See other cases
A patient with history of chronic kidney disease, bilateral nephrostomies, and a postero-inferior acute myocardial infarction three months ago, who was diagnosed five months ago with a locally invasive rectosigmoid tumor and secondary liver metastases, presents with subocclusive syndrome.
Clinical: impaired general condition, hemodynamically and respiratory stable, distended abdomen, with diffuse tenderness present spontaneously and elicited on palpation, without signs of peritoneal irritation, absence of intestinal transit for 4 days, unable to tolerate oral intake, persistent emetic syndrome, palpable hepatomegaly 5–6 cm below the costal margin.
Biological: moderate normochromic normocytic anemia (Hb = 8 g/dl), inflammatory syndrome, leukocytosis = 16,000/mm³ with neutrophilia, C-reactive protein = 200 ng/ml, procalcitonin = 2.7 ng/mg.
Contrast-enhanced computed tomography of the abdomen and pelvis revealed:
• Locally invasive, stenosing rectosigmoid tumor measuring 76×90×100 mm (transverse/anterior-posterior/cranio-caudal)
• Hepatic metastases and supradiaphragmatic lymphadenopathy
• Small amount of intra- and extraperitoneal fluid in the abdomen and pelvis
• Incompletely obstructive bilateral pulmonary thromboembolism
• Left iliofemoral venous thrombosis
Histopathological examination revealed colonic adenocarcinoma NOS with tubulovillous and cribriform architecture, infiltrative growth and areas of ulceration. Immunohistochemistry showed moderately differentiated intestinal adenocarcinoma, panTRK negative, K-RAS, N-RAS, and BRAF wild type, microsatellite stable.
Oncological treatment with FOLFOX chemotherapy regimen was initiated, and palliative endoscopic placement of a colonic stent using the stent-in-stent technique was decided.
Endoscopic Procedure
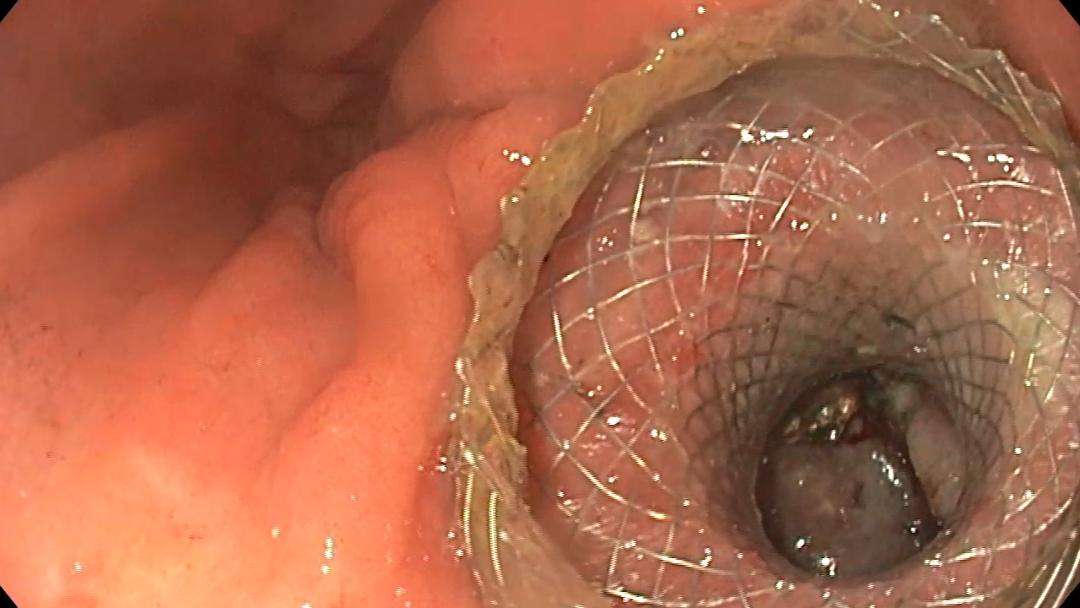
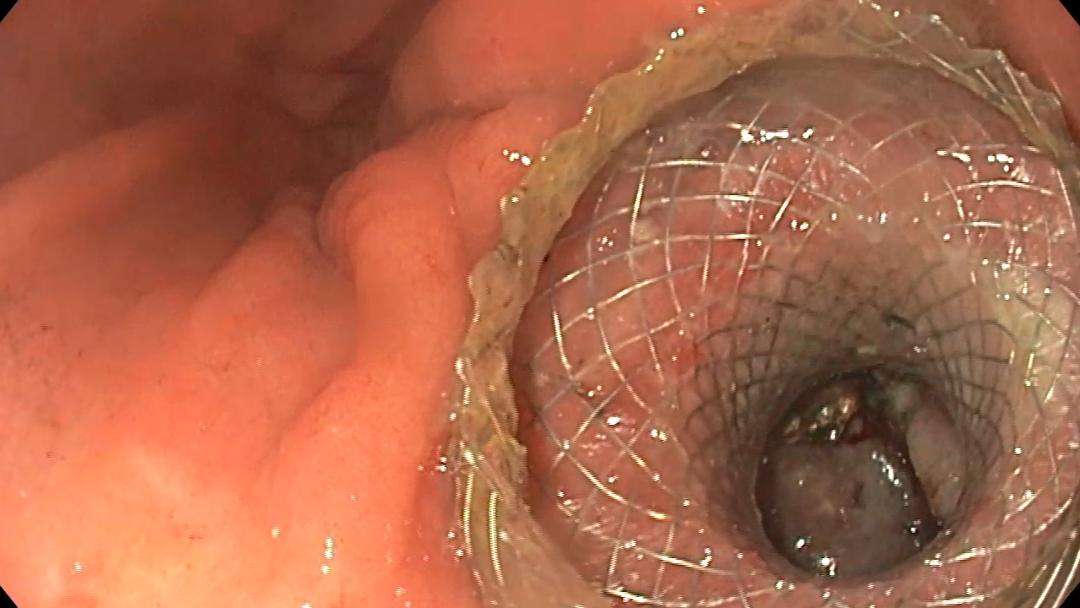
Rectosigmoidoscopy revealed a large stenosing tumor mass of the rectum and sigmoid colon, friable, approximately 10 cm in length, starting 8 cm from the anal verge. The endoscope was advanced through the tumor up to the proximal edge, a JagWire 0.035-inch guidewire was placed using a sphincterotome (Figure 1), and contrast was injected for fluoroscopic localization. The first self-expanding metal stent (SEMS) (Boston Scientific WallFlex 90/22 mm, uncovered) was placed at the proximal portion of the tumor (Figure 2), with the distal end left intratumoral (Figures 3 and 4). A second identical stent (Boston Scientific WallFlex 90/22 mm, uncovered) was inserted with its proximal end inside the first stent and its distal end at the level of the rectal ampulla, distal to the tumor mass.
A non-contrast CT scan performed the next day confirmed the stents in situ, with no upstream sigmoid dilation (Figures 5 and 6).
Stenosing rectosigmoid adenocarcinoma. Palliative stenting using stent-in-stent technique.
In patients with advanced metastatic disease, the management of malignant colonic obstruction is primarily palliative, aiming for rapid decompression, symptom relief, and avoidance of emergency surgery that may result in a stoma. In this context, self-expanding metal stents (SEMS) are an effective therapeutic option, with clinical and technical success rates exceeding 90%, as reported in the literature (1).
The unique aspect of this case was the need to use the stent-in-stent technique. The tumor was approximately 10 cm long, exceeding the length of a standard single stent. Sequential placement of two SEMS, with intraluminal overlap, allowed for complete coverage of the stenosis, adequate patency, and restoration of intestinal transit. This approach is also mentioned in the literature as useful in extensive lesions, as well as in cases of re-obstruction due to tumor ingrowth/overgrowth or stent migration (2).
Major complications of colonic stenting include: perforation, migration, pain, bleeding, re-obstruction. Stent type selection (covered vs. uncovered) influences the risk profile: uncovered stents carry a higher risk of tumor ingrowth and late re-obstruction, covered stents have a higher migration risk. In this case, uncovered stents were used, providing better anchorage and lower migration risk, at the cost of increased potential for late tumor-related re-obstruction (3).
In conclusion, using the stent-in-stent technique allowed efficient control of subocclusive syndrome in this palliative context, avoiding major surgery and improving the patient’s quality of life.
1. Walayat S, Johannes AJ, Benson M, Nelsen E, Akhter A, Kennedy G, et al. Outcomes of colon self–expandable metal stents for malignant vs benign indications at a tertiary care center and review of literature. World J Gastrointest Endosc. 2023; 15(4) :309–18.
2. Kaplan J. Enteral stents for the management of malignant colorectal obstruction. World J Gastroenterol. 2014; 20(37): 13239.
3. Han SH, Lee JH. Colonic Stent-Related Complications and Their Management. Clin Endosc. 2014; 47(5): 415.
See other cases