See other cases
Enteral stenting
A 78-year-old female patient, with no significant past medical history, presents forlate postprandial vomitingand significant weight loss with onset for about two months.
Clinical – altered general condition, underweight, normally-shaped abdomen, with no spontaneous or palpatory pain, roughand irregular inferior liver border, positioned at 3 cm below the costal margin.
Biological – no significant changes.
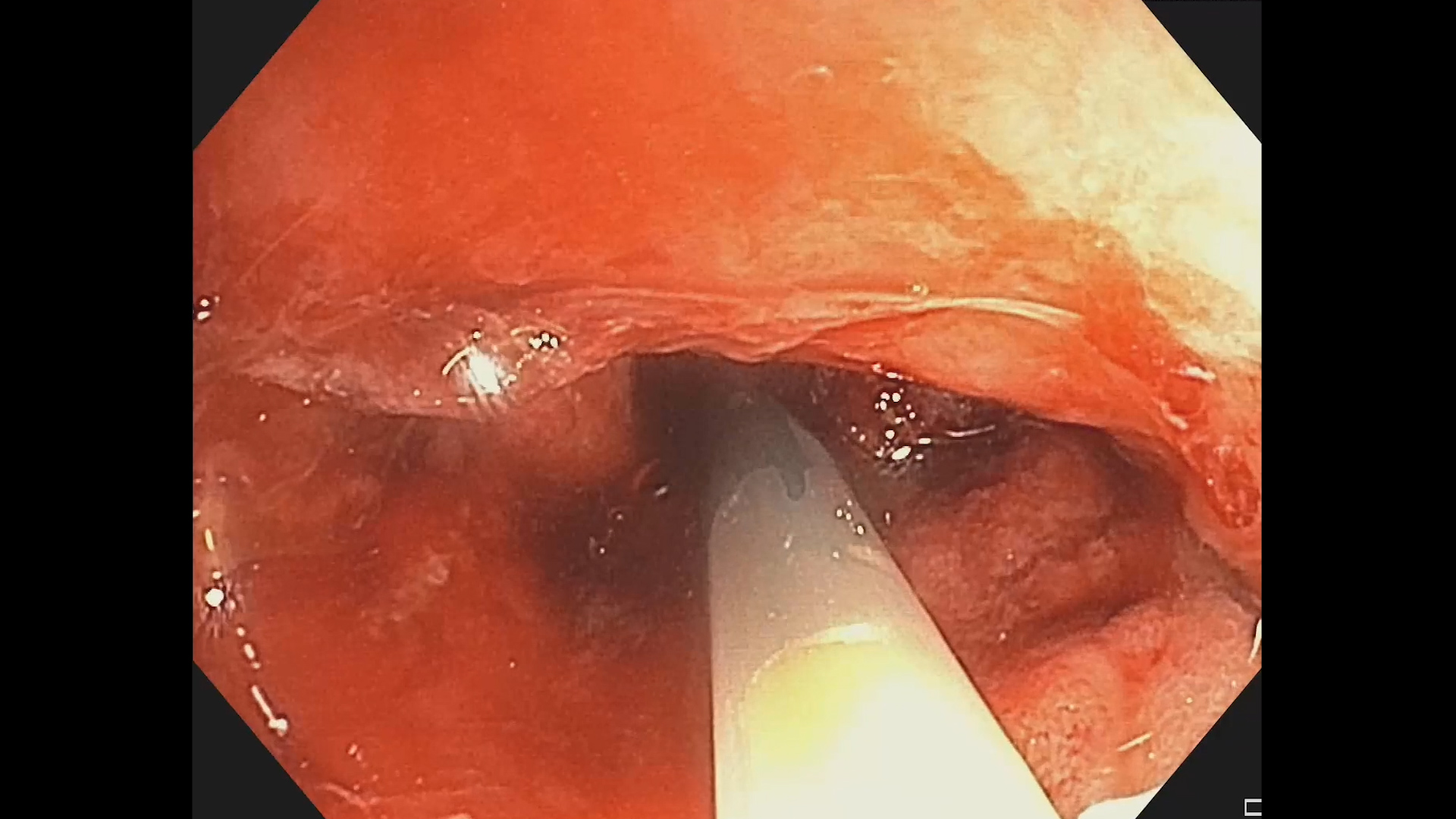
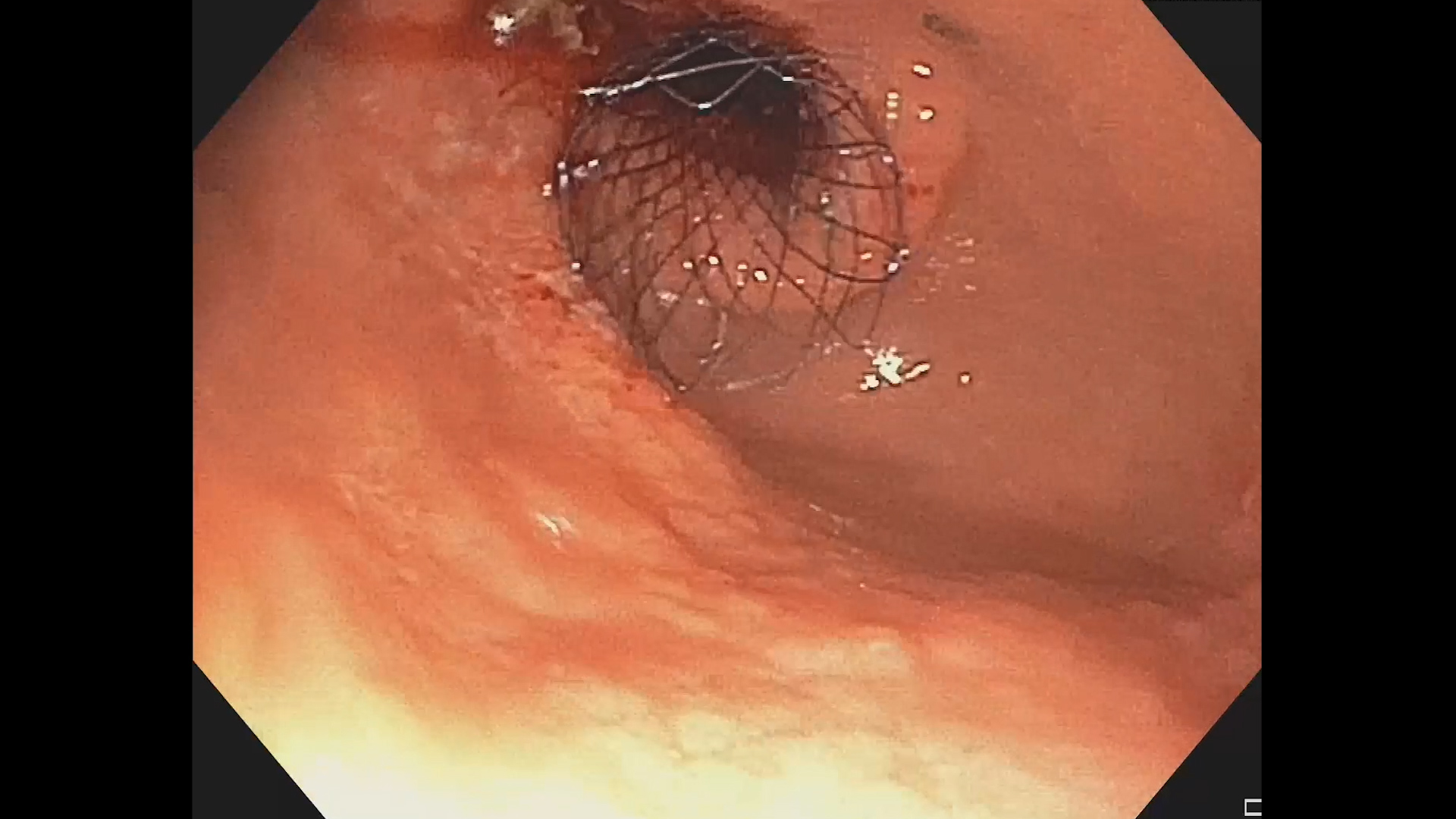
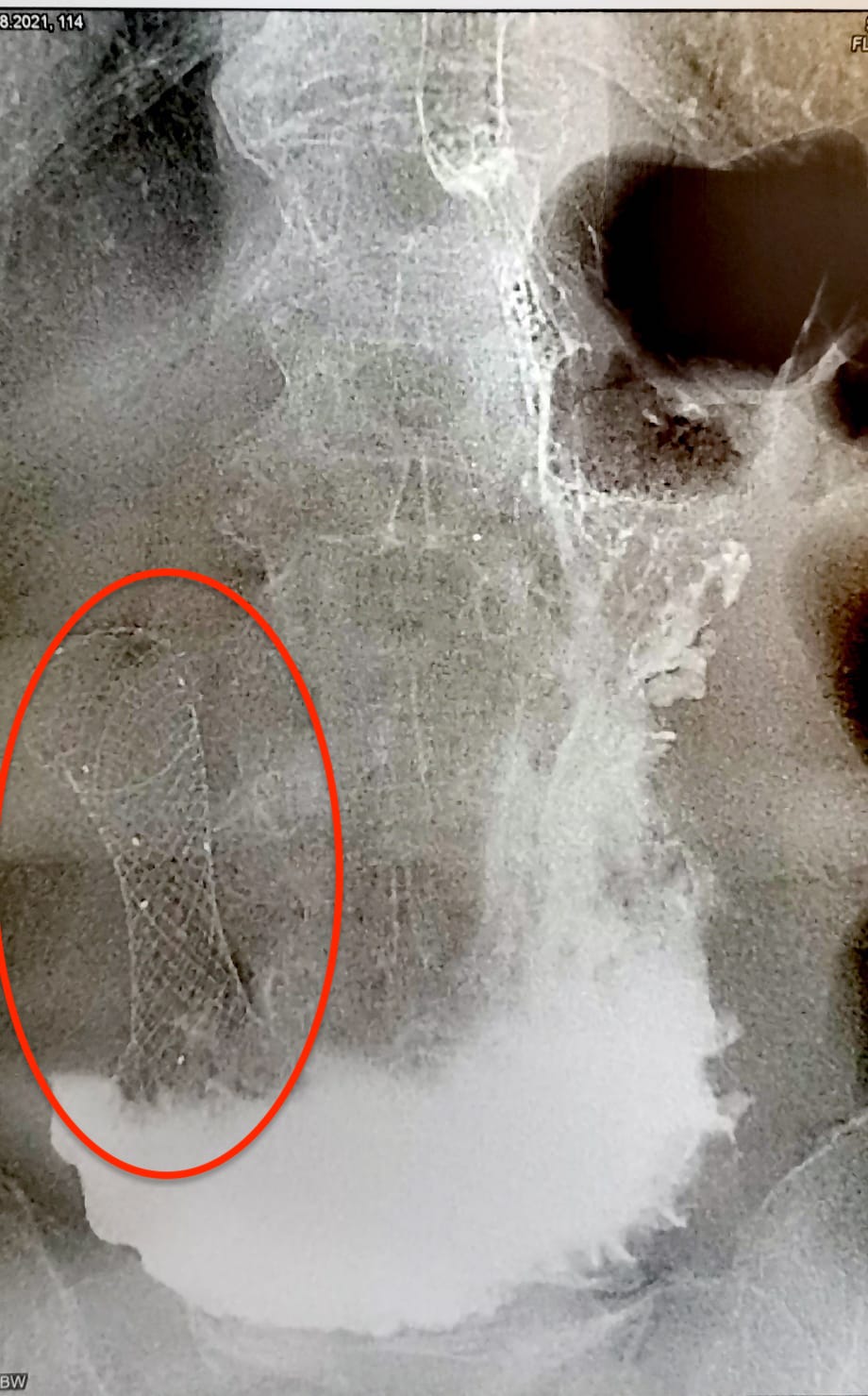
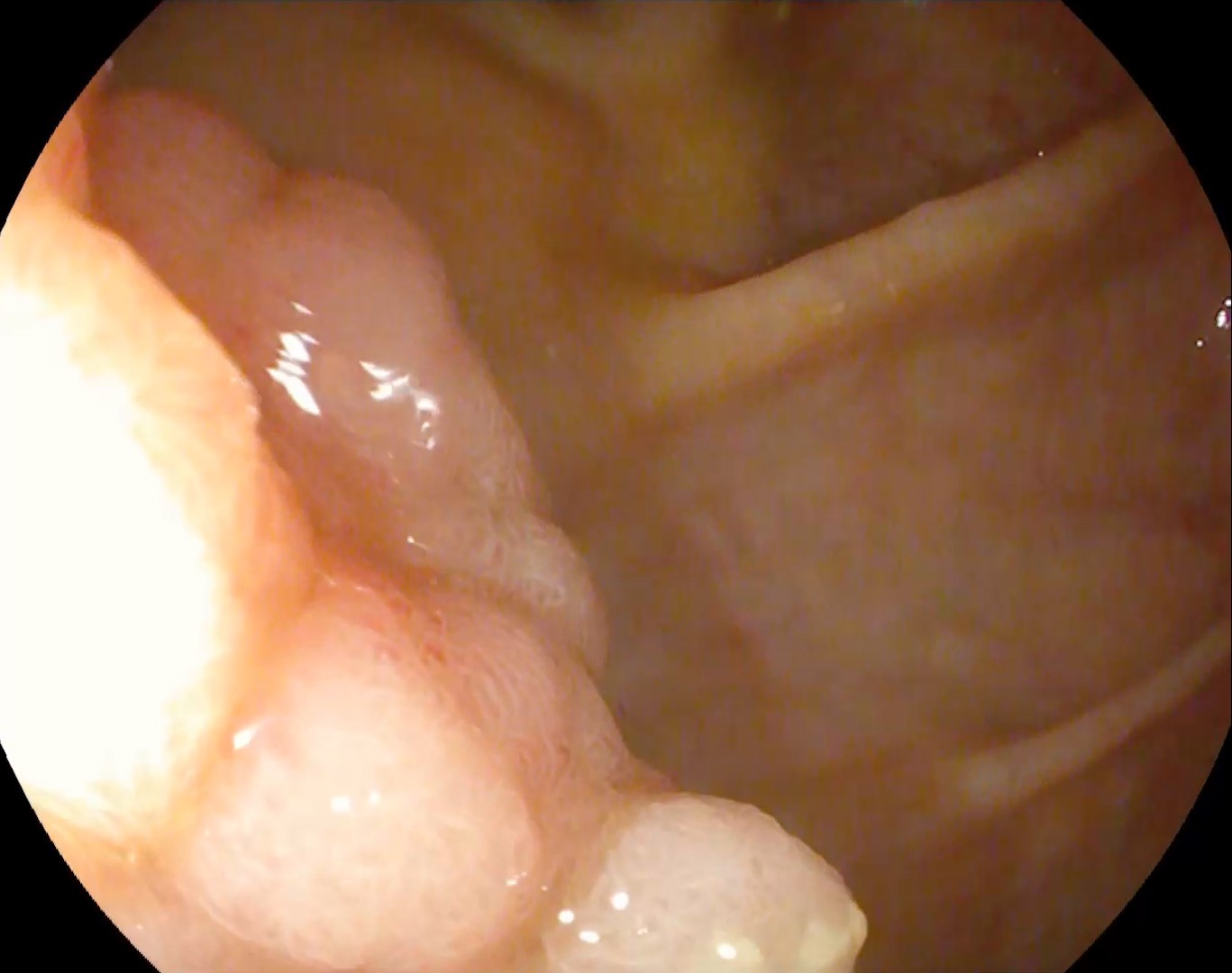
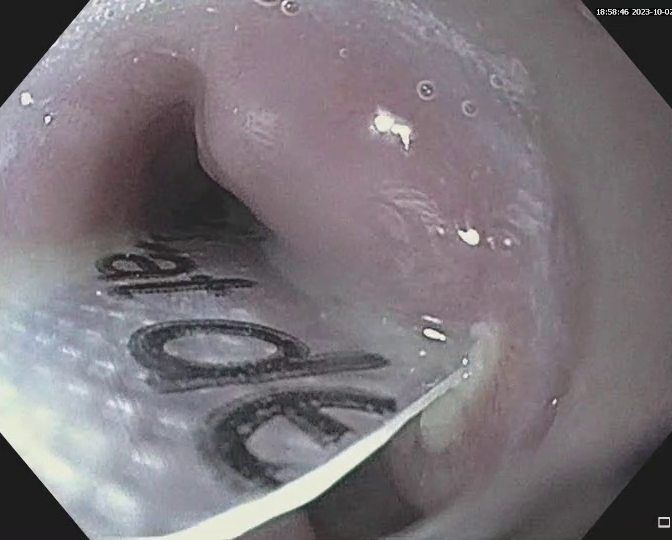
Upper GI endoscopy revealsa significant amount of food in the stomach; from the antrum with extension to the pylorus the mucosa appears irregular, friable andtumor-infiltrated,causing significant luminal stenosis that can behardly passed with the endoscope. The lesion also extends to the duodenal bulb. Multiple biopsies are obtained (histopathological result: ulcerated, moderately differentiated, invasive gastric adenocarcinoma). Abdominal CT scan with intravenous contrast reveals multiple images in the liver highly suggestive of metastasis. Upper GI endoscopy is again undertaken and a 60X22 mm enteral uncovered self-expandable metal stent (SEMS)is placed transpyloric under direct vision. After the procedure, an abdominal X-ray with water-soluble orally-administered contrast is performed, showing stent permeability and passage of the contrast medium to the distal duodenum.
Infiltrative antropyloric gastric neoplasm. Gastric outlet obstruction. Liver metastasis.
Endoscopic enteral stenting is used for restoration of luminal patency in patients with malignant gastric outlet obstruction due to inoperable gastric or duodenal tumors, associated with poor prognosis and a short life expectancy. Generally, uncovered SEMS are used due to the higher risk of stent migration in the duodenum. However, uncovered SEMS are associated with higher rates of tumor ingrowth or overgrowth compared with covered SEMSs. Other complications are gastrointestinal bleeding, perforation (approximately 1%) and biliary obstruction that may occur when covered SEMSs are placed in the papillary region. In this case, due to the advanced neoplasia, the reduced life expectancy and the low overall performance status of the patient which did not allow surgical intervention, we chose to place an enteral stent.
Enteral endoscopic stenting for inoperable malignant gastric outlet obstruction (due to advanced disease or a low performance status of the patient) is a successful alternative to surgery in order to ensure enteral nutrition.
- van Halsema EE, Rauws EA, Fockens P et al. Self-expandable metal stents for malignant gastric outlet obstruction: A pooled analysis of prospective literature. World J Gastroenterol. 2015;21(43):12468-81
- Jeurnink SM, Steyerberg EW, van Hooft JE et al; Dutch SUSTENT Study Group. Surgical gastrojejunostomy or endoscopic stent placement for the palliation of malignant gastric outlet obstruction (SUSTENT study): a multicenter randomized trial. Gastrointest Endosc. 2010;71(3):490-9
- Kim M, Rai M, Teshima C. Interventional Endoscopy for Palliation of Luminal Gastrointestinal Obstructions in Management of Cancer: Practical Guide for Oncologists. Journal of Clinical Medicine. 2022; 11(6):1712