See other cases
Endoscopic management of biliary anastomotic stricture after liver transplantation
We present the case of a 53-year-old patient with an orthotopic liver transplant performed in May 2025 for liver cirrhosis of viral etiology (hepatitis B+D), with a history of antiviral treatment failure after multiple courses (interferon, ribavirin, entecavir), also presenting a dysplastic hepatic nodule. Associated comorbidities include insulin-dependent type 2 diabetes mellitus, arterial hypertension, splenic artery pseudoaneurysm, and hypothyroidism secondary to chronic autoimmune thyroiditis, managed with levothyroxine replacement therapy.
Clinical findings: palpable hepatomegaly.
Laboratory results: hepatocellular injury pattern with ALT predominance (AST 150 U/L, ALT 250 U/L), gamma-GT 400 U/L, alkaline phosphatase 350 U/L, total bilirubin 1.6 mg/dL.
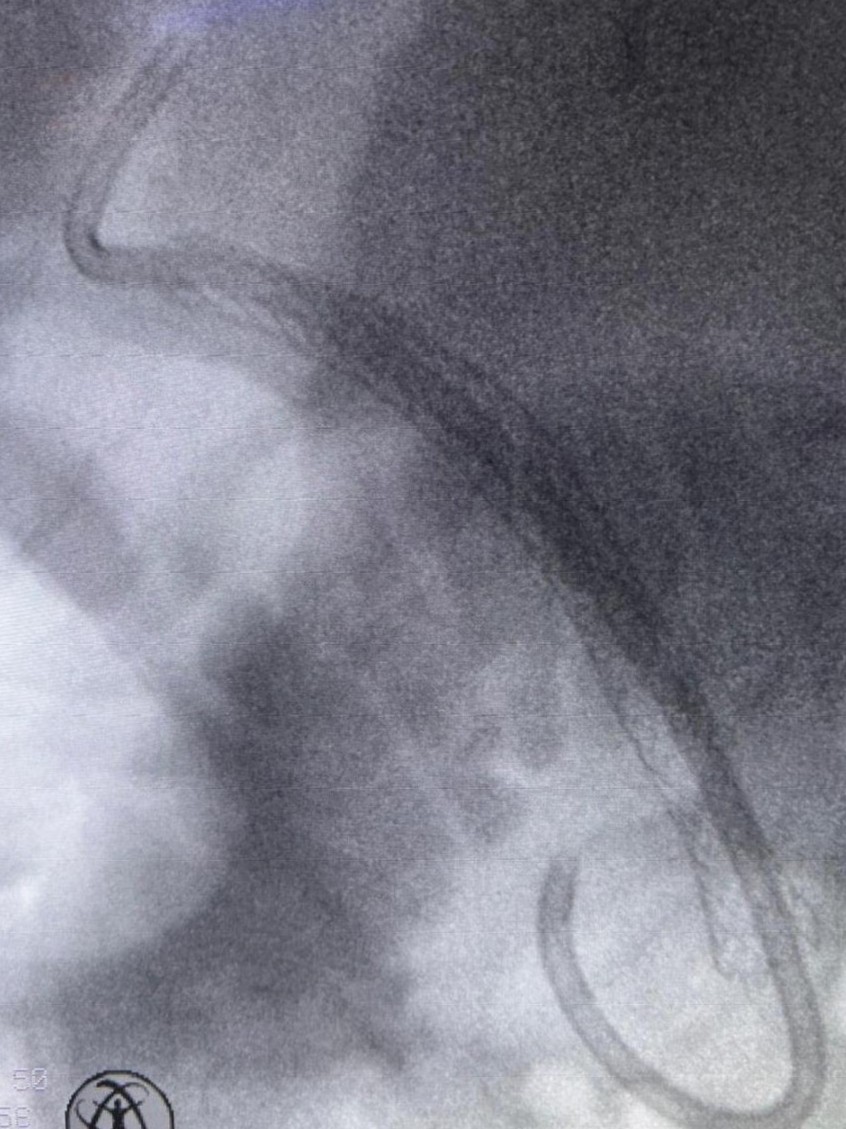
Magnetic resonance cholangiography (MRCP) revealed mild intrahepatic bile duct dilatation in both hepatic lobes, a tight anastomotic stricture of the common bile duct, and dilation of the common bile duct above the bilio-biliary anastomosis up to 11 mm (Fig. 1).
ERCP was performed as follows:
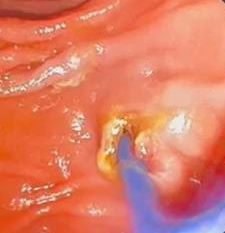
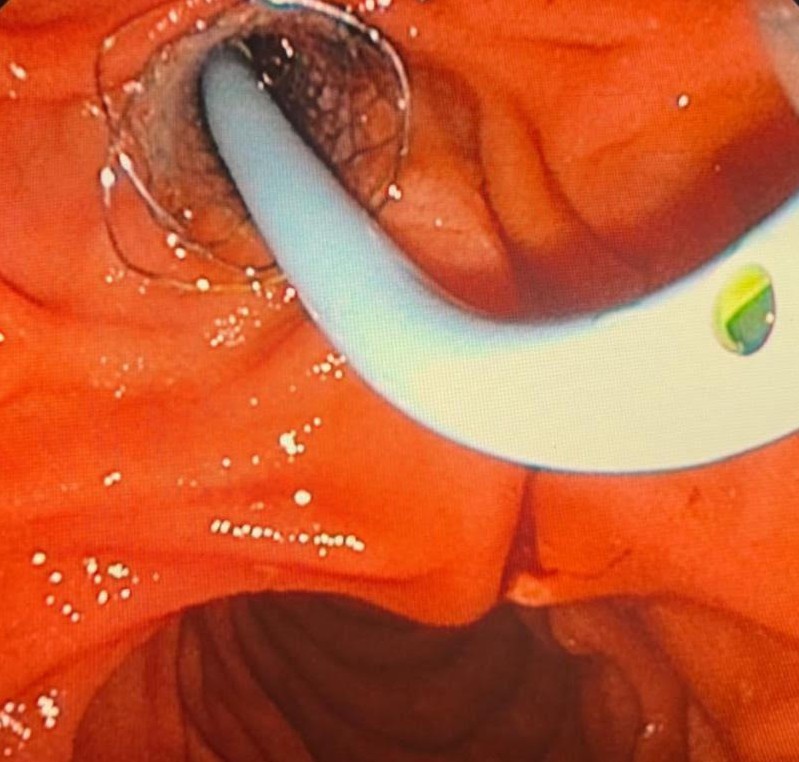
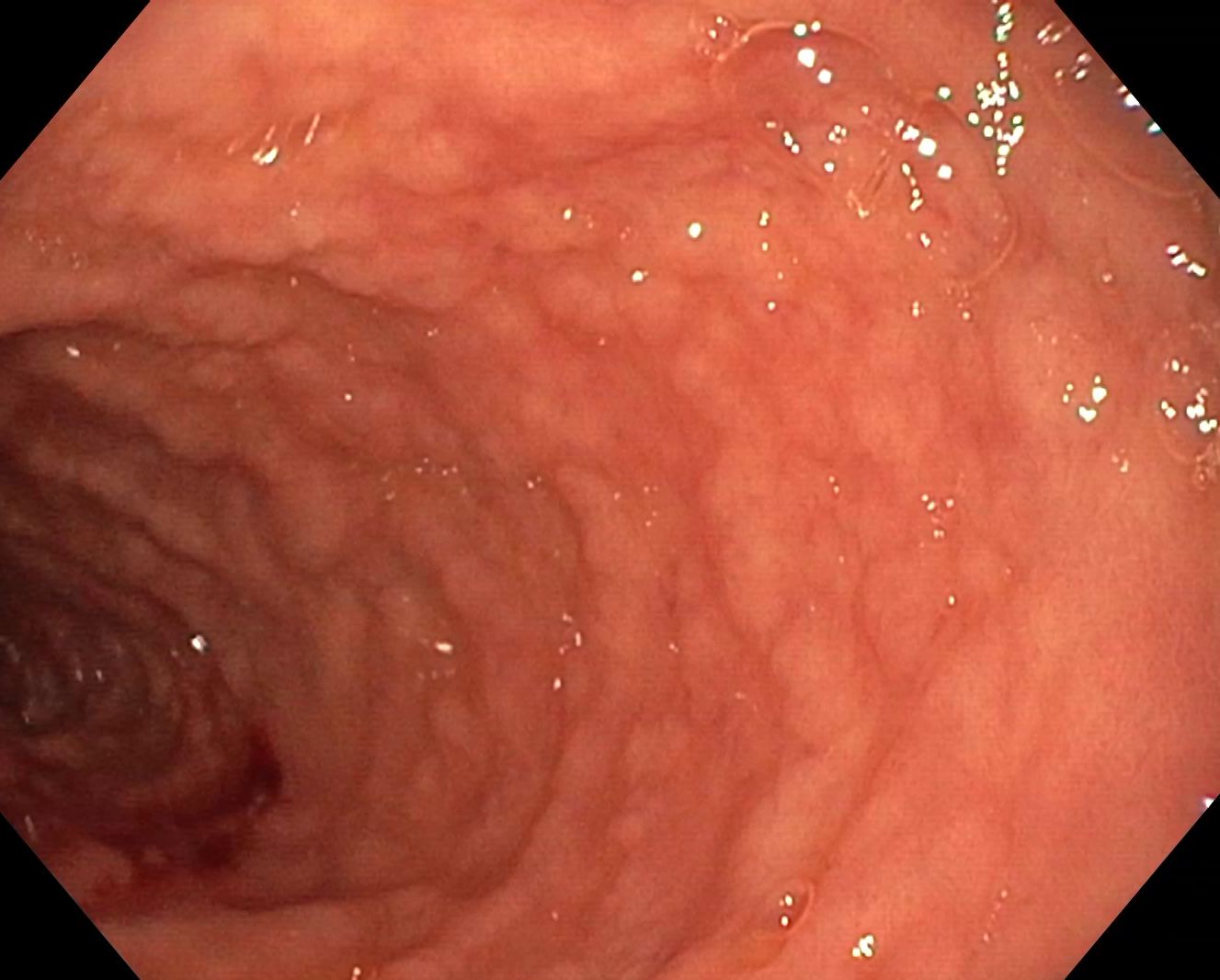
Selective cannulation of the common bile duct (CBD) was achieved using a 0.025-inch guidewire-assisted sphincterotome. Injection of radiopaque contrast revealed a tight mid-choledochal stricture, associated with mild intrahepatic bile duct dilatation. The CBD was dilated above the biliary anastomosis up to 11 mm, with the distal CBD measuring 6 mm. A wide endoscopic sphincterotomy was performed, and attempts were made to advance a 0.025-inch guidewire—both angled and straight—into the intrahepatic biliary tree; however, the anastomotic biliary stricture could not be traversed. Subsequently, the SpyGlass cholangioscope was introduced, enabling direct visualization of the biliary anastomotic stricture and successful passage of the 0.025-inch guidewire across the stenotic segment into the intrahepatic bile ducts. Balloon dilation of the biliary stricture was then performed using a 6/40-mm balloon under combined cholangioscopic and fluoroscopic guidance. Following endoscopic bilioplasty, the cholangioscope advanced through the stricture easily, and tissue samples were collected from the choledochal anastomosis (Fig. 2 and Video 1). A fully covered 8/80mm biliary self-expanding metal stent (SEMS) was subsequently placed, followed by insertion of a 10 Fr/5cm double-pigtail plastic biliary stent through the SEMS to prevent migration of the fully covered stent (Fig. 3, Fig. 4).
Benign biliary anastomotic stricture after orthotopic liver transplantation-biopsy. Endoscopic sphincterotomy. Cholangiography and balloon bilioplasty. Placement of a self-expanding metal biliary stent, anchored with a double-pigtail plastic stent to prevent migration.
Endoscopic therapy is the first-line approach for managing anastomotic strictures following liver transplantation. (1) Early anastomotic strictures (occurring within the first 30 days post-transplant) generally respond well to endoscopic treatment, with complete resolution typically achieved within approximately three months. In contrast, late anastomotic strictures (developing more than one month after transplantation) often require repeated therapeutic sessions over 12–24 months. (2)
Endoscopic therapy using progressively placed multiple plastic stents is effective but necessitates a higher number of repeat procedures. Conversely, fully covered self-expanding metal stents reduce the number of interventions required but are associated with a higher risk of migration. Nevertheless, this increased migration risk does not appear to significantly impact stricture resolution rates. (3) Within the first three years after endoscopic intervention, recurrence rates have been observed to be similar for both stent types. (2)
Endoscopic therapy remains the first-line strategy for managing anastomotic strictures, with comparable effectiveness in preventing stricture recurrence between progressively placed multiple plastic stents and fully covered self-expanding metal stents. Close clinical and imaging follow-up during the first three years after intervention is critical for the timely detection and management of potential recurrences.
- Jarlot-Gas C, Muscari F, Mokrane FZ, Del Bello A, Culetto A, Buscail E, et al. Management of anastomotic biliary stricture after liver transplantation and impact on survival. HPB. 2021 Aug;23(8):1259–68.
- Pinheiro LW, Martins FP, Ferrari AP, Tafner E, De Paulo GA, Della Libera E. Long-term outcomes of post-transplant biliary anastomotic strictures: Endoscopic therapy with plastic and metal stents. World J Gastrointest Endosc [Internet]. 2025 Jun 16 [cited 2025 Nov 4];17(6). Available from: https://www.wjgnet.com/1948-5190/full/v17/i6/103183.htm
- Visconti TA de C, Bernardo WM, Moura DTH, Moura ETH, Gonçalves CVT, Farias GF, et al. Metallic vs plastic stents to treat biliary stricture after liver transplantation: a systematic review and meta-analysis based on randomized trials. Endosc Int Open. 2018 Aug;6(8):E914–23.