See other cases
Benign post-operatory esophago-gastric anastomotic stenosis
A 59-year-old male with a history of surgery for esophageal neoplasm in 2019 (Ivor Lewis technique: intrathoracic esophago-gastric anastomosis), presents complaining of mixed dysphagia. In the previous two years the patient underwent multiple endoscopic dilations with multi-diameter balloon and Savary bougies. Repeated biopsies of the anastomosis did not exhibit any sign of malignancy.
His clinical examination and blood work did not reveal any abnormalities.
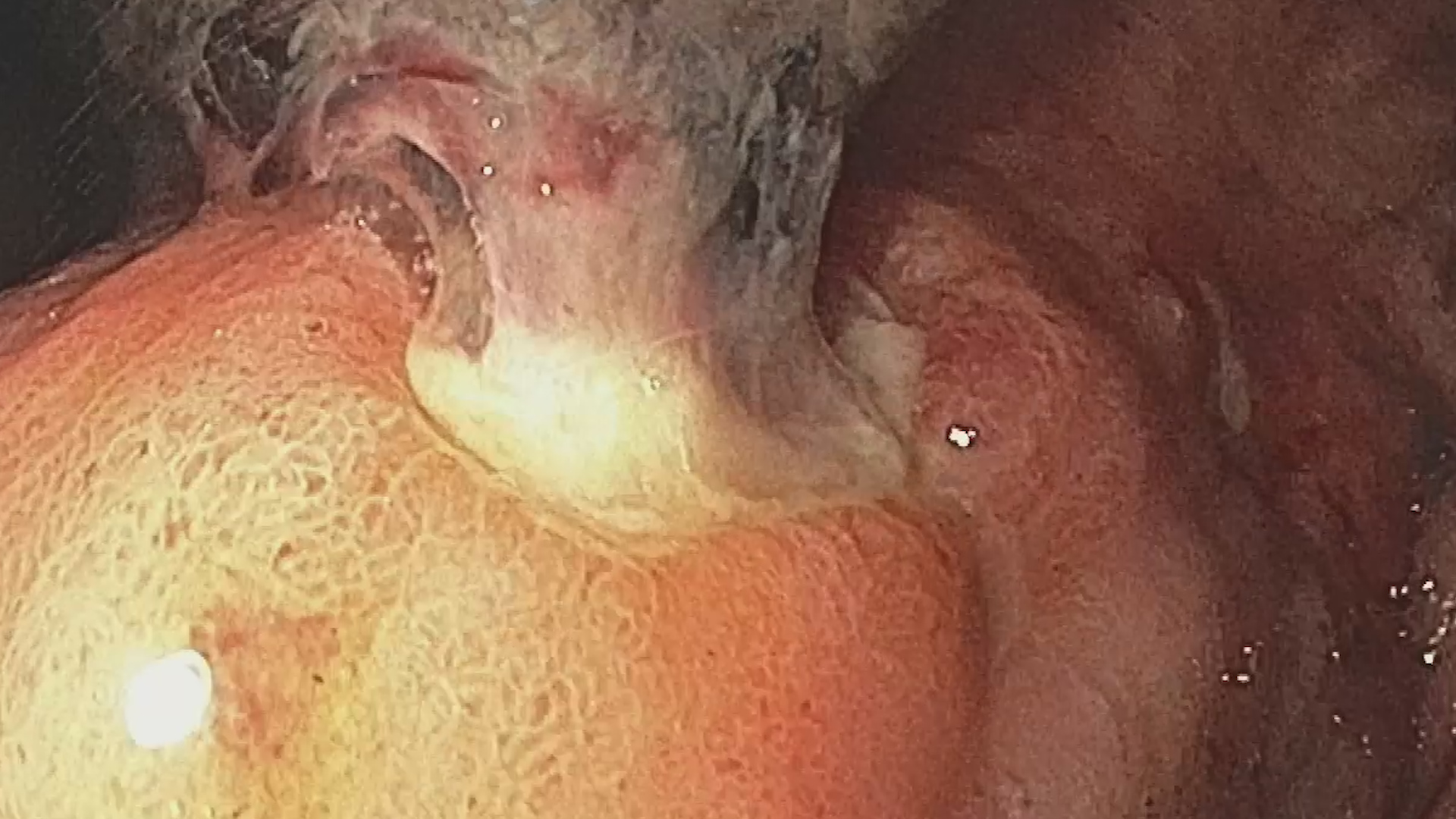
A barium swallow examination was requested which revealed a dilated remnant of esophagus along with a tight esophago-gastric anastomosis and normal gastric stump (Fig. 1) and duodenum.
The full-body CT scan with contrast did not show any abnormal adenopathy or distant metastasis.
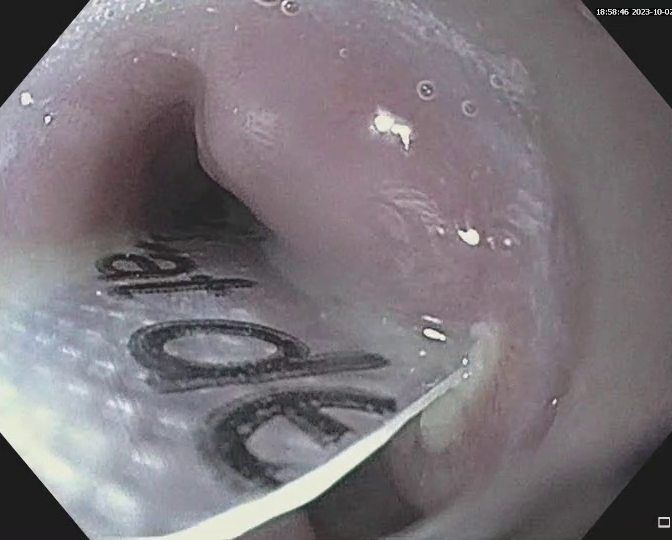
Upper GI endoscopy was performed and unveiled an unpassable esophago-gastric anastomotic stricture at approximately 24 cm from the incisors (Fig. 2).
Benign post-operatory esophago-gastric anastomotic stenosis.
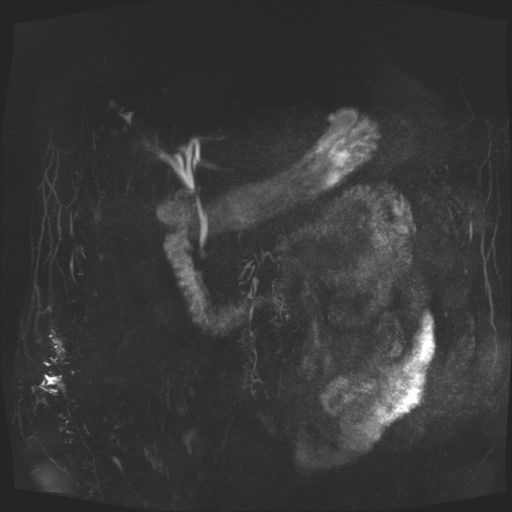
Incisional therapy with needle knife (Fig 3) was performed followed by placement of a 22/10 mm fully covered esophageal stent. Barium swallow with non-ionic contrast at 24 h after the procedure revealed a calibrated anastomotic stenosis with appropriate placement of the esophageal stent. No fistula tract was observed. (Fig 4). The patient was discharged the next day. At 4 weeks after the placement of the esophageal stent the patient was admitted for its extraction. Upper GI endoscopy revealed a calibrated esophago-gastric anastomosis.
The benign post-operatory esophago-gastric anastomosis has multiple options for endoscopic treatment:
- Multi-diameter balloon and Savary bougie dilation represent the mainstray procedures for benign post-operatory anastomotic stenosis.
- Corticosteroid injection in 4 quadrants after endoscopic dilatation can be used but with limited efficacy.
- Incisional therapy with needle knife in different quadrants or placement of totally covered esophageal stents for stenosis calibration show promising results.
This case illustrates the endoscopic, radiological appearance and the endoscopic management of a tight benign post operatory esophago-gastric anastomotic stenosis, refractory to endoscopic multi-diameter balloon and Savary bougie dilation.
- Peter D. Siersema. Management of refractory benign esophageal strictures. Gastroenterology Hepatology 2018 Mar; 14 (3):189-191
- Simon M. Everett. Endoscopic management of refractory benign oesophageal strictures. The AdvGastrointestEndosc 2019 Jan-Dec12: 2631774519862134