See other cases
A rare cause of gastritis: necrotizing ischemic gastritis
A 83-year-old patient with multiple comorbidities (heart failure NYHA class IV, triple vessel disease, permanent cardiac defibrillator, high blood pressure, persistent AF with anticoagulation (NOAC), arteriosclerosis obliterans, HCV cirrhosis) presented to the emergency room for multiple loose, watery stools initially, later melena, with onset about 24 hours earlier.
Clinical: altered general condition but hemodynamically stable, pallor, diffusely painful abdomen, without signs of peritoneal irritation.
Biological: important inflammatory syndrome: leukocytes = 32 000/mm3, Hgb=11.2 g/dl, platelets = 137000/mm3; CRP = 160 mg/l; procalcitonin>100 ng/ml
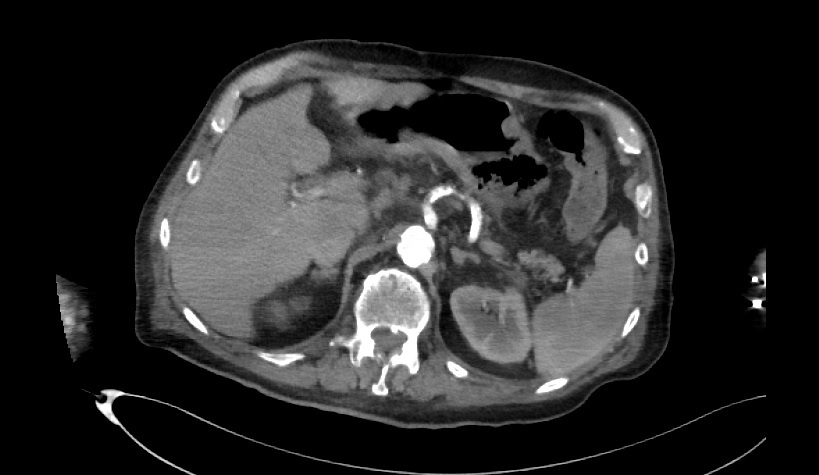
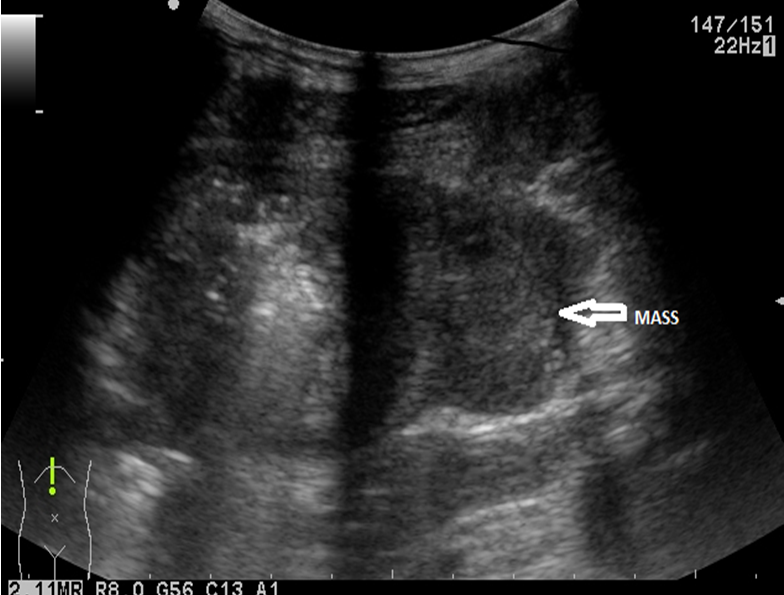
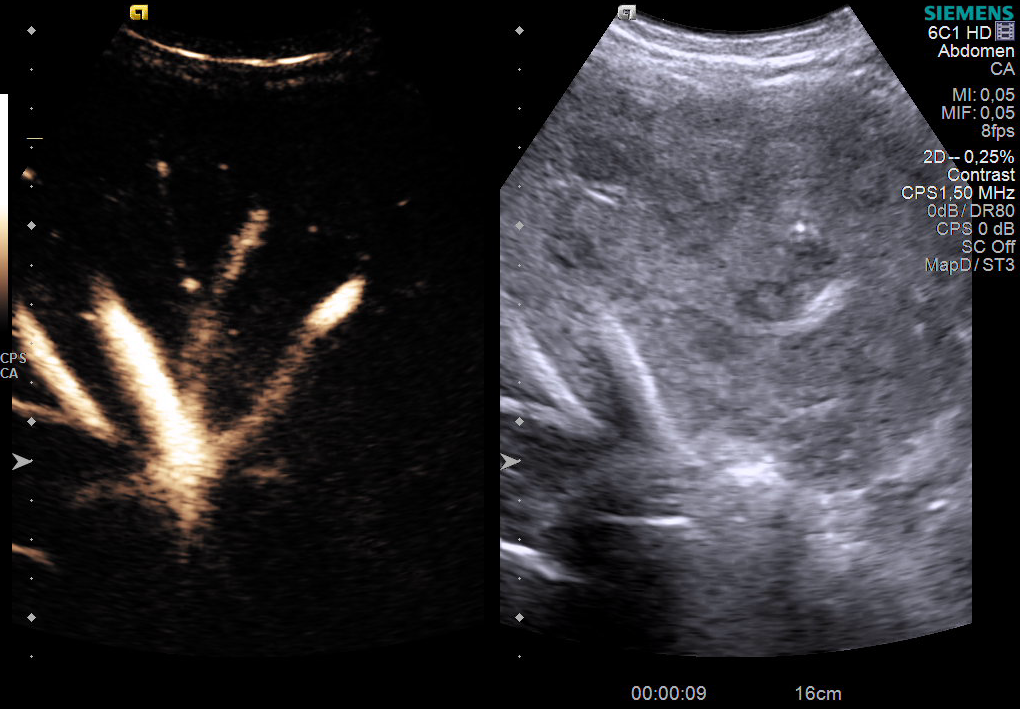
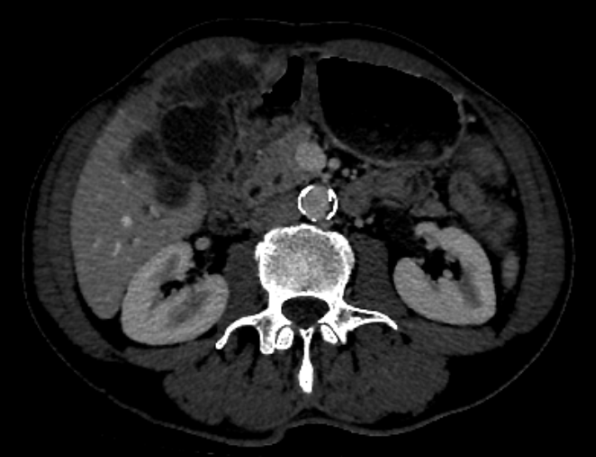
An abdominal CT scan is initially performed: at the level of the gastric fornix wall: a voluminous ulceration, intramural gas, suggesting ischemia and necrosis; without perforation; left portal venous gas; multiple calcified atherosclerotic plaques at the level of the thoraco-abdominal aorta and all its emergents; preservation of the permeability of the celiac trunk, mesenteric arteries and their emergences; small amount of intra- and retroperitoneal fluid at pelvic level (maximum 55 mm); prostatic abscess of approx. 68/63/86 mm.
Day 1:
- Empiric systemic antibiotic therapy is initiated (iv Meronem + Metronidazole) and Vancomycin per os (suspected CD infection) + PPI on infusion
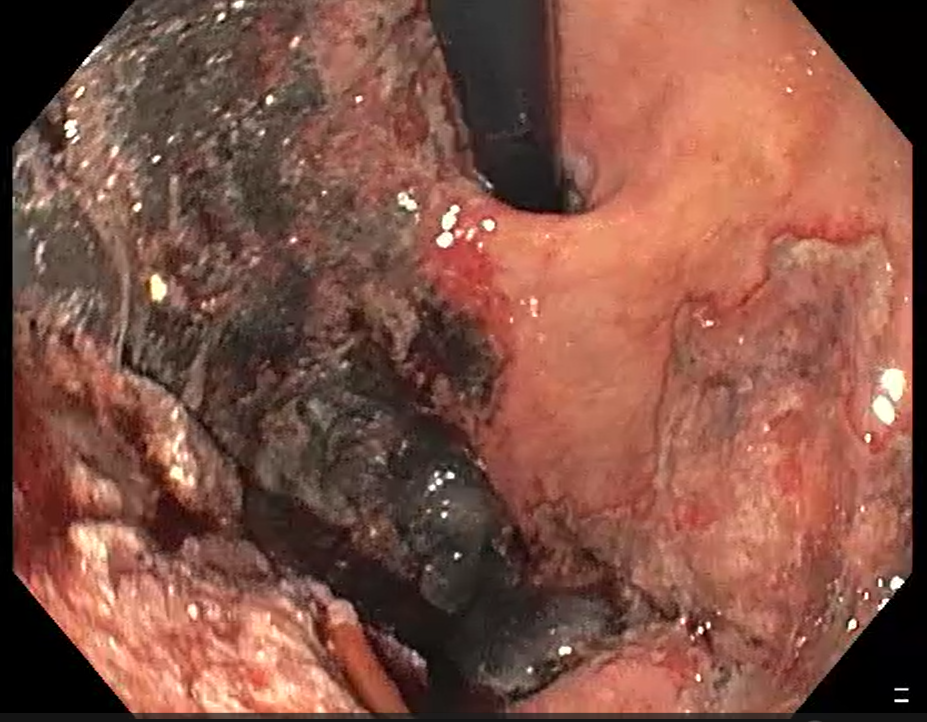
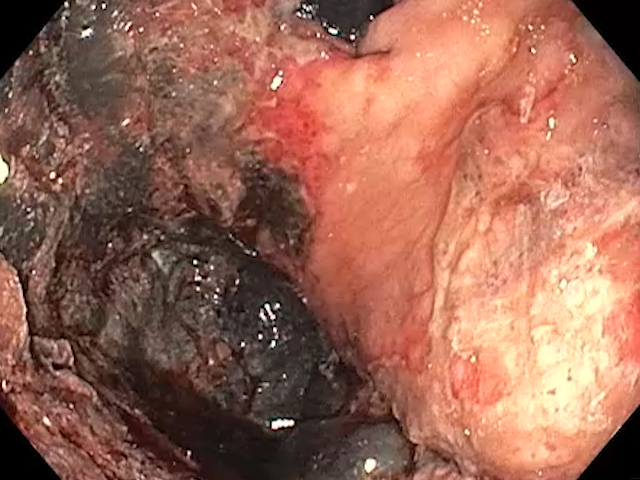
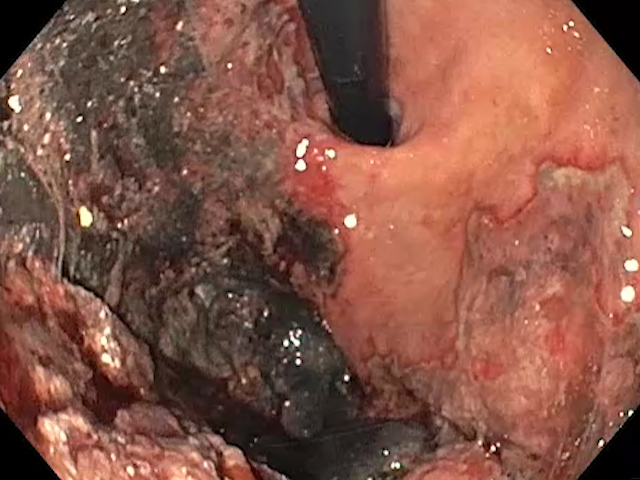
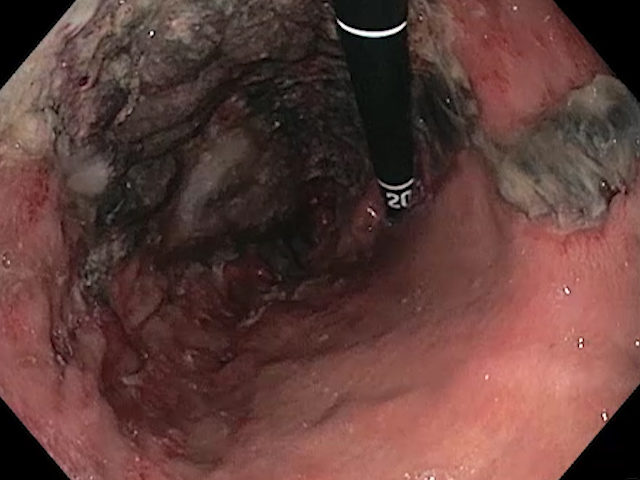
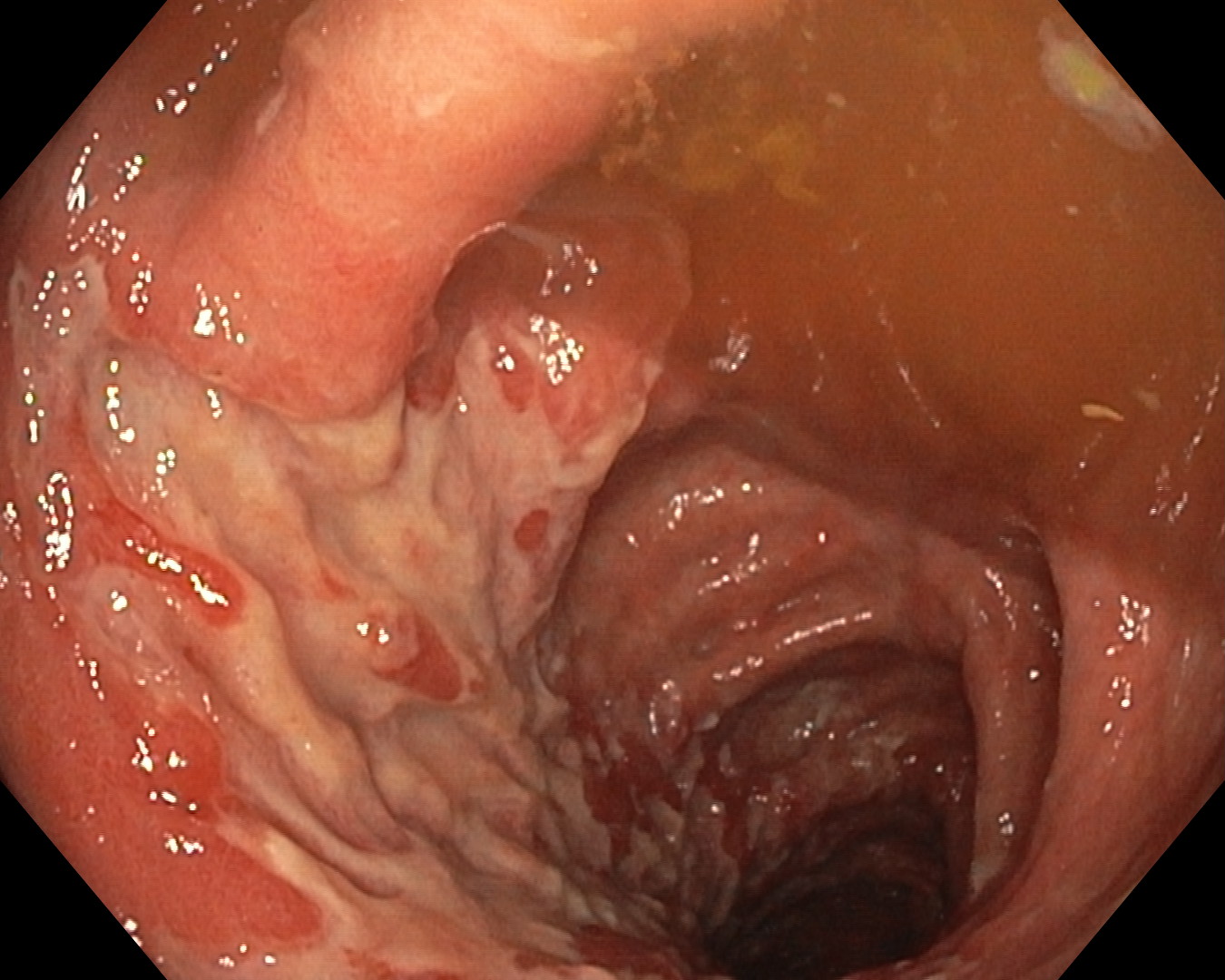
- 12 hours after admission, upper GI endoscopy is performed: esophagitis grade C; stomach lined entirely with digested blood; ulcero-necrotic congestive mucosa areas suggestive of ischemic gastritis. At the level of the fornix, an extended area highly suggestive of necrosis of the gastric wall with adherent clots – biopsy was performed. At the level of the pylorus, multiple confluent necrotic ulcerations. Bulb with a giant FORREST III; DII with atrophic mucosa.
Day 7:
- Biologically, a clear improvement in sepsis is noted: leukocytes = 12 100/mm3, Hgb = 9.9 g/dl, platelets = 244 000/mm3; CRP = 15 mg/l; procalcitonine = 0.6 ng/ml
- Clinically, the patient’s general condition is slightly improved.
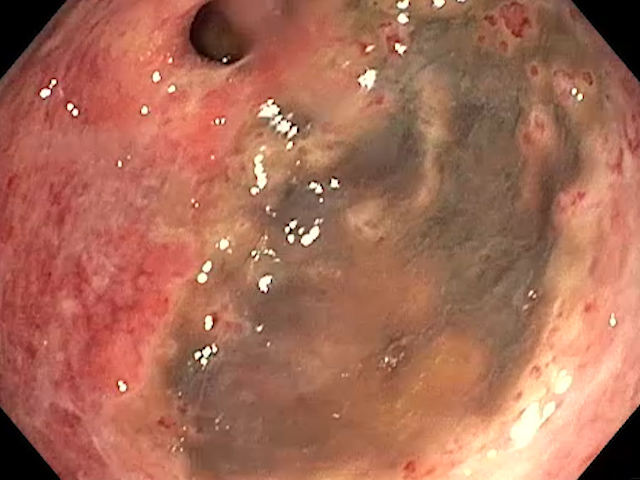
- Second upper GI endoscopy: esophagitis in regression, the fornix appear similar to the previous exam: extensive area of necrosis, extremely friable mucosa; at the antral level, slightly improved appearance – significant hyperemia. Duodenal bulb: the previously described ulcer is cicatrized, reduced in size. Duodenum 2: normal aspect.
- Second CT scan: slight regression of intramural gas at the fundus; without perforation. The disappearance of left portal intraluminal air. Slight dimensional regression of the prostatic abscess, with irregular walls and internal septa, with diameters of approximately 55/45/66 mm.
Biopsy result: gastric mucosa showing diffuse ulceration with fibrino-necrotic and leukocyte detritus, with a reduced number of remaining foveolar/glandular structures, with an atrophic appearance (“withered”); areas of ischemic necrosis.
Under antibiotic treatment and corrective treatment of the electrolyte imbalances, the patient’s evolution was slowly favorable. He did not repeat melena during the hospitalization.
Necrotizing ischemic gastritis.
Necrotizing gastritis is a rare pathology since the stomach is an intensely vascularized organ. Early detection is difficult, with high mortality of 50-80%. Cases can be due to atherosclerosis, embolism, venous thrombosis, volvulus, but they can also be due to infectious gastritis. The pathogenesis of the condition, however, is not completely elucidated. Risk factors are old age and patients with vascular risk, such as renal failure and diabetes. In our case, the patient was elderly and had multiple comorbidities, despite the anticoagulant treatment he was following at home.
The characteristic symptoms include abdominal pain and gastrointestinal bleeding, as in the case presented. Early diagnosis and treatment of ischemic gastritis is difficult because the diagnosis requires upper GI endoscopy when symptoms appear; therefore, early detection by other imaging modalities is preferable. Hence, the first endoscopy performed in our case was 12 hours after admission, after initiation of treatment. CT scan changes are characteristic and include parietal thickening and emphysema, fluid retention, rarely objectifying vascular occlusion. Upper GI endoscopy reveals multiple ulcerations and ischemic changes.
In selected cases, necrotizing gastritis is treated surgically, especially in case of perforation, volvulus or severe ischemia that do not respond to medical therapy. But surgical treatment is often difficult due to the altered general condition of the patient.
Early diagnosis of necrotizing ischemic gastritis increases the chances of survival, especially if therapy is initiated quickly and the patient’s general condition allows for aggressive therapeutic intervention.
- Murugesan RKS, Annamalai S, Prabakar J, Ross K. A Rare Case of Acute Necrotizing Gastritis. Indian J Surg. 2021 May 17;83(Suppl 3):1-4.
- Tomishima K, Sato S, Amano N, Murata A, Tsuzura H, Kanemitsu Y, Shimada Y, Iijima K, Genda T, Wada R, Nagahara A. A case of ischemic gastroduodenal disease in a patient who was receiving hemodialysis treatment that was managed by conservative treatment. Clin J Gastroenterol. 2018;11:386–390.
- Guniganti P, Bradenham CH, Raptis C, Menias CO, Mellnick VM. CT of Gastric Emergencies. Radiographics. 2015;35:1909–1921.