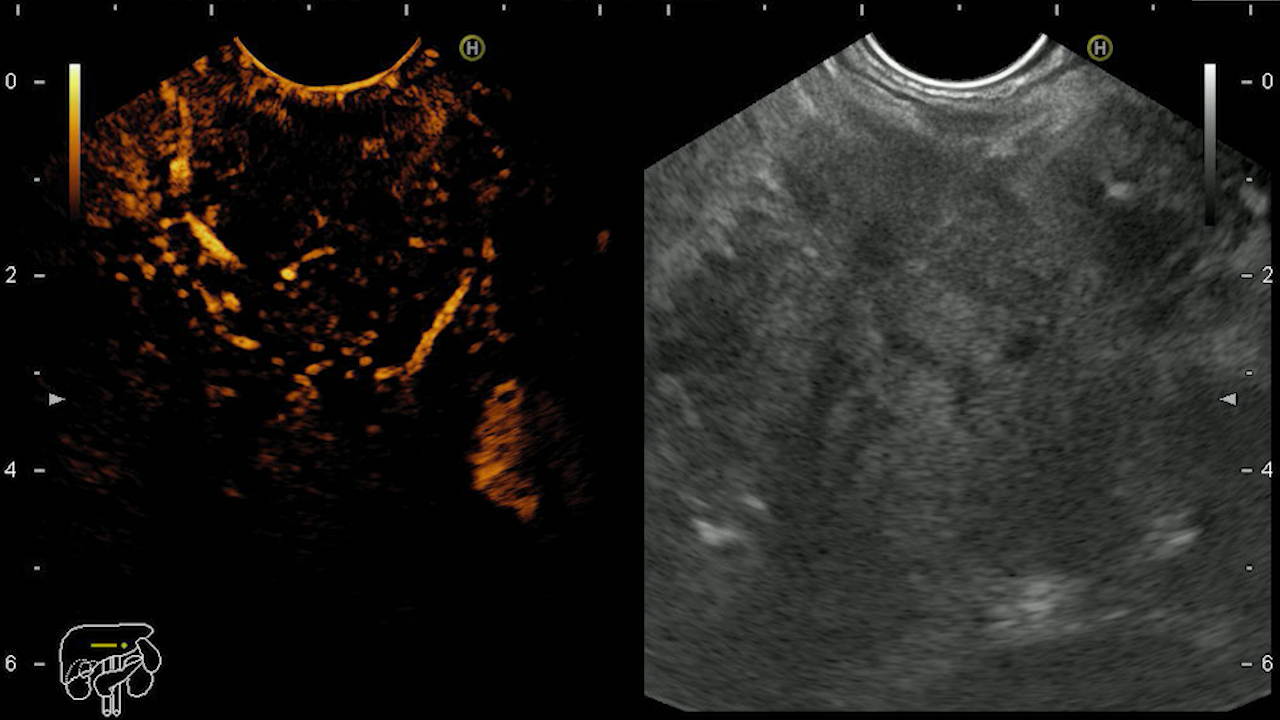
Initial gray-scale EUS examination depicted a 3.4 x 1.8 cm hypoechoic lesion, encapsulated, with slight heterogenous content, located on the posterior side of the pancreas, in close proximity of the pancreatic head, superior mesenteric vein and artery.
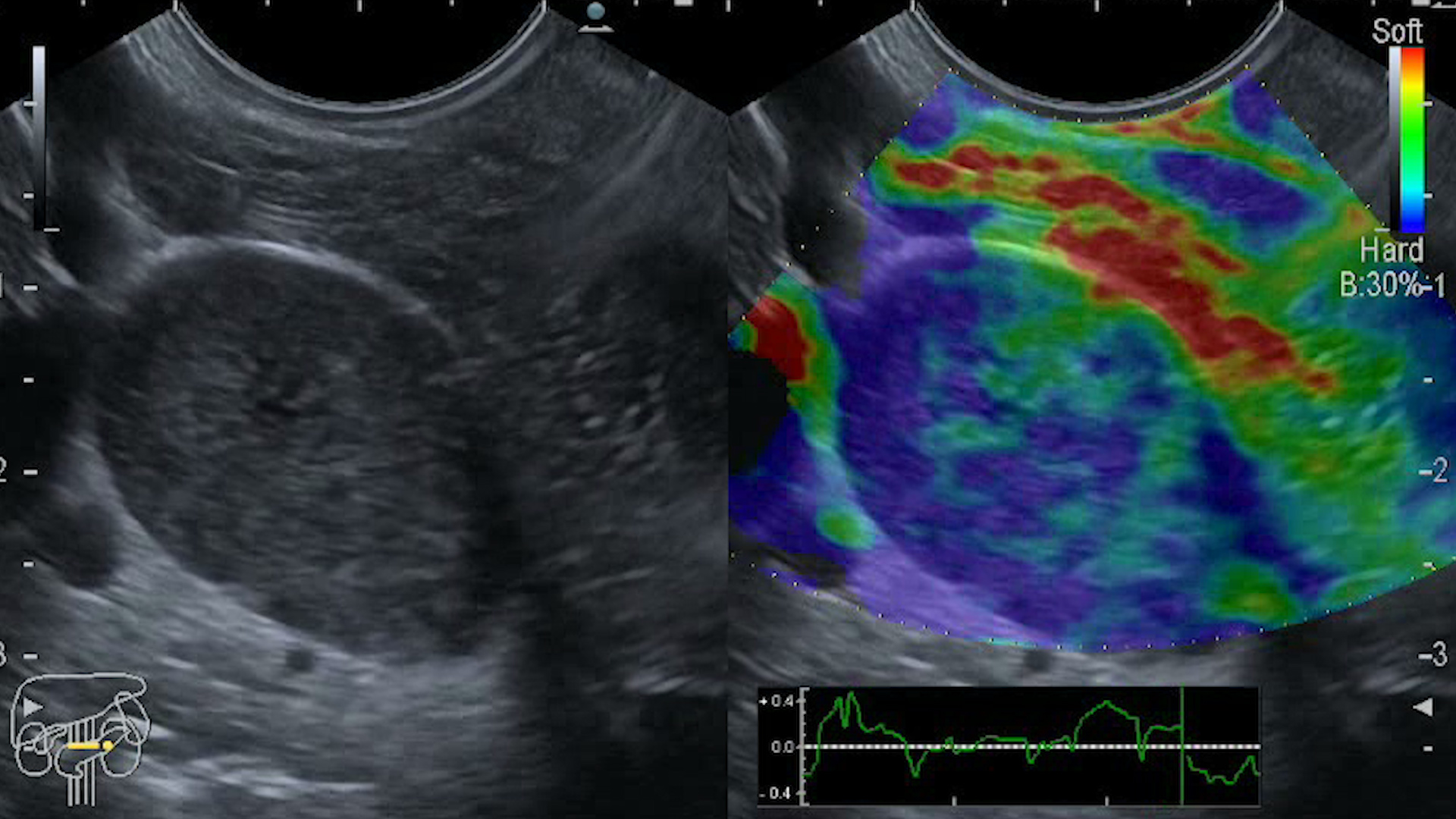
EUS elastography showed a low-strain (hard, non-compressible) focal pancreatic mass.
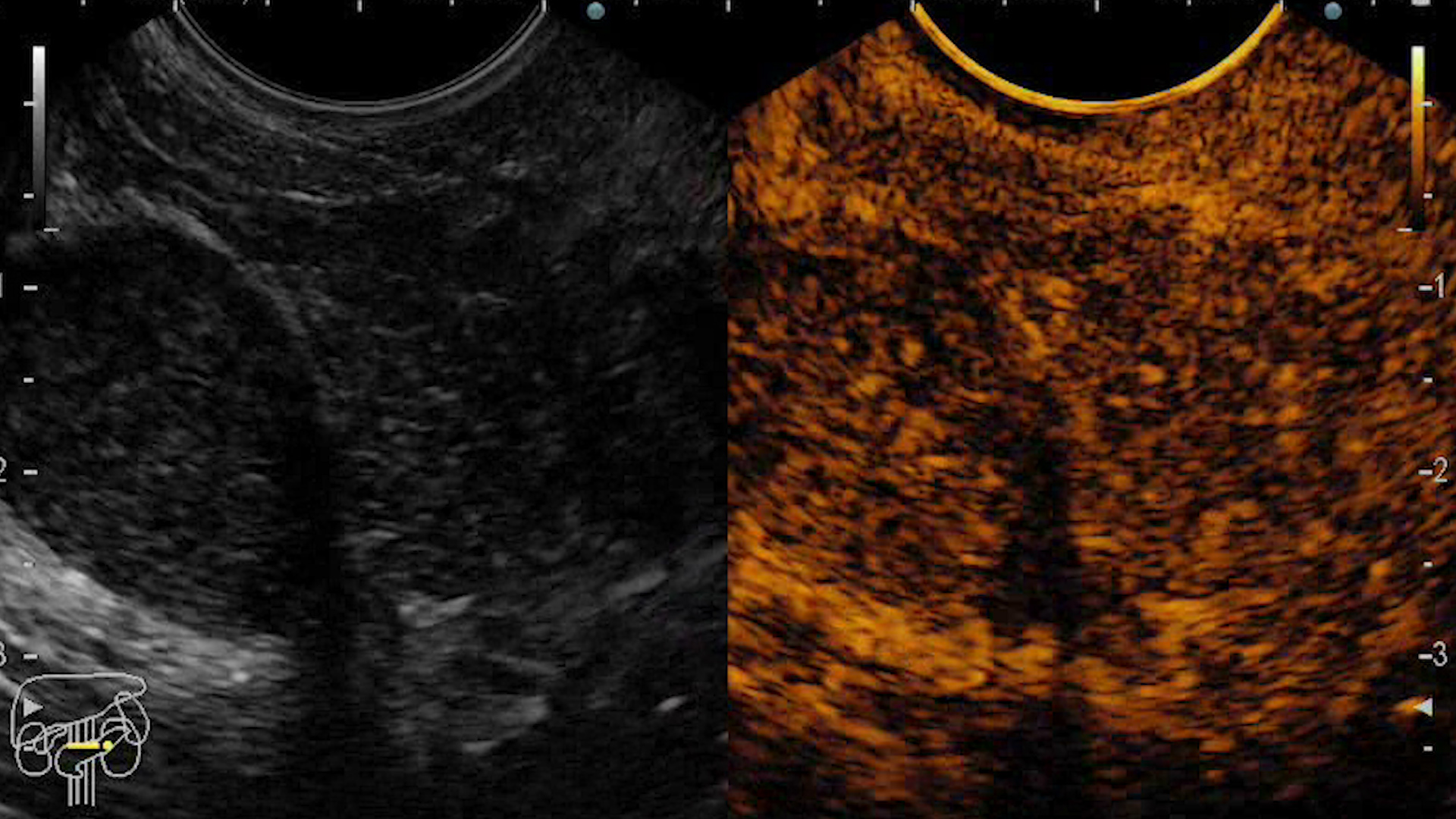
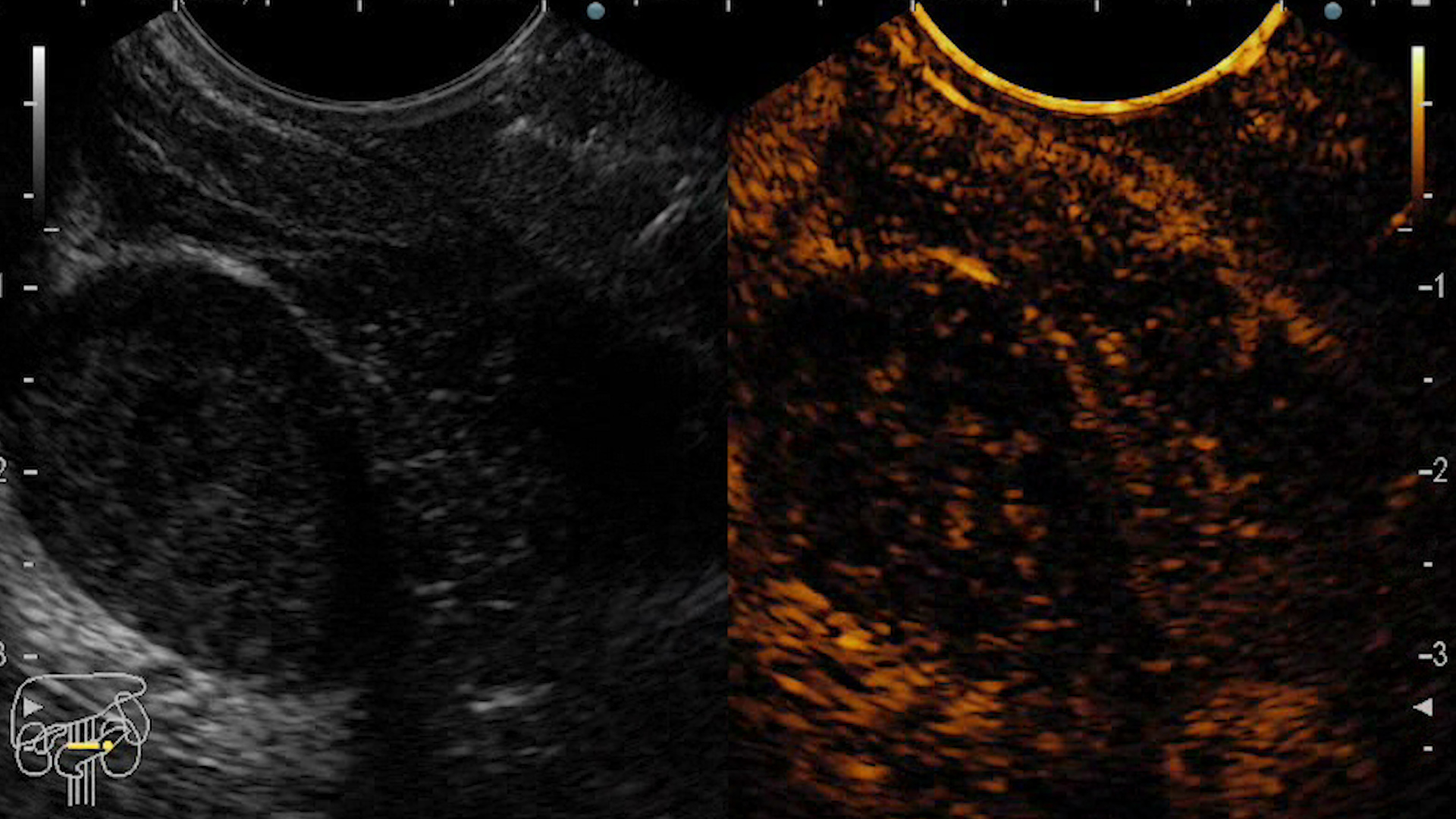
Contrast-enhanced EUS showed arterial hyperenhancement, followed by wash-out in the venous phase.
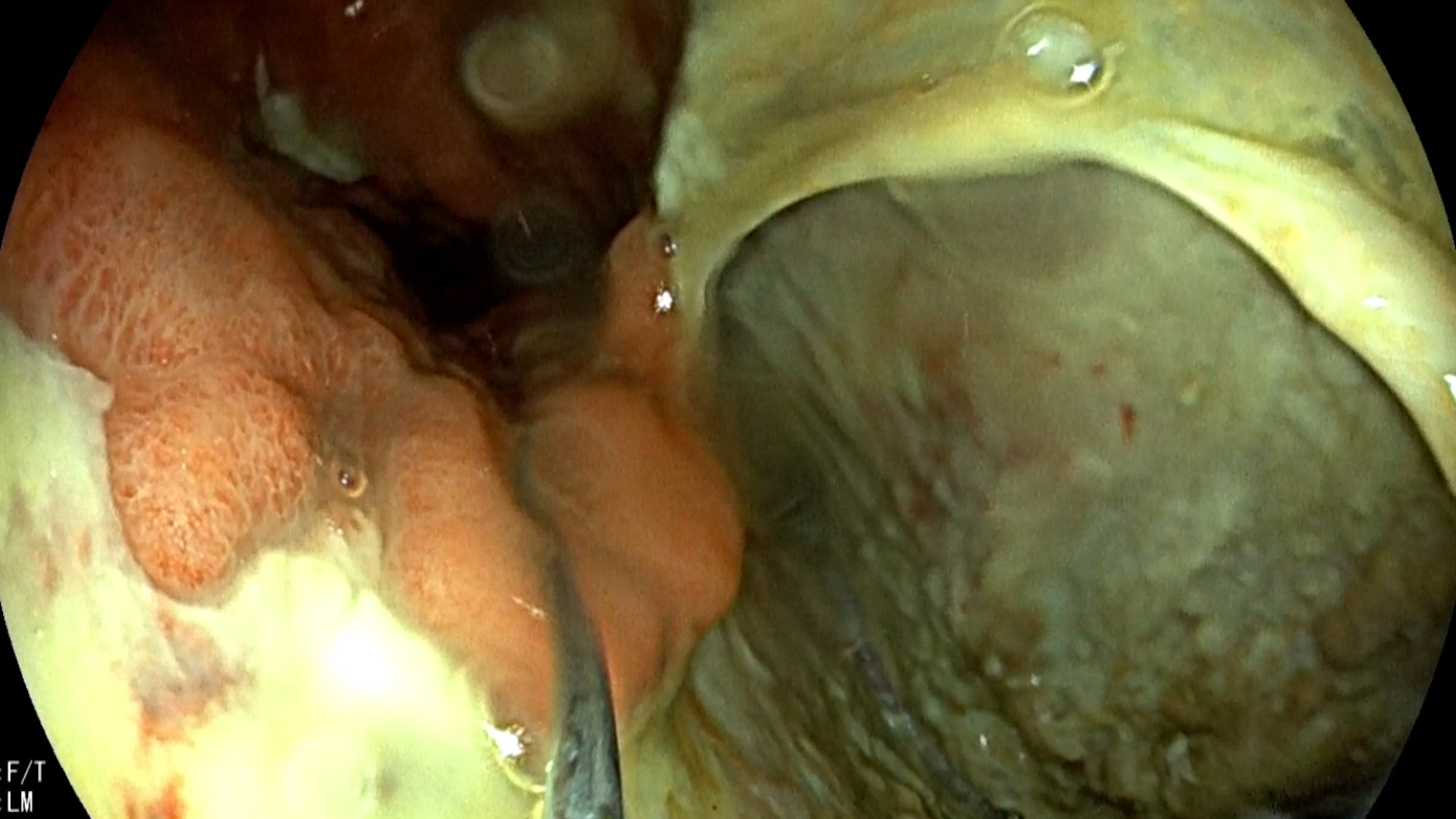
EUS-guided fine needle biopsy (FNB) was further performed showing a decreased acinar pancreatic tissue, with fragments of spindle cells testing positive S-100 & SOX-10, and negative for CK AE1/AE3, DOG1 & synaptofisine imunohistochemical stains. The ki-67 proliferation index of less than 5%.
Pancreatic schwannoma.
Pancreatic schwannoma is a rare tumor (over 100 cases described in the literature), being the most common peripheral nerve sheath tumor. Although benign, it can have malignant potential, especially if large. Furthermore, tumors are variable in size and might undergo degenerative changes, characterized by cyst formation, calcification, hemorrhage, hyalinization, as well as xanthomatous infiltration [1]. Imaging diagnosis by cross-sectional methods (CT and/or MR imaging) is thus non-specific, showing a low-attenuation lesion on CT with a clearly defined capsule on MR [2]. The diagnosis was confirmed by EUS-guided FNB, followed by pathology exam [3]. Although the diagnosis confirmed a benign schwannoma, the decision after a multidisciplinary meeting was to further refer the patient for surgical excision (enucleation) of the mass in view of the malignancy risk.
EUS elastography and contrast-enhanced EUS are useful methods to guide EUS-FNB for confirmation of the diagnosis of schwannoma. Pathology diagnosis is essential in these rare pancreatic tumors to decide on the risk of malignancy. An informed evidence based decision for the management of these patients should be reached in a multidisciplinary tumor board, including also the patient opinion.
- Ntafam C, Miller AT, Beutler BD, Bamporiki J, Sahakian AB, Cheng PM. Pancreatic schwannoma: Case report, clinico-pathologic correlation, and review of the literature. Radiol Case Rep 2022 Jul 27;17(10):3504-3510.
- Aichouni N, Abbou W, Nasri S, Khannoussi W, Ismaili MZ, El Harroudi T, Bennani A, Kamaoui I, Skiker I. Pancreatic schwannoma- CT and MRI findings: A rare case report and review of literature. Ann Med Surg (Lond) 2021; 68: 102664.
- Hanaoka T, Okuwaki K, Imaizumi H, Imawari Y, Iwai T, Yamauchi H, Hasegawa R, Adachi K, Tadehara M, Kurosu T, Watanabe M, Tamaki A, Kida M, Koizumi W. Pancreatic Schwannoma Diagnosed by Endoscopic Ultrasound-guided Fine-needle Aspiration. Intern Med 2021; 60(9): 1389-1395.