See other cases
Colonic stenting
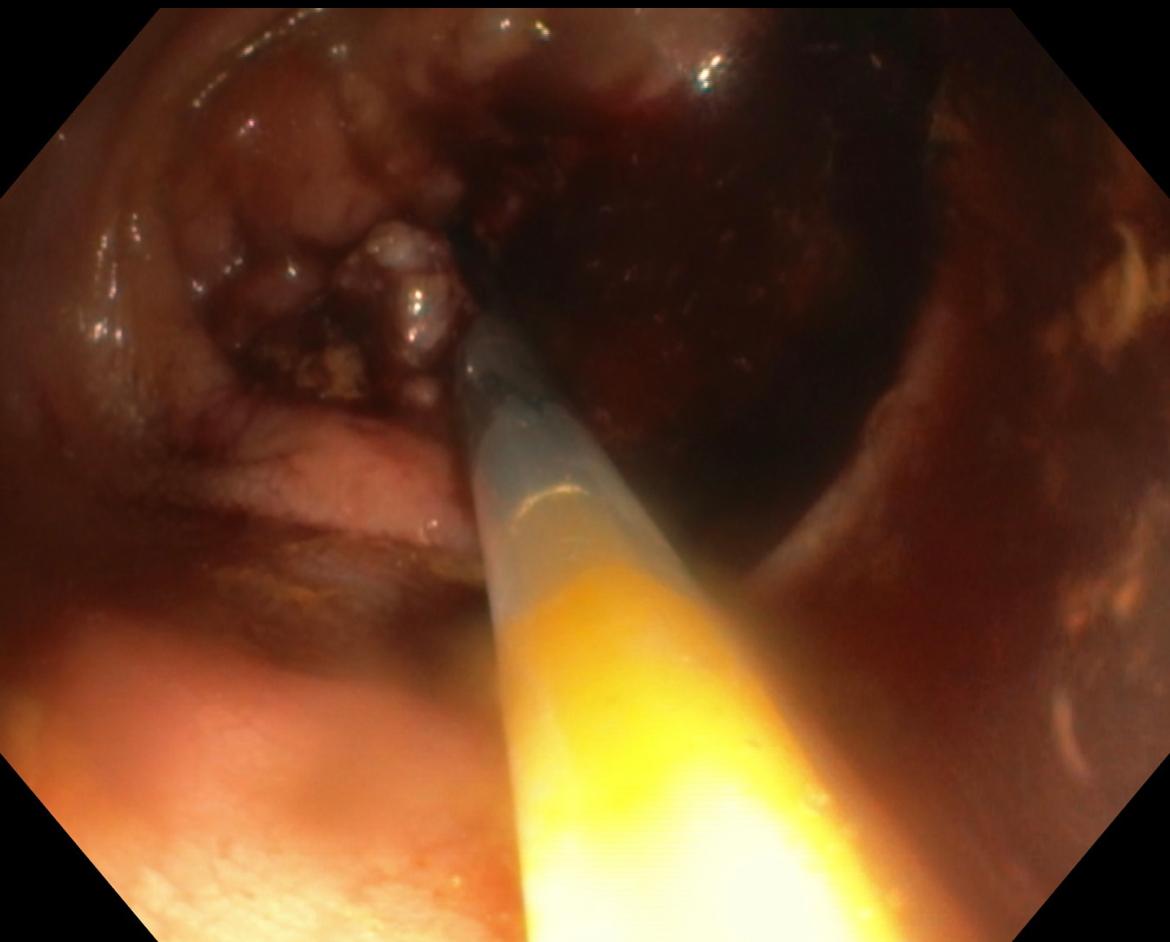
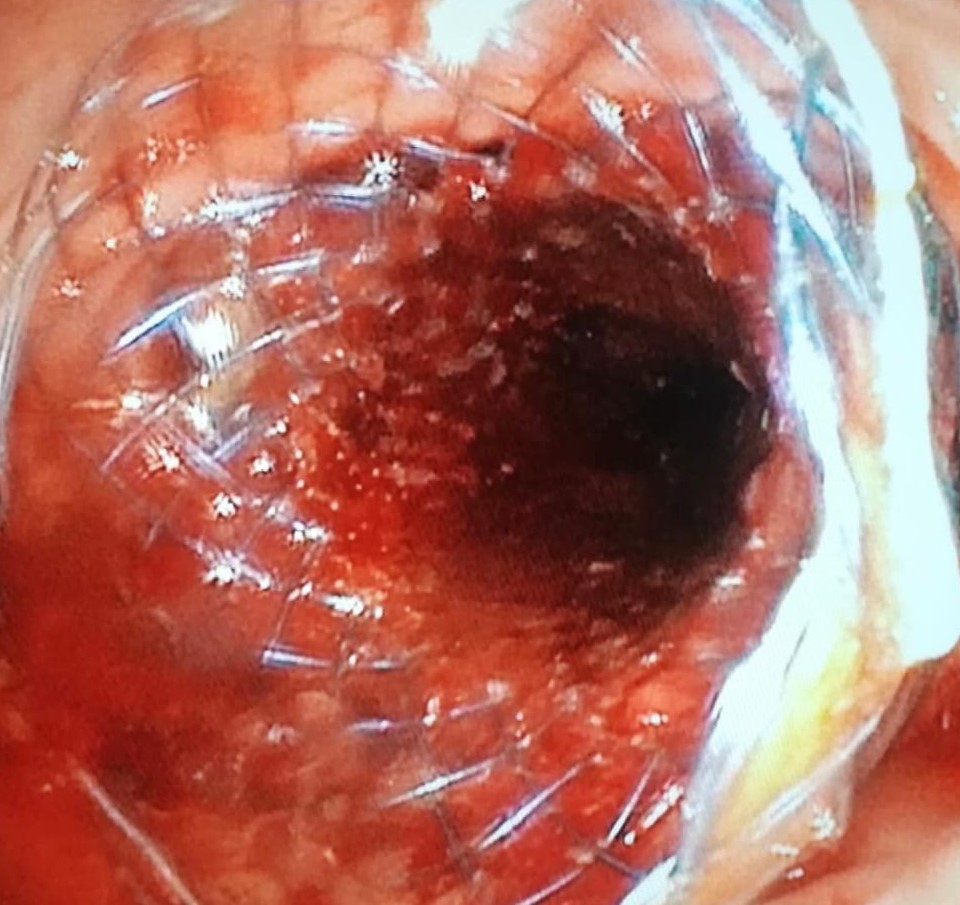
A 93-year-old patient with a history of intestinal occlusion due to middle-superior rectal stenotic neoplasm (ADK) and endoscopic management of intestinal occlusion, for which a 90/25 mm uncovered colonic stent was placed (Fig. 1-3) 6 months ago, presented to the emergency room for: diffuse abdominal pain, vomiting and accelerated intestinal transit, 5-6 soft stools per day. The patient also had multiple liver and lung metastases and associated cardiac and pulmonary pathology.
Clinical: average general state, dehydrated, distended abdomen, painful spontaneously and with palpation.
Biological: hemoglobin 11 g/dl, mild hypokalemia, increased inflammatory markers (leukocytosis, CRP, ESR)
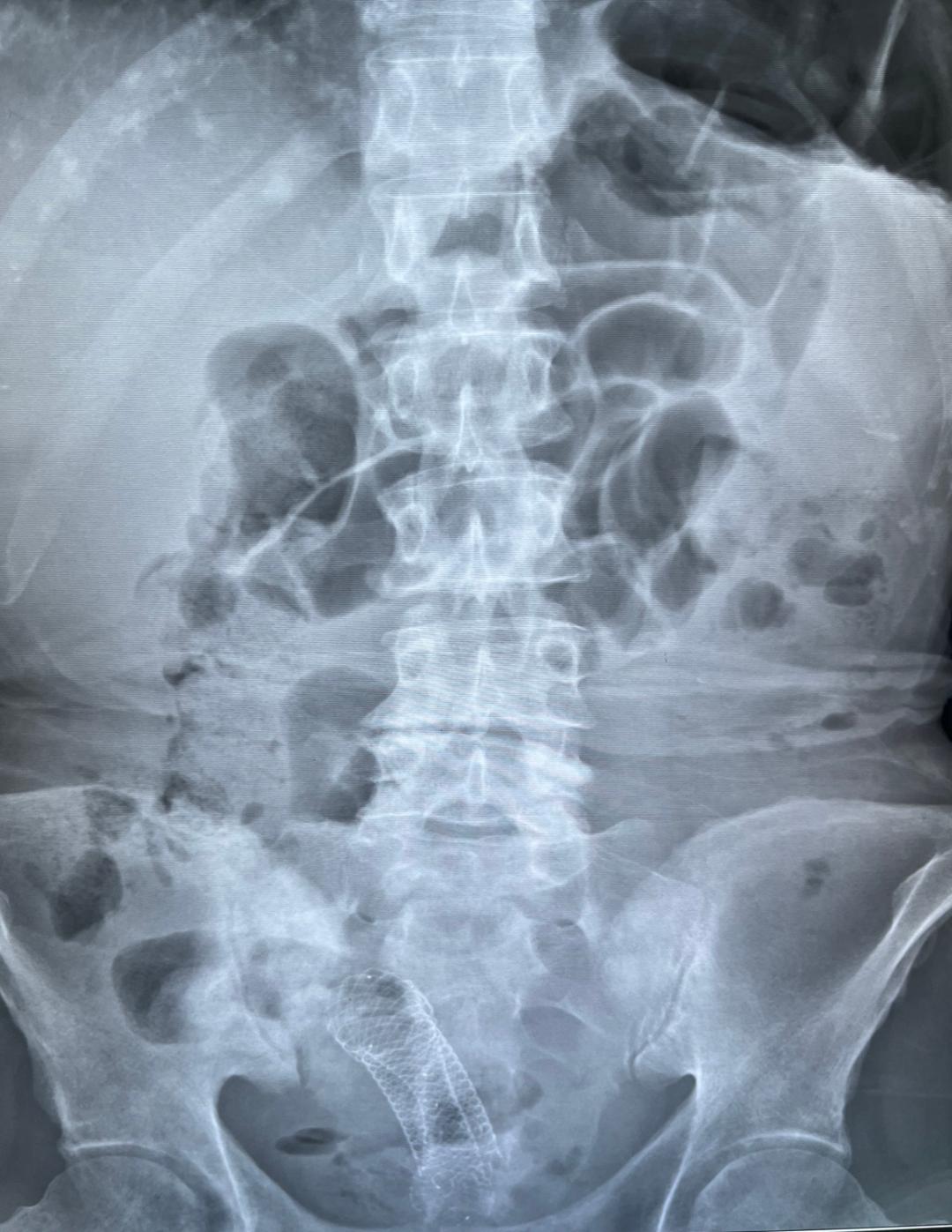
Abdominal X-ray on empty stomach: intestinal loops distended by volume with hydro-aerial level in the left flank; fully expanded stent in the pelvis, without pneumoperitoneum.
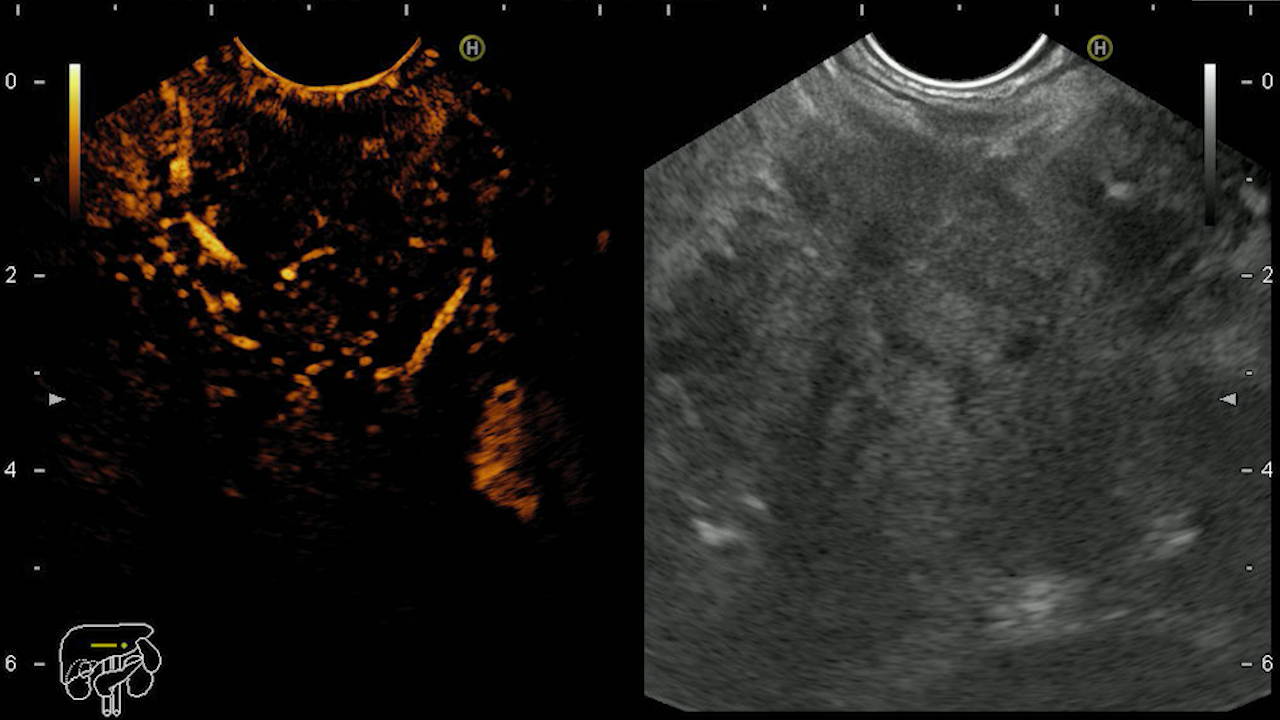
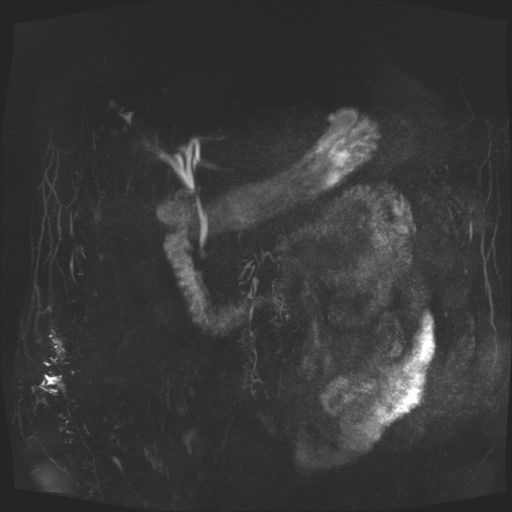
Chest+abdomen+pelvis CT scan with contrast substance: rectal stent in situ, dilated intestinal loops, multiple liver and lung metastases (Fig. 4).
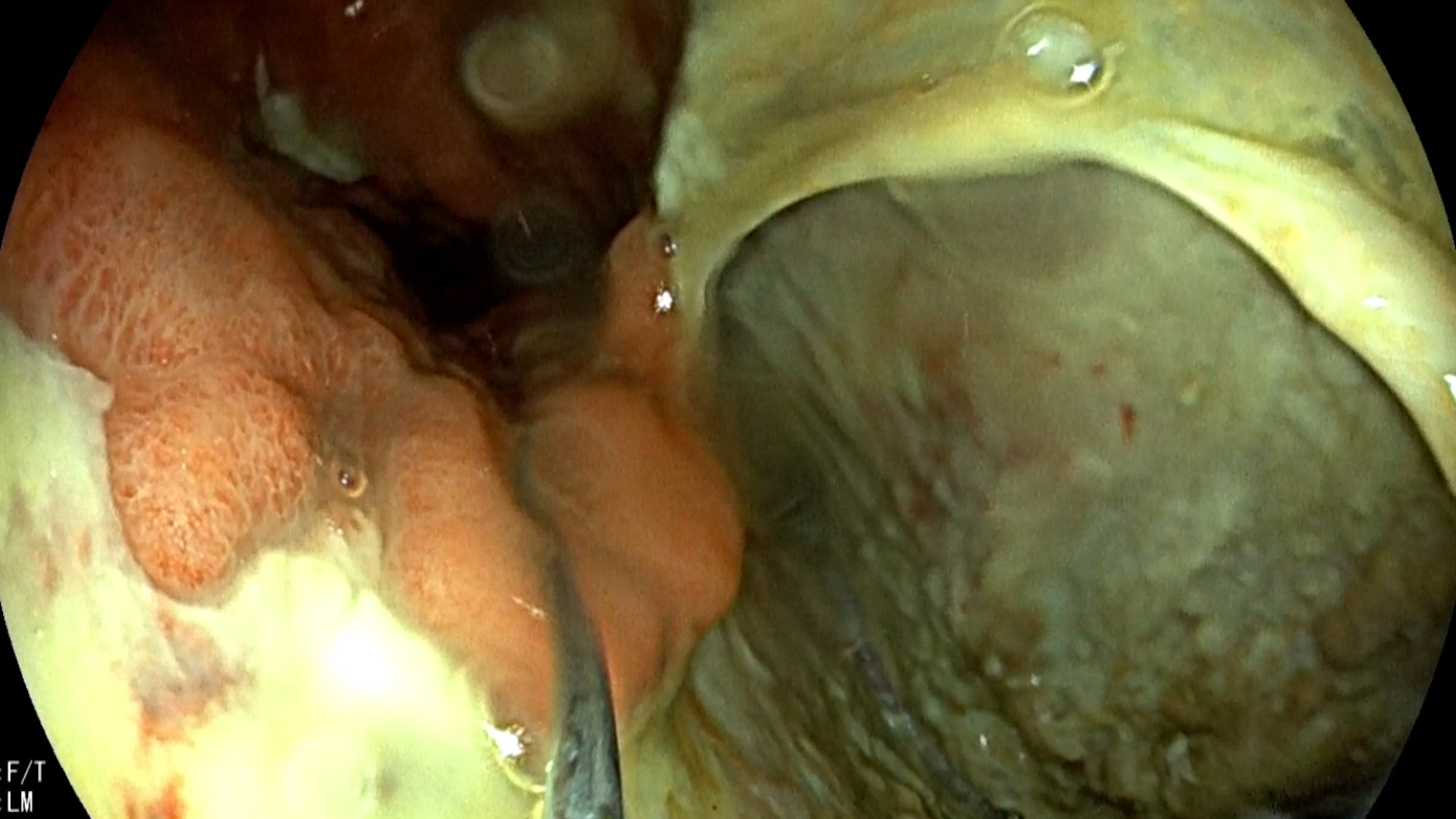
A rectoscopy was performed (preparation performed with evacuation enemas): at approximately 10 cm from the anus, the distal end of the colonic stent in situ, the pediatric colonoscope could not pass through its lumen, due to tumor proliferation at the level of the colonic stent.
Under radiological and endoscopic guidance, through the lumen of the previously mounted colonic stent, it was placed a second colonic stent, partially covered 120/22 mm (Fig. 5).
The patient was discharged 3 days after with an improved general condition, the resumption of normal intestinal transit and the disappearance of vomiting.
Subocclusive syndrome. Endoscopically stented rectal neoplasm. Liver and pulmonary metastases.
The mounting of colonic stents is a minimally invasive method for colonic decompression in colonic stenotic neoplasm.
Indications for colonic stenting:
- Occlusion in patients with stage IV neoplastic disease and associated comorbidities.
- Bridging in the case of patients with occlusion in the context of colonic neoplasm, with the aim of performing minimally invasive surgical tumor resection (laparoscopic) or to reduce the number of surgical interventions (stoma + distal colon repositioning in transit), in patients with associated comorbidities.
Contraindications to colonic stenting are represented by generalized peritonitis or hemorrhagic colonic neoplasm. The location at the level of the flexures (hepatic and splenic) or those at the level of the right colon, presents a high degree of technical difficulty, being considered relative contraindications.
The particularity of the case is represented by the possibility of minimally invasive endoscopic management of intestinal occlusion, in a patient with a history of endoscopically stented rectal neoplasm and tumor proliferation through the lumen of the uncovered colonic stent, in a patient with liver and lung metastases and multiple associated comorbidities.
- Eduardo A. Bonin, Todd H. Baron. Update on the Indications and use of colonic stents. Current Gastroenterology Reports 2010; 374-382.
- Kenneth Buxey Hanu Chouhan. Role and timing of colonic stenting in colorectal cancer. Digestive Medicine Research 2021; 20-133.