See other cases
Radiation Proctitis, a long journey
A 75-year-old male patient with a medical history that includes ligated internal hemorrhoids and prostatic adenocarcinoma presented to the emergency room. His prostatic adenocarcinoma was previously treated with radiotherapy (the last session occurred seven months before symptom onset) and hormonal therapy. He was experiencing persistent rectal bleeding and severe anemia.
Clinical: The patient presented with persistent rectal bleeding.
Biological: Laboratory results revealed severe hypochromic anemia, with hemoglobin measured at 6.2 g/dL. No other significant changes were detected
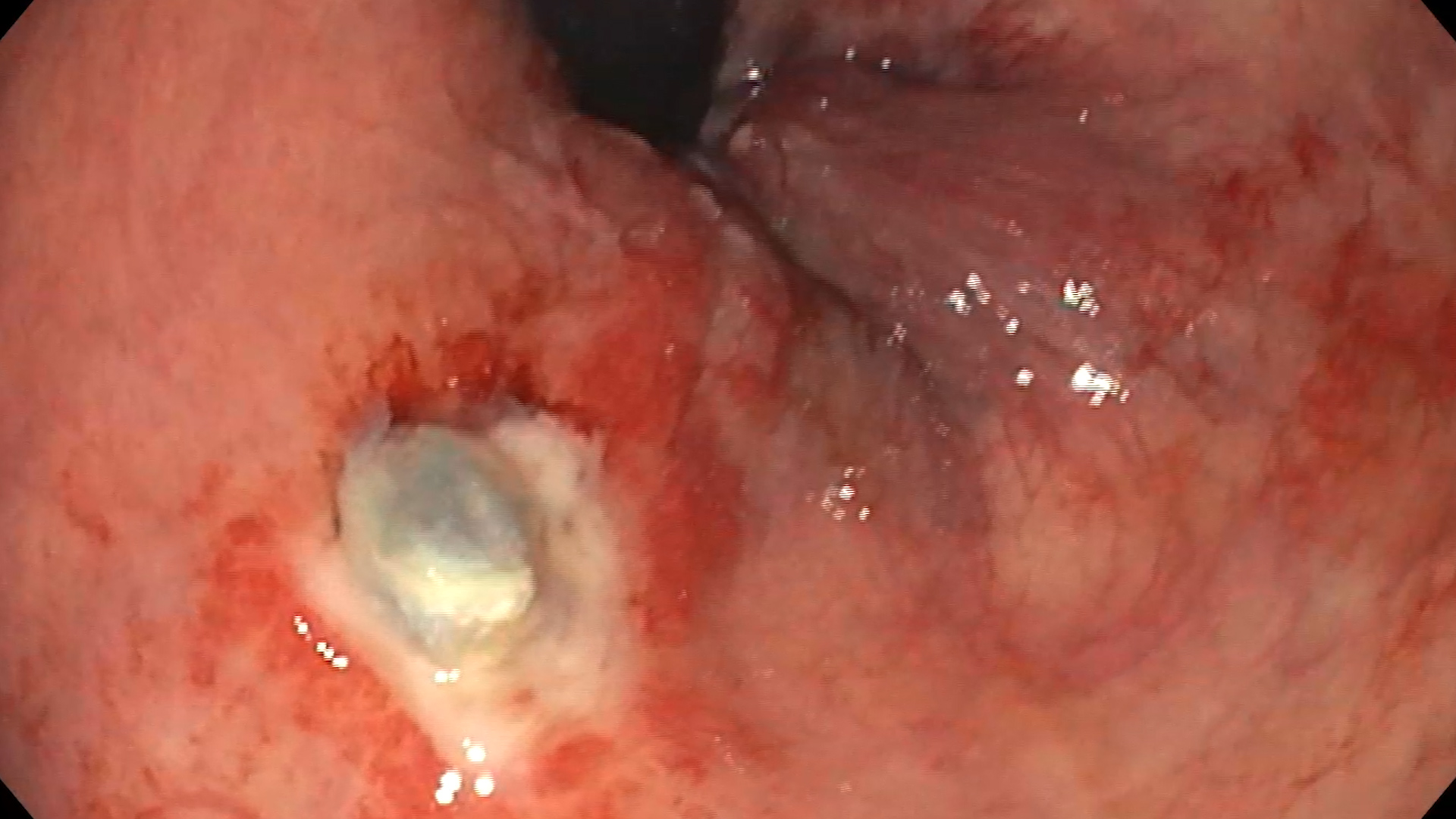
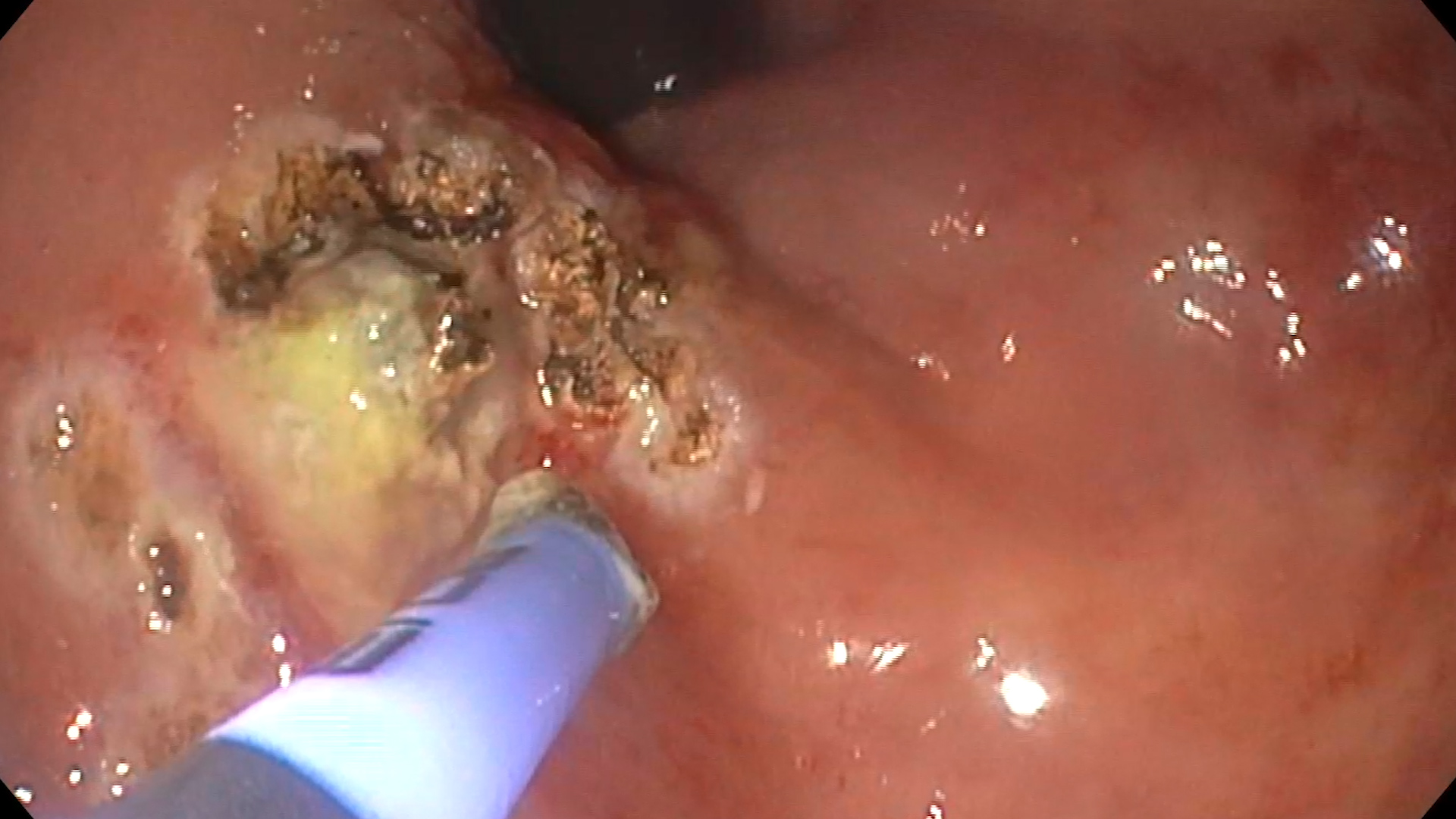
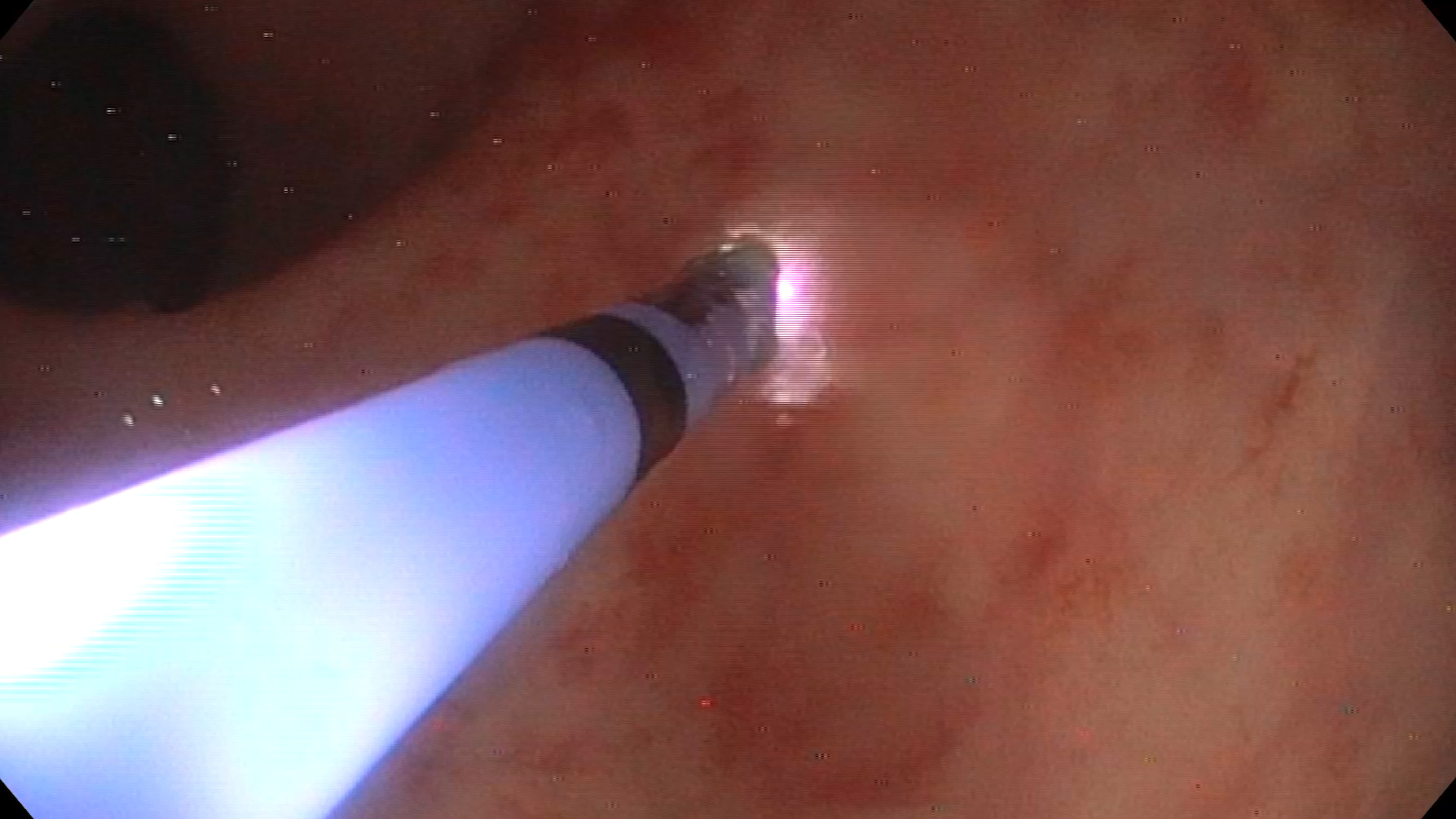
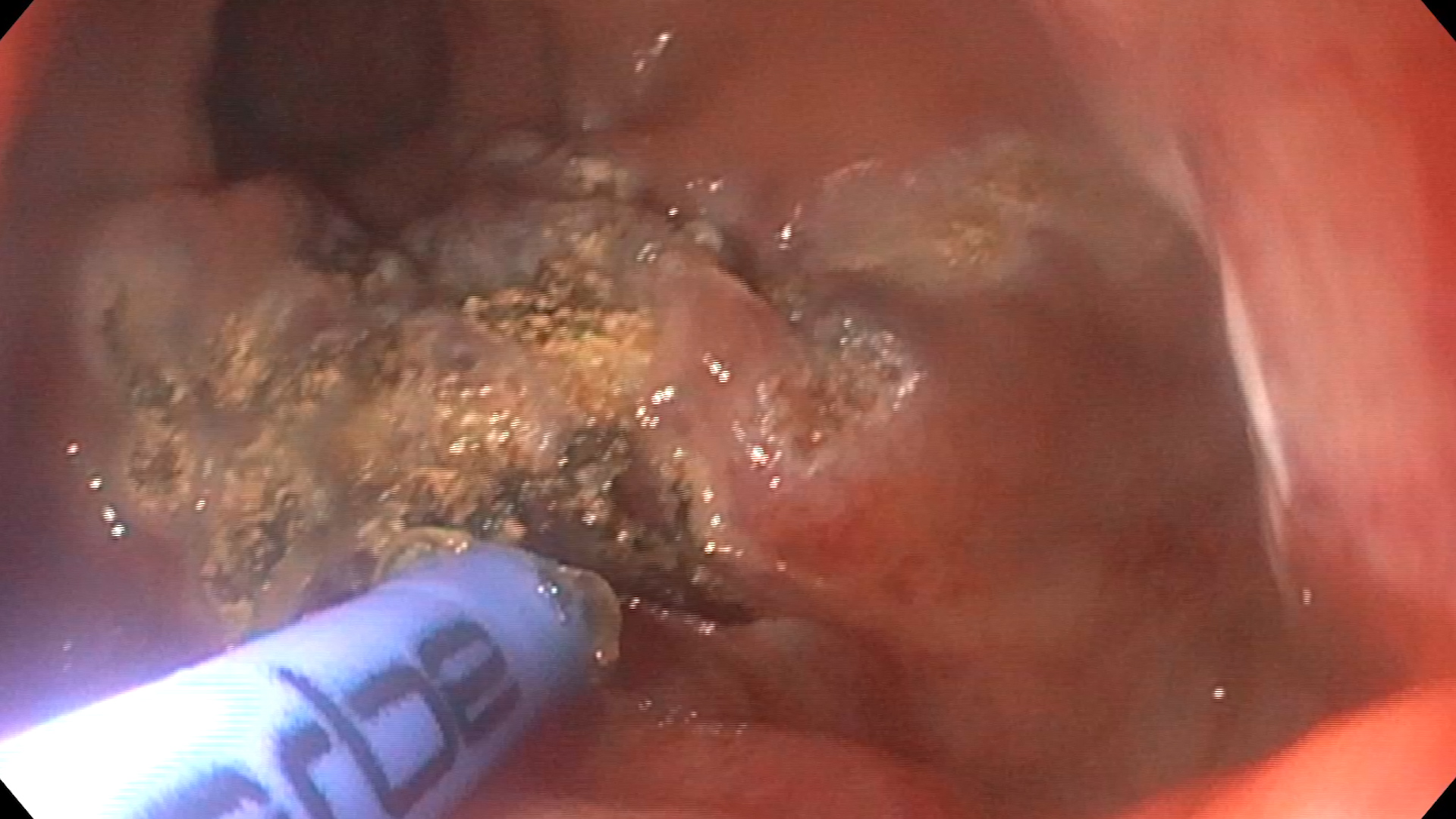
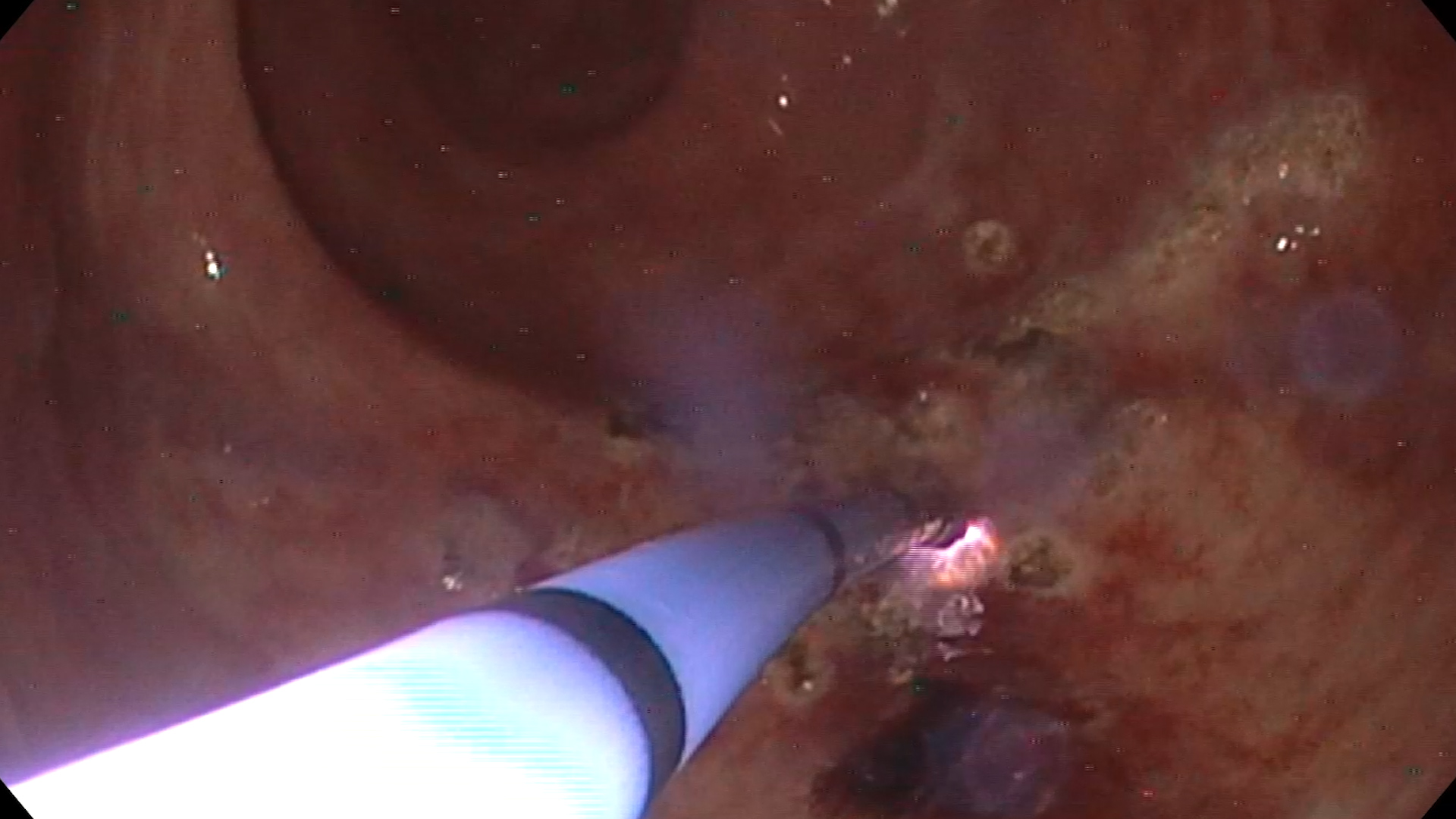
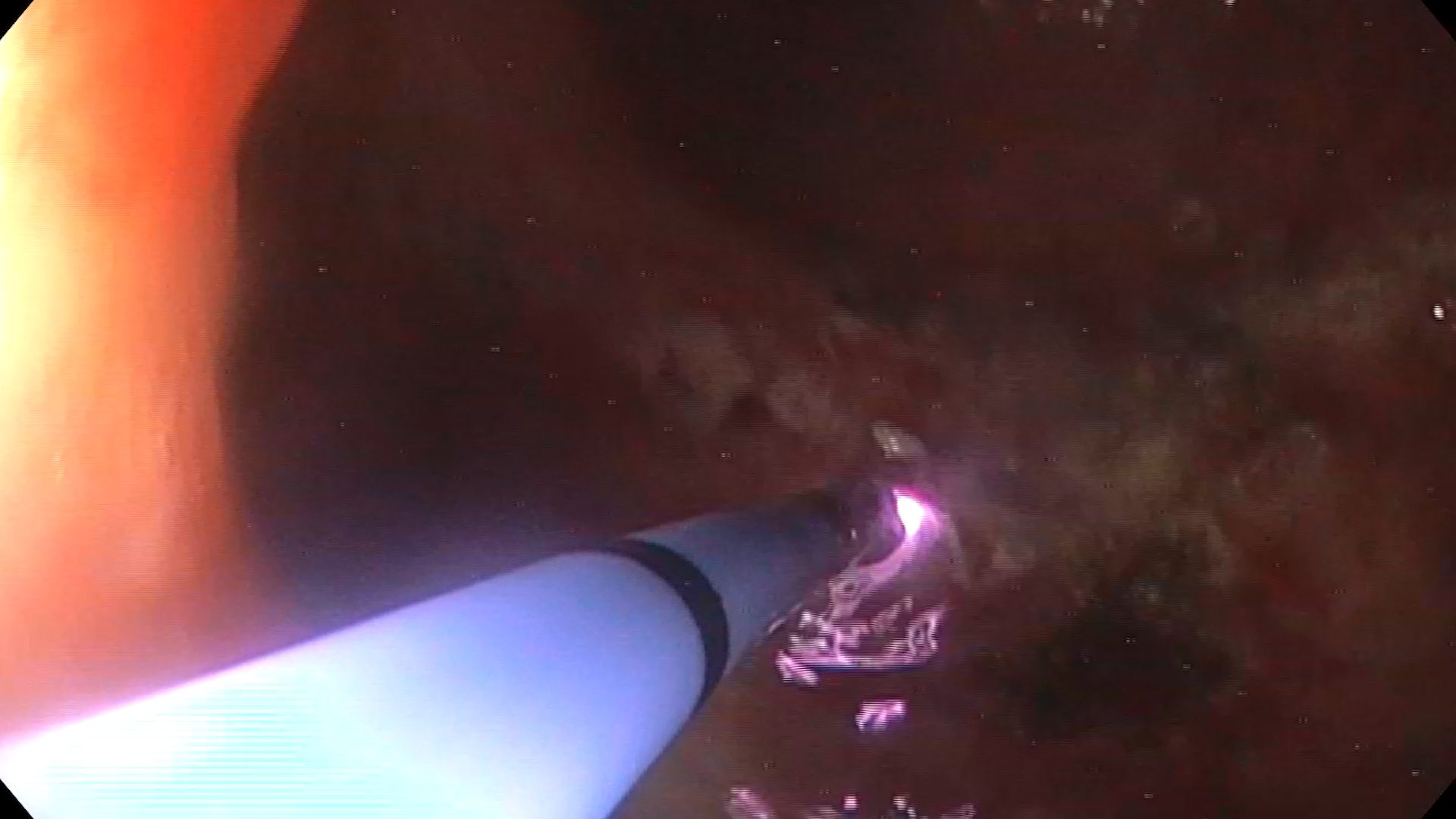
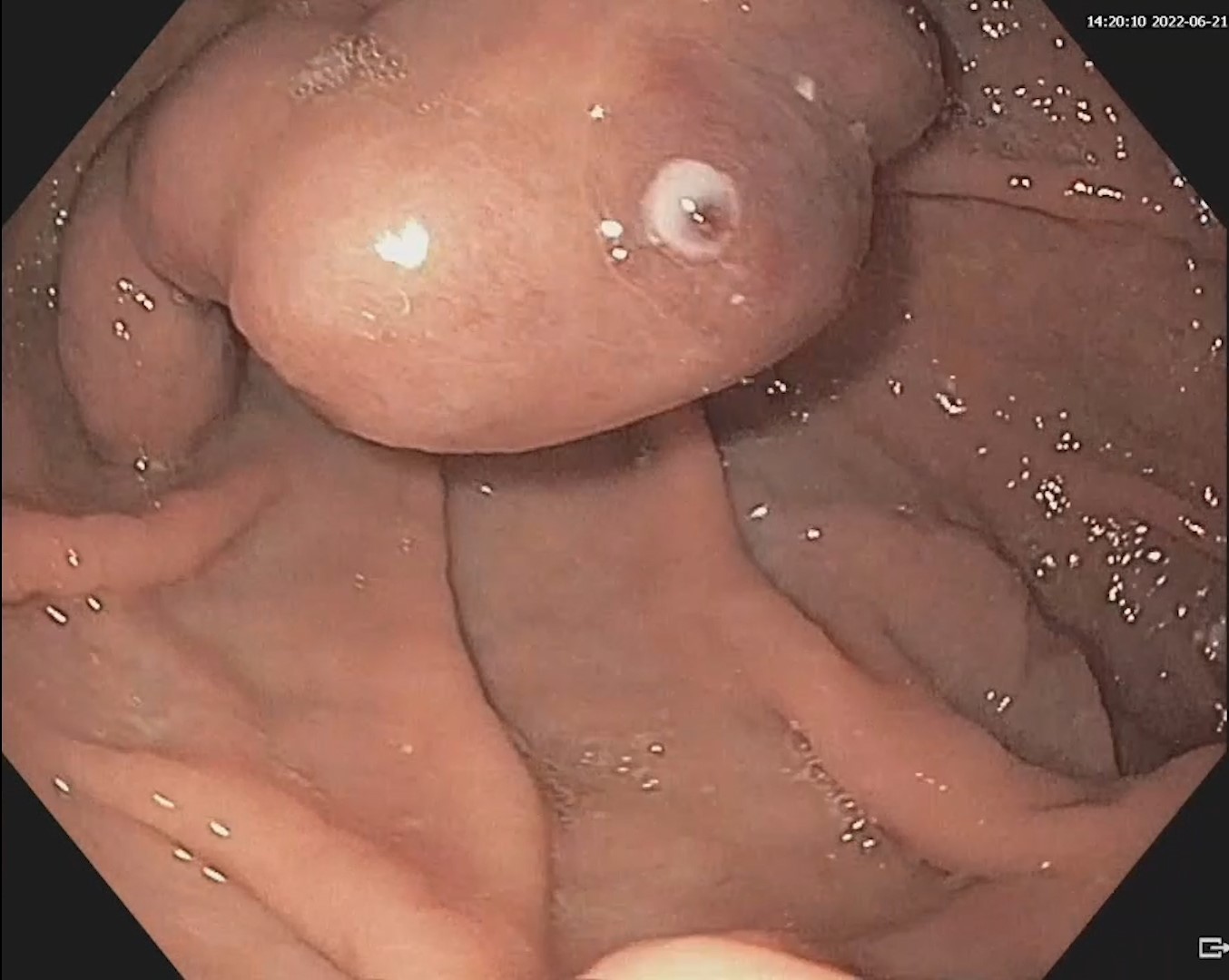
A colonoscopy was performed, revealing both internal and external hemorrhoids. Additionally, there was a fibrin-covered lesion with hematic fragments in the anal canal, likely related to post-hemorrhoidal ligation. Argon plasma coagulation (APC) was applied to the margins of this lesion (Figure 1). The first 10 cm from the anal orifice showed erythematous mucosa with multiple ulcerations and erosions, some of which bled easily upon contact with the endoscope. These areas were also cauterized using APC (Figure 2).
During hospitalization, the patient’s anemia was corrected, and prophylactic post-procedural antibiotic treatment was administered. Upon discharge, suppositories containing Sucralfate and Mesalasine were recommended. Despite this, rectal bleeding persisted, necessitating repeated red blood cell transfusions and multiple APC sessions.
With ongoing topical medication and repeated APC sessions, the patient’s clinical, biological, and endoscopic conditions gradually improved. After nine sessions of APC, lesions were confined to the first 5 cm from the anal orifice.
Radiation proctitis.
Radiation proctitis is a condition characterized by rectal lesions that occur as a side effect of radiotherapy for various pelvic malignancies. It affects approximately 5-11% of radiotherapy patients. Depending on the onset of symptoms, radiation proctitis is classified as either acute (if symptoms begin during or immediately after radiotherapy) or chronic (if symptoms appear at least three months after completing radiotherapy).
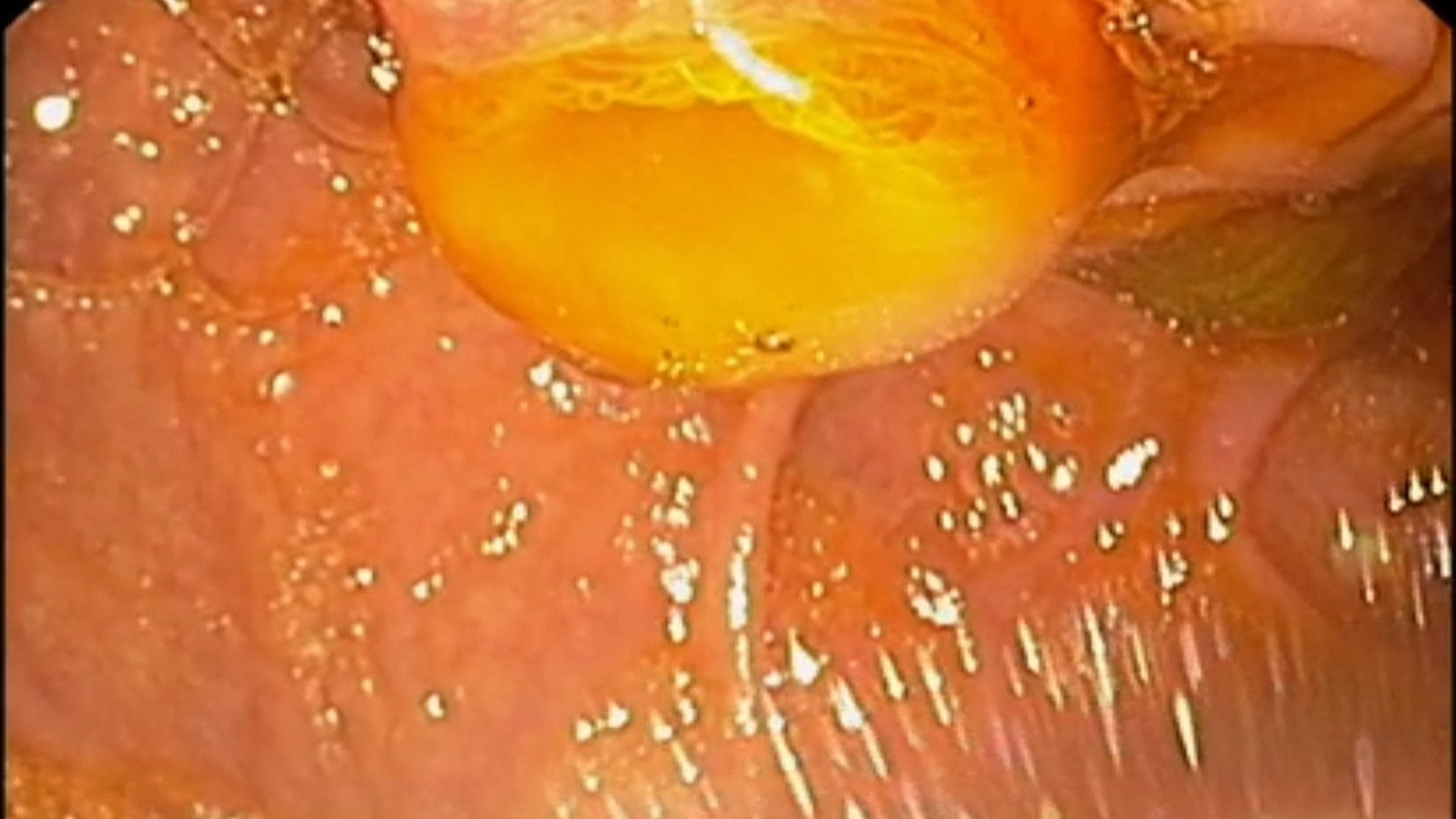
Radiation proctitis symptoms include diarrhea, abdominal pain, and rectal bleeding. Endoscopic findings show friable, edematous rectal mucosa with ulcerations and oozing. Pseudopolyps or strictures may also be observed.
Therapeutic options for chronic radiation proctitis include local applications of formalin (which chemically cauterizes lesions), mesalamine, ozone therapy, metronidazole, short-chain fatty acid enemas, and sucralfate enemas. Endoscopic treatments such as APC and hyperbaric oxygen therapy have also been successful. Other promising but less studied endoscopic treatments recommended by the American Society for Gastrointestinal Endoscopy include electrocoagulation, radiofrequency ablation, cryoablation, and heater probe.
Patients who do not respond to medical and endoscopic treatment, or who experience complications like rectal obstruction, fistulae, or perforation, may require surgical intervention.
Radiation proctitis is a condition with significant morbidity among patients who have undergone radiotherapy. However, it can be managed with various therapeutic options, including medical, endoscopic, and surgical treatments.
1. McKeown DG, Gasalberti DP, Goldstein S. Radiation Proctitis. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan.
2. Paquette IM, Vogel JD, Abbas MA, Feingold DL, Steele SR; Clinical Practice Guidelines Committee of The American Society of Colon and Rectal Surgeons. The American Society of Colon and Rectal Surgeons Clinical Practice Guidelines for the Treatment of Chronic Radiation Proctitis. Practice Guideline Dis Colon Rectum 2018; 61(10): 1135-1140.
3. Dahiya DS, Kichloo A, Tuma F, Albosta M, Wani F. Radiation Proctitis and Management Strategies. Review Clin Endosc 2022; 55(1): 22-32.
4. McCrone LF, Neary PM, Larkin J, McCormick P, Mehigan B. The surgical management of radiation proctopathy. Review Int J Colorectal Dis 2017; 32(8): 1099-1108.