See other cases
A gastroenterological riddle: navigating severe anemia with immunological surprises
A 67-year-old male patient presented to the ER with intense fatigue and shortness of breath. He was soon diagnosed with severe anemia, denying any kind of known or visible bleeding. He also stated that this anemia has a long, known evolution of about 10 years, for which he performed multiple investigations in the distant history, but without finding out the cause.
Clinical: fatigue and shortness of breath, the patient denies any other symptoms.
Biological: severe normocytic anemia (Hb: 6g/dL), abnormal liver blood tests (AST and ALT 2-3 times the normal value).
During the hospitalization, the patient needed several blood transfusions.
After the patient was stabilized, both a gastroscopy and colonoscopy were performed.
Colonoscopy: everything was normal, no direct or indirect signs of bleeding were noticed.
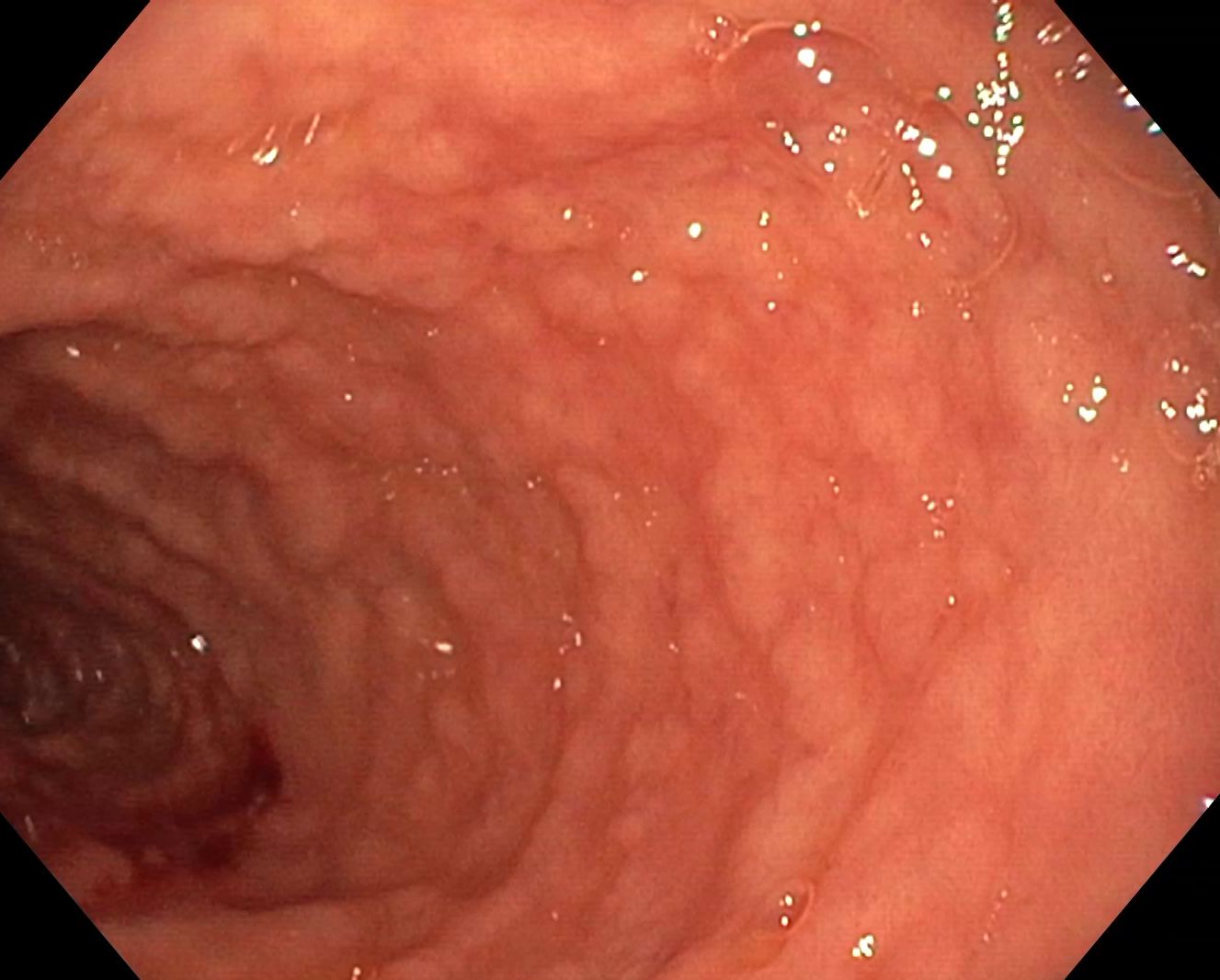
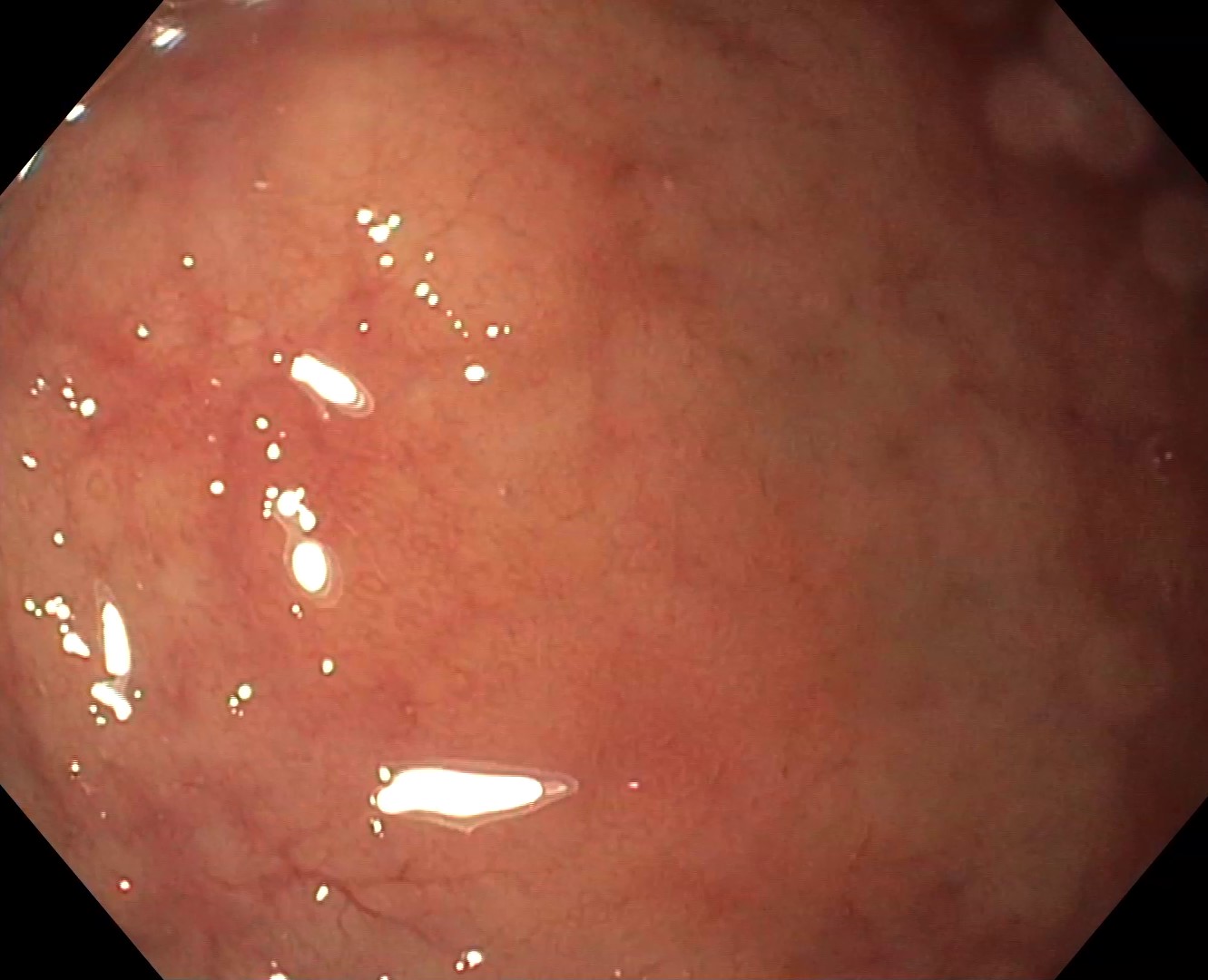
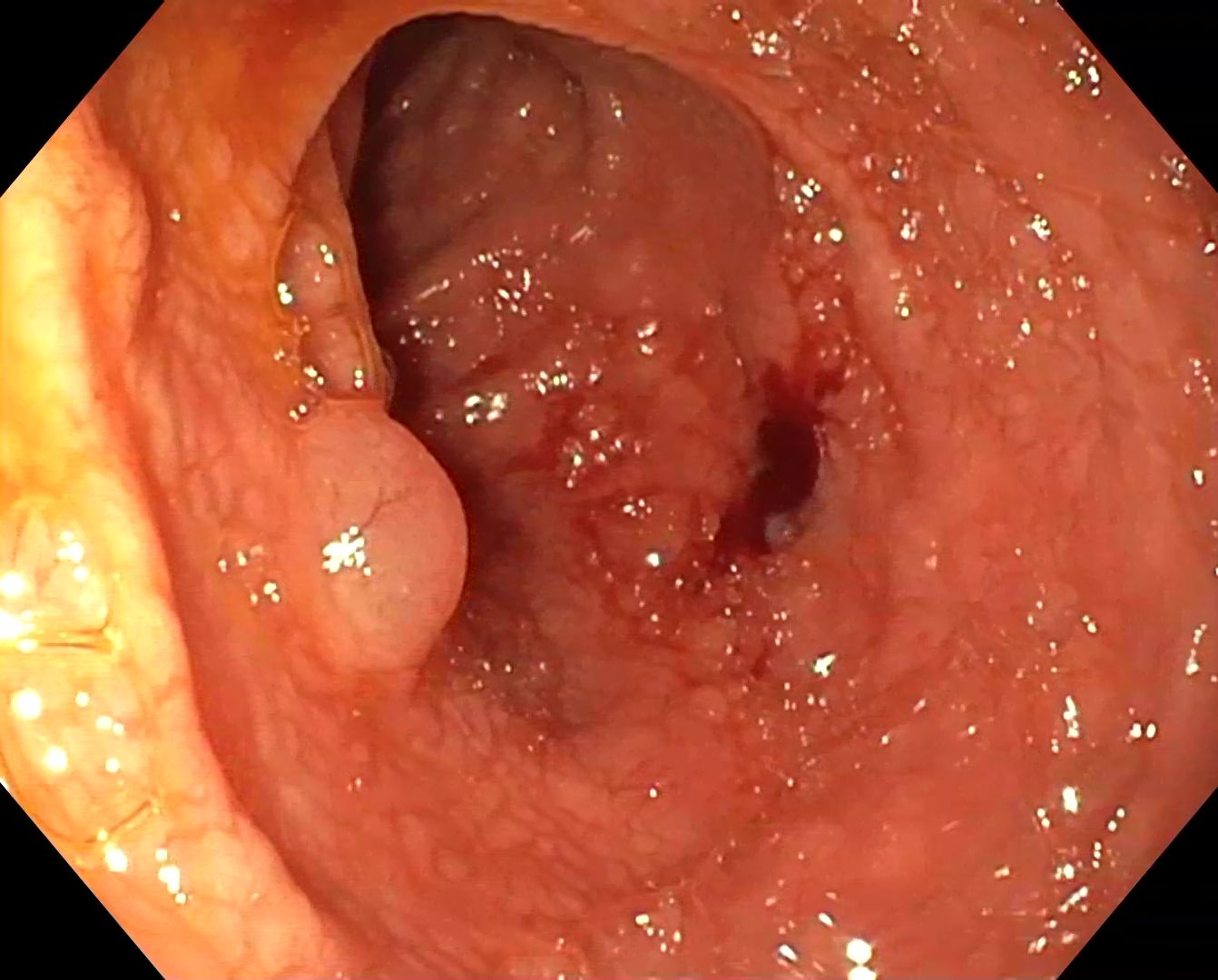
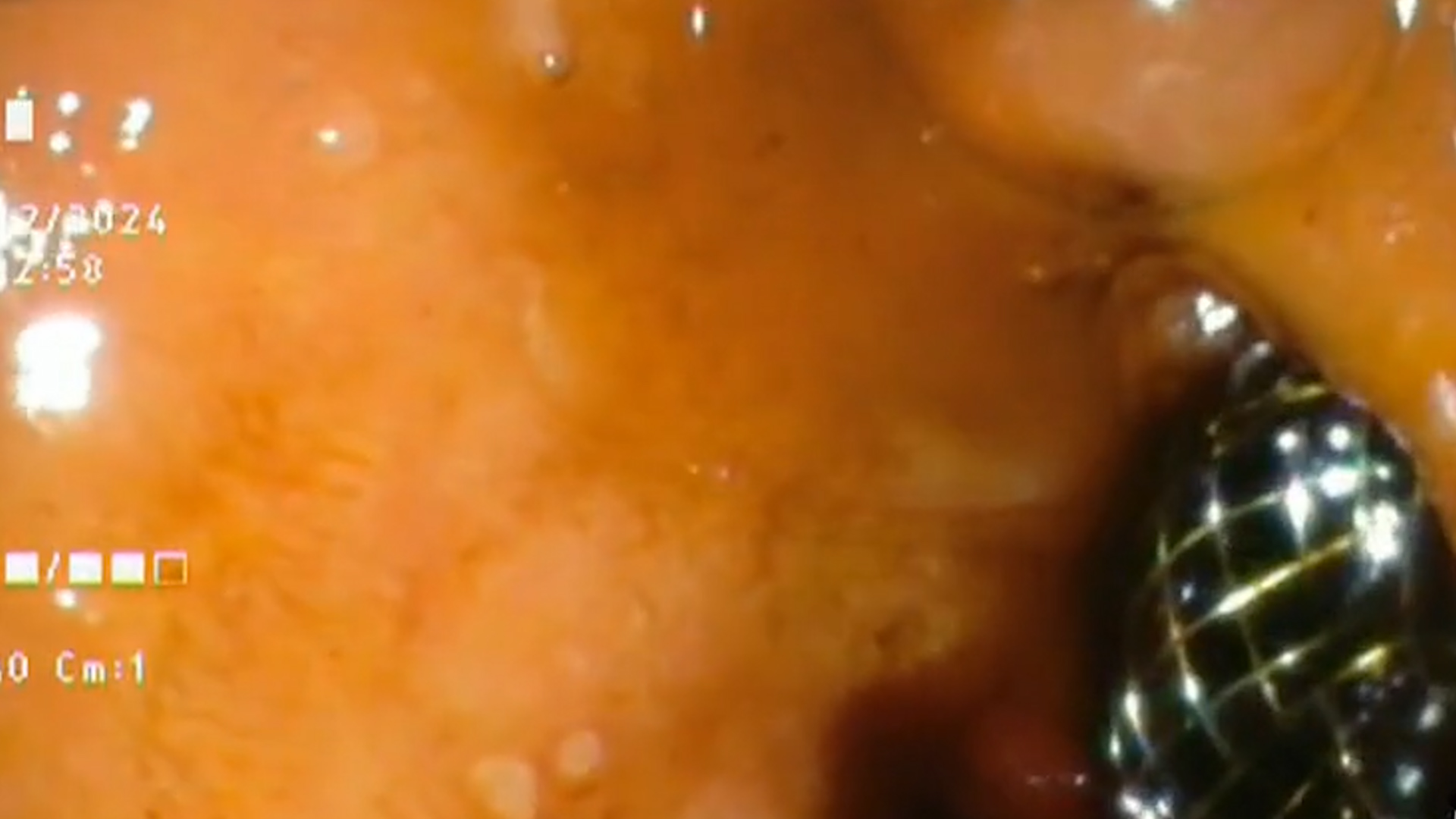
Gastroscopy: in the D2 (Figure 1) and D1 (Figure 2) duodenum we noticed an important villous atrophy, scalloping of the duodenal folds as well as decreased folds, and pneumatosis intestinalis (Figure 3).
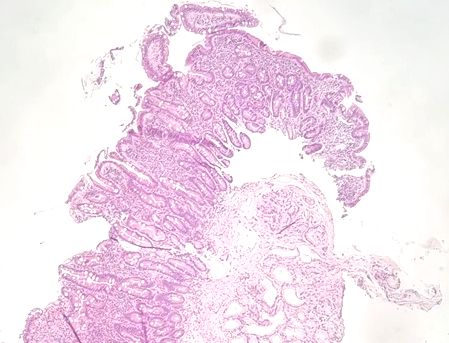
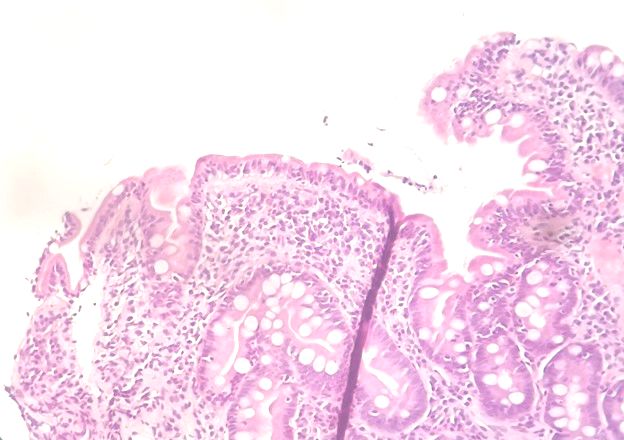
The biopsies taken from the D2 and D1 duodenum revealed (Figure 4 and 5): villous atrophy, lamina propria inflammation and intraepithelial lymphocytosis.
Serological tests for celiac disease came back negative: anti tTG IgA antibodies, anti-endomysial IgA antibodies and the antigliadin antibodies IgA.
A more complete serology panel was ordered: serological total IgA < 5 mg/dL (normal range 101-645 mg/dL), tTG antibodies IgG 23 U/mL (normal range <10 U/mL; a genetic testing was also performed, that came back positive for HLA DQ2 haplotype.
Celiac disease. Selective IgA deficiency.
An estimated 2% of patients with celiac disease also have a selective IgA deficiency, thus it is important to always screen the patients with probable celiac disease for serological IgA deficiency. 1Thus, the presence of IgA deficiency can lead to an inaccurate negative result on a celiac disease antibody test.
One of the most common extraintestinal manifestations of a celiac disease is anemia. It usually is a multifactorial anemia and that’s why screening for celiac disease in cases of anemia with no apparent cause, might be of use. 2
As there is a notable correlation between celiac disease and pneumatosis intestinalis, further investigation is needed to better understand the clinical implications for patients with these conditions.3
- Chow MD, Lebwohl B, Reilly NR, Green PHR. Immunoglobulin A Deficiency in Celiac Disease Marisa A. J Clin Gastroenterol 2012;46(10): 850-854.
- Martín-Masot R, Nestares MT, Diaz-Castro J, López-Aliaga I, Alférez MJM, Moreno-Fernandez J, Maldonado J. Multifactorial Etiology of Anemia in Celiac Disease and Effect of Gluten-Free Diet: A Comprehensive Review. Nutrients 2019;11(11):2557.
- Dayal S, Bolton-Jones R, Stallard S, Romics JrL. Extensive Pneumatosis Intestinalis in Association With Celiac Disease: A Case Report. Journal of Medical Cases 2011;2(2):39-43.